Abstract
A persistent finding is that assisted reproductive technology (ART) is associated with compromised birth outcomes, including higher risks for prematurity, low birthweight, and congenital malformations, even among singletons. Over the past decade, our research group, the Massachusetts Outcome Study of Assisted Reproductive Technology (MOSART), has evaluated pregnancy and birth outcomes among three groups of women, those women treated with ART, those with indicators of subfertility but without ART treatment, and fertile women. We have also explored the influence of infertility-related diagnoses on outcomes for women and infants. Over the course of our research, we have changed our perspective from an original focus on ART treatment parameters as the primary cause of excess morbidity to one centered instead on the underlying infertility-related diagnoses. This paper summarizes the research findings from our group that support this change in focus for infertility-based research from a primary emphasis on ART treatment to greater attention to the contribution of preexisting pathology underlying the infertility and suggests directions for future analyses.
Similar content being viewed by others
References
Fauser BCJM, Devroey P, Diedrich K, Balaban B, Bonduelle M, de Waal HA D-v, et al. Health outcomes of children born after IVF/ICSI: a review of current expert opinion and literature. Reprod BioMed Online. 2014;28:162–82.
Helmerhorst FM, Perquin DAM, Donker D, Keirse JNC. Perinatal outcome of singletons and twins after assisted conception: a systematic review of controlled studies. BMJ. 2004;328:261–6.
Henningsen AKA, Pinborg A, Lidegaard Ø, Vestergaard C, Forman JL, Andersen AN. Perinatal outcome of singleton siblings born after assisted reproductive technology and spontaneous conception: Danish national sibling-cohort study. Fertil Steril. 2011;95:959–63.
Källén B, Finnström O, Lindam A, Nilsson E, Nygren K-G, Otterblad PO. Congenital malformations in infants born after in vitro fertilization in Sweden. Birth Defects Res (Part A). 2010;88:137–43.
Källén B, Finnström O, Lindam A, Nilsson E, Nygren K-G, Olausson PO. Trends in delivery and neonatal outcome after in vitro fertilization in Sweden: data for 25 years. Hum Reprod. 2010;25:1026–34.
Sutcliffe AG, Ludwig M. Outcome of assisted reproduction. Lancet. 2007;370:351–9.
Barlow DH. The children of assisted reproduction—the need for an ongoing debate. Hum Reprod. 2002;17:1133–4.
Brison DR, Roberts SA, Kimber SJ. How should we assess the safety of IVF technologies? Reprod BioMed Online. 2013;27:710–21.
Gosden R, Trasler J, Lucifero D, Faddy M. Rare congenital disorders, imprinting genes, and assisted reproductive technology. Lancet. 2003;361:1975–7.
Niemitz EL, Feinberg AP. Epigenetics and assisted reproductive technology: a call for investigation. Am J Hum Genet. 2004;74:599–609.
President’s Council on Bioethics. Reproduction and responsibility: the regulation of new biotechnologies. Washington, DC, 2004.
Declercq ER, Belanoff C, Diop H, Gopal D, Hornstein MD, Kotelchuck M, et al. Identifying women with indicators of subfertility in a statewide population database: operationalizing the missing link in ART research. Fertil Steril. 2014;101:463–71.
Luke B, Stern JE, Kotelchuck M, Declercq E, Anderka M, Diop H. Birth outcomes by infertility diagnosis: analyses of the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). Journal of Reproductive Medicine (2015b).
Stern JE, Luke B, Tobias M, Gopal D, Hornstein MD, Diop H. Adverse pregnancy and birth outcomes by infertility diagnoses with and without ART treatment. Fertil Steril. 2015;103:1438–45.
Basso O, Olsen J. Subfecundity and neonatal mortality: longitudinal study within the Danish national birth cohort. BMJ. 2005;330:393–4.
Cooper AR, O’Neill KE, Allsworth JE, Jungheim ES, Odibo AO, Gray DL, et al. Smaller fetal size in singletons after infertility therapies: the influence of technology and the underlying infertility. Fertil Steril. 2011;96:1100–6.
Kondapalli LA, Perales-Puchalt A. Low birth weight: is it related to assisted reproductive technology or underlying infertility? Fertil Steril. 2013;99:303–10.
Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Söderström-Anttila V, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013;19:87–104.
Raatikainen K, Kuivasaari-Pirinen P, Hippeläinen M, Heinonen S. Comparison of the pregnancy outcomes of subfertile women after infertility treatment and in naturally conceived pregnancies. Hum Reprod. 2012;27:1162–9.
Romundstad LB, Romundstad PR, Sunde A, von Düring V, Skjærven R, Gunnell D, et al. Effects of technology or maternal factors on perinatal outcome after assisted fertilization: a population-based cohort study. Lancet. 2008;372:737–43.
Luke B, Stern JE, Kotelchuck M, Declercq E, Anderka M, Diop H. Birth outcomes by infertility treatment: analyses of the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). Journal of Reproductive Medicine (2015a).
Luke B, Brown MB, Grainger DA, Stern JE, Klein N, Cedars M. The effect of early fetal losses on singleton assisted-conception pregnancy outcomes. Fertil Steril. 2009;91:2578–85.
Luke B, Brown MB, Grainger DA, Stern JE, Klein N, Cedars M. The effect of early fetal losses on twin assisted-conception pregnancy outcomes. Fertil Steril. 2009;91:2586–92.
Luke B, Stern JE, Kotelchuck M, Declercq ER, Hornstein MD, Gopal D, et al. Adverse pregnancy outcomes after in vitro fertilization: effect of number of embryos transferred and plurality at conception. Fertil Steril. 2015;104:79–86.
Luke B, Brown MB, Stern JE, Grainger DA, Klein N, Cedars M. Effect of embryo transfer number on singleton and twin implantation pregnancy outcomes after assisted reproductive technology (ART). J Reprod Med. 2010;55:387–94.
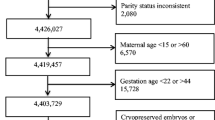
Declercq E, Luke B, Belanoff C, Cabral H, Diop H, Gopal D, et al. Perinatal outcomes associated with assisted reproductive technology: the Massachusetts outcomes study of assisted reproductive technologies (MOSART). Fertil Steril. 2015;103:888–95.
Diop H, Cabral H, Gopal D, Belanoff C, Declercq ER, Kotelchuck M, Luke B, Stern JE. Child health after assisted reproductive technology: association of ART with enrollment in early intervention programs. Pediatrics (2015).
Declercq E, Stern JE, Luke B, Cabral H, Gopal D, Belanoff C, Diop H, Kotelchuck M. Maternal postpartum hospitalization following ART births. Epidemiology 2015;26:e64–65.
Center for Disease Control and Prevention, American Society for Reproductive Medicine, and Society for Assisted Reproductive Technology, 2012 Assisted Reproductive Technology Success Rates: National Summary and Fertility Clinic Reports. Washington, DC: US Dept. of Health and Human Services; 2014.
Martin JA, Hamilton BE, Ventura SJ, Osterman MJK, Curtin SC, Births MTJ. Final data for 2013. Nat Vital Stat Rep. 2015;64(1):1–87.
Luke B, Brown MB, Wantman E, Stern JE, Baker VL, Widra E, et al. Application of a validated prediction model for in vitro fertilization: comparison of live birth rates and multiple birth rates with one embryo transferred over two cycles versus two embryos in one cycle. Am J Obstet Gynecol. 2015;212(676):e1–7.
Liberman RF, Stern JE, Luke B, Reefhuis J, Anderka M. Maternal self-report of assisted reproductive technology Use in the national birth defects prevention study: validation using fertility clinic data. (Research letter). Epidemiology. 2014;25:773–5.
Boulet SL, Schieve LA, Nannini A, et al. Perinatal outcomes of twin births conceived using assisted reproduction technology: a population-based study. Hum Reprod. 2008;23(8):1941–8.
Mneimneh AS, Boulet SL, Sunderam S, et al. States monitoring assisted reproductive technology (SMART) collaborative: data collection, linkage, dissemination, and use. J Womens Health. 2013;22:571–7.
Tepper NK, Farr SL, Cohen BB, Nannini A, Zhang Z, Anderson JE, et al. Singleton preterm birth: risk factors and association with assisted reproductive technology. Matern Child Health J. 2012;16(4):807–13.
Zhang Y, Cohen B, Macaluso M, et al. Probabilistic linkage of assisted reproductive technology information with vital records, Massachusetts 1997–2000. Matern Child Health J. 2012;16(8):1703–8.
Acknowledgments
The project described was supported by Award Numbers R01HD064595 and R01HD067270 from the National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule This review presents evidence that infertility research should focus on underlying pathology rather than treatment parameters as the major cause of compromised outcomes.
Rights and permissions
About this article
Cite this article
Luke, B., Stern, J.E., Hornstein, M.D. et al. Is the wrong question being asked in infertility research?. J Assist Reprod Genet 33, 3–8 (2016). https://doi.org/10.1007/s10815-015-0610-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-015-0610-3