Abstract
Purpose
Vitreoretinal surgery in eyes with Boston type 1 keratoprosthesis (KPro) is challenging due to narrow optic of the KPro. This study analyzed the results of pars plana vitrectomy (PPV) using a wide-field imaging accessory, Resight®700 Fundus Viewing System (Carl Zeiss Meditec, Inc., Germany), for better intraoperative peripheral retinal imaging.
Methods
In this retrospective case series, KPro patients who underwent simultaneous or sequential PPV at Dokuz Eylul University Hospital between June 2010 and January 2020 were evaluated in terms of anatomic and visual prognoses, as well as KPro- and PPV-associated complications.
Results
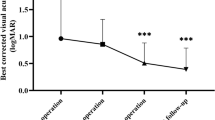
Among 9 KPro eyes that necessitated vitreoretinal surgery, 3 (33.3%) underwent simultaneous KPro and PPV due to proliferative vitreoretinopaties; 6 (66.7%) underwent PPV for retinal detachment or suprachoroidal hemorrhage that appeared after KPro surgery. Retina could be attached in 7 eyes (77.8%), and vision improved in 3 eyes (33.3%). In 1 eye, injected silicone oil moved to subconjunctival area through glaucoma drainage device.
Conclusion
In eyes with a Boston KPro, wide-angle viewing systems helped handling peripheral retinal problems successfully during PPV, with no observed inadequacy of imaging. Despite anatomical success in most cases, visual prognosis depends on vitality of the macula and the optic disc.



Similar content being viewed by others
Availability of data and material
The datasets during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Nonpassopon M, Niparugs M, Cortina MS (2020) Boston type 1 keratoprosthesis: updated perspectives. Clin Ophthalmol 14:1189–1200. https://doi.org/10.2147/OPTH.S219270
Priddy J, Bardan AS, Tawfik HS, Liu C (2019) Systematic review and meta-analysis of the medium- and long-term outcomes of the Boston type 1 keratoprosthesis. Cornea 38:1465–1473. https://doi.org/10.1097/ICO.0000000000002098
Rishi P, Rishi E, Koundaya VV, Mathur G, Iyer G, Srinivasan B (2016) Vitreoretinal complications in eyes with Boston keratoprosthesis type 1. Retina 36:603–610. https://doi.org/10.1097/IAE.0000000000000740
Dohlman CH, Nouri M (2005) Keratoprosthesis surgery. In: Foster CS, Azar DT, Dohlman CH (eds). Smolin and Thoft’s, The Cornea. 4th edn.: Lippincott, Williams & Wilkins, Philadelphia, PA, pp 1085–1095.
Eghrari AO, Ahmad S, Ramulu P, Iliff NT, Akpek EK (2016) The usage of a conjunctival flap to improve retention of Boston type 1 keratoprosthesis in severe ocular surface disease. Ocul Immunol Inflamm 24:555–560. https://doi.org/10.3109/09273948.2015.1037458
Saeed HN, Shanbhag S, Chodosh J (2017) The Boston keratoprosthesis. Curr Opin Ophthalmol 28:390–396. https://doi.org/10.1097/ICU.0000000000000373
Lee WB, Shtein RM, Kaufman SC, Deng SX, Rosenblatt MI (2015) Boston keratoprosthesis: outcomes and complications: a Report by the American academy of ophthalmology. Ophthalmology 122:1504–1511. https://doi.org/10.1016/j.ophtha.2015.03.025
Modjtahedi BS, Eliott D (2014) Vitreoretinal complications of the Boston keratoprosthesis. Semin Ophthalmol 29:338–348. https://doi.org/10.3109/08820538.2014.959204
Petrou P, Banerjee PJ, Wilkins MR, Singh M, Eastlake K, Limb GA, Charteris DG (2017) Characteristics and vitreoretinal management of retinal detachment in eyes with Boston keratoprosthesis. Br J Ophthalmol 101:629–633. https://doi.org/10.1136/bjophthalmol-2016-308854
Kanu LN, Niparugs M, Nonpassopon M, Karas FI, de la Cruz JM, Cortina MS (2020) Predictive factors of Boston type I keratoprosthesis outcomes: a long-term analysis. Ocul Surf 18:613–619. https://doi.org/10.1016/j.jtos.2020.07.012
Lekhanont K, Thaweesit P, Muntham D, Chuckpaiwong V, Vongthongsri A (2014) Medium-term outcomes of Boston type 1 keratoprosthesis implantation in Bangkok, Thailand. Cornea 33:1312–1319. https://doi.org/10.1097/ICO.0000000000000265
Kang KB, Karas FI, Rai R, Hallak JA, Kang JJ, de la Cruz J, Cortina MS (2018) Five year outcomes of Boston type I keratoprosthesis as primary versus secondary penetrating corneal procedure in a matched case control study. PLoS ONE 13:e0192381. https://doi.org/10.1371/journal.pone.0192381
Chang HY, Luo ZK, Chodosh J, Dohlman CH, Colby KA (2015) Primary implantation of type I Boston keratoprosthesis in nonautoimmune corneal diseases. Cornea 34:264–270. https://doi.org/10.1097/ICO.0000000000000357
Samarawickrama C, Strouthidis N, Wilkins MR (2018) Boston keratoprosthesis type 1: outcomes of the first 38 cases performed at Moorfields Eye Hospital. Eye (Lond) 32:1087–1092. https://doi.org/10.1038/s41433-018-0016-4
Robert MC, Moussally K, Harissi-Dagher M (2012) Review of endophthalmitis following Boston keratoprosthesis type 1. Br J Ophthalmol 96:776–780. https://doi.org/10.1136/bjophthalmol-2011-301263
Durand ML, Dohlman CH (2009) Successful prevention of endophthalmitis in eyes with the Boston keratoprosthesis. Cornea 28:896–901. https://doi.org/10.1097/ICO.0b013e3181983982
Gologorsky D, Williams BK Jr, Flynn HW Jr (2017) A posterior pole retinal detachment secondary to a macular hole can be repaired using standard techniques despite the limited view through a Boston keratoprosthesis. Am J Ophthalmol Case Rep 5:56–58. https://doi.org/10.1016/j.ajoc.2016.12.001
Jardeleza MSR, Rheaume MA, Chodosh J, Lane AM, Dohlman CH (2015) Retinal detachments after Boston keratoprosthesis: incidence, predisposing factors, and visual outcomes. Digit J Ophthalmol 21:1–15. https://doi.org/10.5693/djo.01.2015.10.001
Relimpio López MI, Gessa Sorroche M, Garrido Hermosilla AM, Laborda Guirao T, Espejo Arjona F, de la Rúa Franch ER (2016) Delayed Boston keratoprosthesis exchange due to a preceding vitreoretinal surgery with intraoperative choroidal detachment. Ophthalmologica 235:61. https://doi.org/10.1159/000442533
El-Khoury J, Mustafa M, Daoud R, Harissi-Dagher M (2021) Time to achieve best postoperative visual acuity following Boston keratoprosthesis surgery. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-317483.
Rudnisky CJ, Belin MW, Guo R, Ciolino JB; Boston type 1 keratoprosthesis study group (2016) Visual acuity outcomes of the Boston keratoprosthesis type 1: multicenter study results. Am J Ophthalmol 162:89-98. https://doi.org/10.1016/j.ajo.2015.10.023
Lim JI, Machen L, Arteaga A, Karas FI, Hyde R, Cao D, Niec M, Vajaranant TS, Cortina MS (2018) Comparison of visual and anatomical outcomes of eyes undergoing type I Boston keratoprosthesis with combination pars plana vitrectomy with eyes without combination vitrectomy. Retina 38:S125–S133. https://doi.org/10.1097/IAE.0000000000002036
Perez VL, Leung EH, Berrocal AM, Albini TA, Parel JM, Amescua G, Alfonso EC, Ali TK, Gibbons A (2017) Impact of total pars plana vitrectomy on postoperative complications in aphakic, snap-on, type 1 Boston keratoprosthesis. Ophthalmology 124:1504–1509. https://doi.org/10.1016/j.ophtha.2017.04.016
Shousha MA, Eleiwa T, Gibbons A, Smith C, Edelstein S, Kontadakis G, Schmitz Z, Abernathy J, Chod R, Bodnar Z, McDaniel K, Bentivegna R, Akduman L (2019) Risk of endophthalmitis in Boston type 1 Keratoprosthesis combined with vitrectomy and silicone oil insertion. J Ophthalmol. https://doi.org/10.1155/2019/9648614
Kornberg DL, Yannuzzi NA, Klufas MA, D’Amico DJ, Orlin A, Kiss S (2016) Ultra-widefield imaging of posterior segment pathology in the setting of the Boston keratoprosthesis. Retina 36:1101–1110. https://doi.org/10.1097/IAE.0000000000000833
Oshima Y (2012) Choices of wide-angle viewing systems for modern vitreoretinal surgery. Retina Today 9:37–42. https://retinatoday.com/pdfs/0912RT_F1_Oshima.pdf
Zhang T, Tang W, Xu G (2019) Comparative analysis of three-dimensional heads-up vitrectomy and traditional microscopic vitrectomy for vitreoretinal diseases. Curr Eye Res 44:1080–1086. https://doi.org/10.1080/02713683.2019.1612443
Acknowledgements
We owe our former head of department, Prof Dr. Ferit Hakan Öner, a dept of gratitude for his generous support for the management of these challenging cases in our clinic and for our academic progress. Unfortunately, he passed away on August 2020, but his legacy will live with us forever.
Funding
No funding was available.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Canan Asli Utine], [Mahmut Kaya] and [Kıvanç Kasal]. The first draft of the manuscript was written by [Kıvanç Kasal], and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
Dokuz Eylül University Ethical Committee Approval was obtained for this retrospective research (2020/28–34).
Consent to participate
Detailed signed informed consent was obtained from each subject before the surgery.
Consent for publication
Consent for publication was obtained from each subject upon admission to the hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Utine, C.A., Kaya, M. & Kasal, K. Wide-field vitreoretinal surgery in eyes with Boston type 1 keratoprosthesis. Int Ophthalmol 42, 997–1005 (2022). https://doi.org/10.1007/s10792-021-02083-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02083-7