Abstract
Purpose
The objective of this study was to evaluate a panel of three sperm function tests; tests known to assess different aspects of sperm functionality and genomic integrity, the: 1) Sperm DNA Accelerated Decondensation (SDADTM) Test, 2) Sperm DNA Decondensation (SDDTM) Test, and 3) Sperm Penetration Assay (SPA), determining if positive and negative test scores correlated with failed and successful ICSI outcomes, respectfully.
Methods
A prospective, double blinded, cohort study was performed. One study sample (ejaculated semen) was collected by each of the 60 male partners of the 60 couples enrolled in the study; males whose female partners were found to have no major female factor issues. The sperm from each male was analyzed in the SPA, and SDAD and SDD Tests, and used for ICSI (1 ICSI cycle per couple).
Results
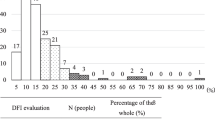
The ICSI cycle pregnancy rate for this study was 50 %, with a delivery rate = 40 % (n = 60 ICSI cycles). The SPA and SDD Test scores did not significantly predict ICSI outcome when used as stand-alone tests (p> > 0.05). However, when the SPA and SDD Test scores were used together, ICSI outcomes for a subgroup of 10 (16.7 %) males, were significantly predicted (p = 0.03), with 1 live birth, and 9 negatives where the transferred embryos did not implant. In total, 38.4 % of the couples in this study were found to have a very poor chance for a successful ICSI cycle.
Conclusion
SDAD Test scores alone, and SPA and SDD Test scores used together, significantly predicted failed ICSI outcomes. This indicates that the scores obtained when analyzing patients’ sperm using a panel of sperm function tests; specifically, the SPA, and SDAD and SDD Tests, can be used to identify infertile couples who should not be directed to ICSI.




Similar content being viewed by others
References
Agarwal A, Said TM. Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum Reprod Update. 2003;9:331–45.
Agarwal A. Current and future perspectives on intracytoplasmic sperm injection: a critical commentary. Reprod BioMed Online. 2007a;15:719–27.
Agarwal A, Prabakaran S. Clinical relevance of oxidative stress in patients with male factor infertility; evidence-based analysis. Am Urol Assoc Updat Ser. 2007b;26:1–11.
Agarwal A, Deepinder F, Sharma RK, Ranga G, Li J. Effect of cell phone usage on semen analysis in men attending infertility clinic: an observational study. Fertil Steril. 2008;89:124–8.
Aitken RL, Buckingham D, West K, Wu FC, Zikopoulos K, Richardson DW. Differential contribution of leucocytes and spermatozoa to the high levels of reactive oxygen species recorded in the ejaculates of oligozoospermic patients. J Reprod Fertil. 1992;94:451–462.
Aitken RJ, Gordon E, Harkiss D, Twigg JP, Milne P, Jennings Z, et al. Relative impact of oxidative stress on the functional competence and genomic integrity of human spermatozoa. Biol Reprod. 1998;59:1037–46.
Aitken RJ. Whither must spermatozoa wander? The future of laboratory seminology. Asian J Androl. 2010;12:99–103.
Anderson AN, Goossens V, Ferraretti AP, et al. Assisted reproductive technology in Europe. Hum Reprod. 2008;23:1158–76.
Bar-Charma N, Lamb DJ. Evaluation of sperm function. What is available in the modern andrology laboratory. Urol Clin N Am. 1994;21:433–46.
Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–12.
Bonde JPE, Ernst E, Jensen TK, et al. Relation between semen quality and fertility: a population-based study of 430 first-pregnancy planners. Lancet. 1998;352:1172–7.
Brown DB, Blake E, Wolgemuth D, Gordon K, Ruddle F. Chromatin decondensation and DNA synthesis in human sperm activated in vitro by using Xenopus laevis egg extracts. J Exp Zool. 1987;242:215–31.
Brown DB, Nagamani M. Use of Xenopus laevis frog egg extract in diagnosing human male unexplained infertility. Yale J Biol Med. 1992;65:29–38.
Brown DB, Hayes EJ, Uchida T, Nagamani M. Some cases of human male infertility are explained by abnormal in vitro human sperm activation. Fertil Steril. 1995;64:612–22.
Brown DB, Gelman KM, Whitman-Elia GF, Witt MA, Kordus RJ, Roseff SJ. Comparing the sperm decondensation (SDDTM) and sperm DNA accelerated decondensation (SDADTM) tests’ capacity for identifying infertile males likely to benefit from anti-oxidant treatment. Fertil Steril. 2010;94 Suppl 4:S238.
Bungum M, Spano M, Humaidan P, Eleuteri P, Rescia M, Giwercman A. Sperm chromatin structure assay parameters measured after density gradient centrifugation are not predictive for the outcome of ART. Hum Reprod. 2008;23:4–10.
Bungum M (2012) Sperm DNA integrity assessment: a new tool in diagnosis and treatment of fertility. Obstet Gynecol Int doi:10.1155/2012/531042.
Cohen J, Edwards RG, Fehilly CB, Fishel SB, Hewitt J, Rowland G, et al. Treatment of male infertility by in vitro fertilization: factors affecting fertilizations and pregnancy. Acta Eur Fertil. 1984;15:455–65.
Davies MJ, Moore VM, Willson KJ, Van Essen P, Priest K, Scott H, et al. Reproductive technologies and the risk of birth defects. N Engl J Med. 2012;366:1803–13.
Dunson DB, Baird DD, Colombo B. Increased infertility with age in men and women. Obstet Gynecol. 2004;103:51–6.
Evenson DP, Darzynkiewicz Z, Melamed MR. Relation of mammalian sperm chromatin heterogeneity to fertility. Science. 1980;210:1131–3.
Evenson DP, Jost LK, Marshall D, et al. Utility of the sperm chromatin structure assay as a diagnostic and prognostic tool in the human fertility clinic. Hum Reprod. 1999;14:1039–49.
Gandlnl L, Lombardo F, Paoli D, et al. Full-term pregnancies achieved with ICSI despite high levels of sperm chromatin damage. Hum Reprod. 2004;19:1409–17.
Gomez E, Irvine DS, Aitken RJ. Evaluation of a spectrophotometric assay for the measurement of malondialdehyde and 4-hydroxyalkenals in human spermatozoa: relationships with semen quality and sperm function. Int J Androl. 1998;21:81–94.
Greco E., Lacobelli M, Ferrero S, Baroni E, Minasi MG, Ubaldi F, et al. ICSI in cases of sperm DNA damage: beneficial effect of oral anti-oxidant treatment. J Androl. 2005;20:2590–2594.
Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility and concentration in infertile and fertile men. N Engl J Med. 2001;345:1388–93.
Johnson AR, Bassham B, Lipshultz LI, Lamb DJ. Methodology for the optimized sperm penetration assay. In: Keel B, Webster B, editors. Handbook of the laboratory diagnosis and treatment of infertility. Boca Raton: CRC Press; 1990. p. 135–47.
Johnson A, Bassham B, Lipshultz LI, Lamb DJ. A quality control system for the optimized sperm penetration assay. Fertil Steril. 1995;64:832–7.
Kemal Duru N, Morshedi M, Oehninger S. Effects of hydrogen peroxide on DNA and plasma membrane integrity of human spermatozoa. Fertil Steril. 2000;74:287–91.
Lamb DJ. Semen analysis in 21st century medicine: the need for sperm function testing. Asian J Androl. 2010;12:64–70.
Larson KL, DeJonge CJ, Barnes AM, Jost LK, Evenson DP. Sperm chromatin structure assay parameters as predictors of failed pregnancy following assisted reproductive techniques. Hum Reprod. 2000;15:1717–22.
Larson-Cook KL, Brannian JD, Hansen KA, Kasperson KM, Aamold ET, Evenson DP. Relationship between the outcomes of assisted reproductive techniques and sperm DNA fragmentation as measured by the sperm chromatin structure assay. Fertil Steril. 2003;80:895–902.
Longo FJ, Kunkle M. Transformation of sperm nuclei upon insemination. Curr Top Dev Biol. 1978;12:149–84.
Matsumoto K, Nagata K, Miyaji-Yamaguchi M, Kikuchi A, Tsujimoto M. Sperm chromatin decondensation by template activating factor I through direct interaction with basic proteins. Mol Cell Biol. 1999;19:6940–52.
Merryman DC, Stringfellow SE, Yancey CA, Houserman VL, Long CA, Honea KL. Does in vitro fertilization (IVF) with intracytoplasmic sperm injection compensate for impaired sperm function as predicted by the sperm penetration assay (SPA)? Fert Steril. 2001;76 Suppl 1:S215.
Merryman DC, Stringfellow SE, Dalton KE, Houserman VL, Long CA, Honea KL. Sperm capacitation index (SCI) predicts pregnancy outcome with controlled ovarian hyperstimulation (COH) + intrauterine insemination (IUI). Fertil Steril. 2007;88 Suppl 1:S118–9.
Merryman DC, Rivnay B, Honea KL, Brown DB. Sperm DNA decondensation and sperm penetration assay with gradient preparation are not predictive of pregnancy outcome in in vitro fertilization cycles with intracytoplasmic sperm injection. Fertil Steril. 2007;88 Suppl 1:S380–1.
Misro MM, Choudbury L, Upreti K, Gautam D, Chaki SP, Mahaian AS, et al. Use of hydrogen peroxide to assess the sperm susceptibility to oxidative stress in subjects presenting a normal semen profile. Int J Androl. 2004;27:82–7.
Muratori M, Marchiani S, et al. Markers of human sperm functions in the ICSI era. Front Biosci. 2011;16:1344–63.
Natali A, Turek PJ. An assessment of new sperm tests for male infertility. Urology. 2011;77:1027–34.
Ochsendorft FR. Infections in the male genital tract and reactive oxygen species. Hum Reprod. 1999;5:399–420.
Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340:17–8.
Payne JF, Raburn DJ, Couchman GM, Price TM, Jamison MG, Walmer DK. Redefining the relationship between sperm deoxyribonucleic acid fragmentations as measured by the sperm chromatin structure assay and outcomes of assisted reproductive tehniques. Fertil Steril. 2005;84:356–64.
Philpott A, Leno GH, Laskey RA. Sperm decondensation in Xenopus egg cytoplasm is mediated by nucleoplasmin. Cell. 1991;65:569–78.
Philpott A, Leno GH. Nucleoplasmin remodels sperm chromatin in Xenopus egg extracts. Cell. 1992;69:759–67.
Rogers BJ, Van Campen H, Ueno M, Lambert H, Bronson R, Hanson RW. Analysis of human spermatozoa fertilizing ability using zona-free ova. Fertil Steril. 1979;32:664–70.
Sawyer DE, Brown DB. Diminished decondensation and DNA synthesis in activated sperm from rats treated with cyclophosphamide. Toxicol Lett. 2000;114:19–26.
Sawyer DE, Brown DB. The use of a in vivo sperm activation assay to detect chemically-induced damage of human sperm nuclei. Reprod Toxicol. 1995;9:351–7.
Sawyer DE, Hillman GR, Uchida T, Brown DB. Altered nuclar activation parametersof Rat sperm treated in vitro with chromatin damaging agents. Toxicol Sci. 1998;44:52–62.
Sigman M. Medications that impair male fertility. Sex Reprod Menopause. 2007;5:11–6.
Sigman M, Zini A. Semen analysis and sperm function assays: what do they mean? Semin Reprod Med. 2009;27:115–23.
Tirado EE, Sharma R, Sawyer DE, Awasthi YC, Brown DB. Effects of oxidative stress on human sperm activation. Fertil Steril. 2003;80 Suppl 3:S240.
Turkyilmaz Z, Gulen S, Sonmez K, Karabulut R, Dincer S, Can Basaklar A, et al. Increased nitric oxide is accompanied by lipid oxidation in adolescent varicocele. Int J Androl. 2004;27:183–7.
World Health Organization. Towards more objectivity in diagnosis and management of male infertility. Int J Androl. 1987;7:1–53.
World Health Organization. WHO laboratory manual for the examination and processing of human semen. 5th ed. Geneva: WHO Press; 2010.
Yanagimachi R, Yanagimachi H, Rogers BJ. The use of zona-free animal ova as a test system for the assessment of the fertilizing capacity of human spermatozoa. Biol Reprod. 1976;15:471–6.
Yanagimachi R. Mechanisms of fertilization in mammals. In: Mastrioni, Biggers J, editors. Fertilization and embryonic development. New York: Plenum Press; 1981. p. 81–187.
Yanagimachi R. Problems of sperm fertility: A reproductive biologist’s view. Systems Boil Reprod Med doi:10.3109/19396368.2010.507860.
The Practice Committee of the American Society for Reproductive Medicine. The clinical utility of sperm DNA integrity testing: a guideline. Fertil Steril. 2013;99:673–677.
Zini A, Meriano J, Kader K, Jarvi K, Laskin CA, Cadesky K. Potential adverse effect of sperm DNA damage on embryo quality after ICSI. Hum Reprod. 2005;20:3476–80.
Acknowledgments
The authors wish to acknowledge Olivera Vragovic, MBA (Research Manager, Dept. of Ob/Gyn, Boston University School of Medicine), for her invaluable help with the statistical analyses performed during the course of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
A Panel of physiologically relevant sperm function tests was shown to have significant clinical utility when used to predict ICSI outcome.
David B. Brown and Deborah C. Merryman contributed equally to this work.
Rights and permissions
About this article
Cite this article
Brown, D.B., Merryman, D.C., Rivnay, B. et al. Evaluating a novel panel of sperm function tests for utility in predicting intracytoplasmic sperm injection (ICSI) outcome. J Assist Reprod Genet 30, 461–477 (2013). https://doi.org/10.1007/s10815-013-9960-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-9960-x