Abstract
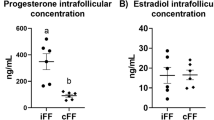
Purpose
Studies in bovine and porcine have indicated that melatonin (MT) could induce meiotic maturation of immature oocytes in vitro. The object of the current study was to investigate if MT could ameliorate human oocytes maturation during rescue in vitro maturation (IVM).
Methods
Two hundred seventy eight germinal vesicle (GV) oocytes and 451 (MI) metaphase I oocytes were vitrified, thawed and then matured in vitro. All the oocytes were randomly allocated into six groups in which the oocytes were cultured in medium supplemented with different concentrations of MT (0, 10−2, 1, 102, 104, 106 nM) and nuclear maturation was evaluated at 6 h, 12 h, 18 h, 24 h and 48 h of culture.
Results
The optimal MT concentration for both GV and MI oocytes was 1 nM. At 24 h of culture, nuclear maturation rate of MI oocytes cultured in 1 nM MT medium was significantly higher than other groups (P < 0.05); Nuclear maturation rate of GV oocytes cultured in 1 nM MT medium was also significantly higher than the control group (P < 0.05). On the other hand, decreased nuclear maturation rate was observed in the high MT concentration group (106 nM).
Conclusions
The current study demonstrated that low concentration of exogenous MT could ameliorate nuclear maturation of human oocyte during rescue IVM, while high concentration of MT presented negative effects.


Similar content being viewed by others
References
Balakier H, Sojecki A, Motamedi G, Librach C. Time-dependent capability of human oocytes for activation and pronuclear formation during metaphase II arrest. Hum Reprod. 2004;19(4):982–7.
Chan W, Ng T. Development of pre-implantation, mouse embryos under the influence of pineal indoles. J Neural Transm Gen Sect JNT. 1994;96(1):19–29.
Chian R-C, Lim J-H, Tan S-L. State of the art in in-vitro oocyte maturation. Curr Opin Obstet Gynecol. 2004;16(3):211.
Combelles CM, Gupta S, Agarwal A. Could oxidative stress influence the in-vitro maturation of oocytes? Reprod BioMed Online. 2009;18(6):864–80.
Edwards RG. Maturation in vitro of human ovarian oöcytes. Lancet. 1965;2(7419):926.
Gardner DK. Textbook of assisted reproductive techniques: laboratory and clinical perspectives. Taylor & Francis; 2001.
Guerin P, El Mouatassim S, Menezo Y. Oxidative stress and protection against reactive oxygen species in the pre-implantation embryo and its surroundings. Hum Reprod Updat. 2001;7(2):175–89.
Hardeland R. Atioxidative protection by melatonin. Endocrine. 2005;27(2):119–30.
Harvey AJ, Kind KL, Thompson JG. REDOX regulation of early embryo development. Reproduction. 2002;123(4):479–86.
Ishizuka B, Kuribayashi Y, Murai K, Amemiya A, Itoh MT. The effect of melatonin on in vitro fertilization and embryo development in mice. J Pineal Res. 2000;28(1):48–51.
Jahnke G, Marr M, Myers C, Wilson R, Travlos G, Price C. Maternal and developmental toxicity evaluation of melatonin administered orally to pregnant Sprague–Dawley rats. Toxicol Sci. 1999;50(2):271–9.
Legge M, Sellens MH. Free radical scavengers ameliorate the 2-cell block in mouse embryo culture. Hum Reprod. 1991;6(6):867–71.
Leon J, Acuña-Castroviejo D, Escames G, Tan DX, Reiter RJ. Melatonin mitigates mitochondrial malfunction. J Pineal Res. 2005;38(1):1–9.
McElhinny AS, Davis FC, Warner CM. The effect of melatonin on cleavage rate of C57BL/6 and CB A/Ca preimplantation embryos cultured in vitro. J Pineal Res. 1996;21(1):44–8.
Nogueira D, Sadeu JC, Montagut J. In vitro oocyte maturation: current status. In: Seminars in reproductive medicine. Thieme Medical Publishers; 2012. p. 199–213.
Pang S, Li L, Ayre E, Pang C, Lee P, Xu R, et al. Neuroendocrinology of melatonin in reproduction: recent developments. J Chem Neuroanat. 1998;14(3):157–66.
Papis K, Poleszczuk O, Wenta-Muchalska E, Modlinski JA. Melatonin effect on bovine embryo development in vitro in relation to oxygen concentration. J Pineal Res. 2007;43(4):321–6.
Rao GD, Chian R, Son W, Gilbert L, Tan S. Fertility preservation in women undergoing cancer treatment. Lancet. 2004;363(9423):1829–9.
Reiter RJ. Melatonin and human reproduction. Ann Med. 1998;30(1):103–8.
Reiter RJ. Melatonin: clinical relevance. Best Pract Res Clin Endocrinol Metab. 2003;17(2):273–85.
Reiter RJ, Tan D-X, Osuna C, Gitto E. Actions of melatonin in the reduction of oxidative stress. J Biomed Sci. 2000;7(6):444–58.
Shu Y, Gebhardt J, Watt J, Lyon J, Dasig D, Behr B. Fertilization, embryo development, and clinical outcome of immature oocytes from stimulated intracytoplasmic sperm injection cycles. Fertil Steril. 2007;87(5):1022–7.
Son W-Y, Chung J-T, Demirtas E, Holzer H, Sylvestre C, Buckett W, et al. Comparison of in-vitro maturation cycles with and without in-vivo matured oocytes retrieved. Reprod BioMed Online. 2008;17(1):59–67.
Son W-Y, Lee S-Y, Lim J-H. Fertilization, cleavage and blastocyst development according to the maturation timing of oocytes in in vitro maturation cycles. Hum Reprod. 2005;20(11):3204–7.
Takami M, Preston S, Toyloy V, Behrman HR. Antioxidants reversibly inhibit the spontaneous resumption of meiosis. Am J Physiol Endocrinol Metab. 1999;276(4):E684–8.
Tamura H, Takasaki A, Taketani T, Tanabe M, Kizuka F, Lee L, et al. The role of melatonin as an antioxidant in the follicle. J Ovarian Res. 2012;5(5):5.
Tan D-X, Manchester LC, Reiter RJ, Plummer BF, Limson J, Weintraub ST, et al. Melatonin directly scavenges hydrogen peroxide: a potentially new metabolic pathway of melatonin biotransformation. Free Radic Biol Med. 2000;29(11):1177–85.
Tan D, Reiter RJ, Manchester LC, Yan M, El-Sawi M, Sainz RM, et al. Chemical and physical properties and potential mechanisms: melatonin as a broad spectrum antioxidant and free radical scavenger. Curr Top Med Chem. 2002;2(2):181–97.
Tomás-Zapico C, Coto-Montes A. A proposed mechanism to explain the stimulatory effect of melatonin on antioxidative enzymes. J Pineal Res. 2005;39(2):99–104.
Veeck L, Wortham Jr J, Witmyer J, Sandow B, Acosta A, Garcia J, et al. Maturation and fertilization of morphologically immature human oocytes in a program of in vitro fertilization. Fertil Steril. 1983;39(5):594.
Wei D, Zhang C, Yin B, Wang P, Xie J, Song X, et al. Early cumulus cell removal could reduce the available embryo rate in human IVF. J Assist Reprod Genet. 2011;28(12):1213–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding information
The current study is funded by Major Program of Key Medical Science Project of Henan Province (Funding Number:201001010).
Capsule Low concentration of exogenous melatonin could ameliorate nuclear maturation of human oocyte during rescue IVM, while high concentration of melatonin presented negative effects.
Rights and permissions
About this article
Cite this article
Wei, D., Zhang, C., Xie, J. et al. Supplementation with low concentrations of melatonin improves nuclear maturation of human oocytes in vitro. J Assist Reprod Genet 30, 933–938 (2013). https://doi.org/10.1007/s10815-013-0021-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-013-0021-2