Abstract
Purpose
To quantitatively analyze α-zone and β-zone peripapillary atrophy (PPA) in patients having early primary open-angle glaucoma (POAG) using fundus autofluorescence (FAF) in conjunction with spectral domain optical coherence tomography, colored photography and perimetry.
Design
This is an observational cross-sectional case–control study.
Methods
This study included 100 eyes (54 patients) of early to moderate POAG and 100 normal eyes (50 subjects). Ophthalmological examination, OCT for the optic nerve and FAF were performed. The extent of α-PPA and β-PPA was measured.
Results
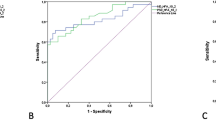
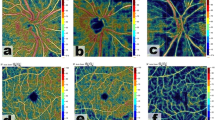
The extent of α-PPA and β-PPA as measured by FAF had higher values in POAG group as compared to control group (p values 0.003 and ≤ 0.001 for the total nasal and temporal extents, respectively). However, the nasal alpha and temporal beta zones showed more values in POAG patients as compared to normal controls (p values 0.002 and 0.024). The difference between the total extents of either zones alone was not significant. B-scan OCT was able to positively detect both zones. Detecting the alpha zone was significantly higher in the control group, while beta zone detection was significantly higher in the POAG group (p values ≤ 0.001).
Conclusion
The sensitivity of alpha zone detection was equal using colored photographs, FAF and B-scan OCT. FAF showed superior results in estimating the beta zone extent although OCT was more accurate in the anatomical delineation of Bruch’s membrane and RPE termination. The nasal alpha and temporal beta zone extents could be taken as early indices for evaluating early glaucomatous optic neuropathy.





Similar content being viewed by others
Data availability
All data are available from the authors and can be shared only if a request conforming to the ethics statement is provided.
References
Reznicek L, Seidensticker F, Mann T, Hübert I, Buerger A, Haritoglou C et al (2013) Correlation between peripapillary retinal nerve fiber layer thickness and fundus autofluorescence in primary open-angle glaucoma. Clin Ophthalmol 7:1883–1888
Jonas JB, Nguyen XN, Gusek GC, Naumann GO (1989) Parapapillary chorioretinal atrophy in normal and glaucoma eyes I Morphometric data. Invest Ophthalmol Vis Sci 30:908–918
Marjanovic I. The Optic Nerve in Glaucoma. In: Tomas Kubena (Eds.), The Mystery of Glaucoma, September 2011.doi: https://doi.org/10.5772/19811. https://www.intechopen.com/books/the-mystery-of-glaucoma
Jonas JB, Jonas SB, Jonas RA, Holbach L, Panda-Jonas S (2011) Histology of the parapapillary region in high myopia. Am J Ophthalmol 152:1021–1029
Jonas JB (2005) Clinical implications of peripapillary atrophy in glaucoma. Curr Opin Ophthalmol 16:84–88
Teng CC, De Moraes CG, Prata TS, Tello C, Ritch R, Liebmann JM (2010) Beta-zone parapapillary atrophy and the velocity of glaucoma progression. Ophthalmology 117:909–915
Shin JW, Uhm KB, Seo S (2015) Quantitative analysis of localized retinal nerve fiber layer defects using spectral domain optical coherence tomography. J Glaucoma 24:335–343
Viestenz A, Mardin CY, Langenbucher A, Naumann GO (2003) In-vivo measurement of autofluorescence in the parapapillary atrophic zone of optic discs with and without glaucomatous atrophy. Klin Monbl Augenheilkd 220:545–550
Hodapp E, Parrish RK II, Anderson DR (1993) Clinical decisions in glaucoma. The CV Mosby Co, St Louis, pp 52–61
Savatovsky E, Mwanza JC, Budenz DL, Feuer WJ, Vandenbroucke R, Schiffman JC, Anderson DR (2015) Longitudinal changes in peripapillary atrophy in the ocular hypertension treatment study: a case-control assessment. Ophthalmology 122(1):79–86
Jonas J, Hayreh S, Tao Y (2014) Clinicopathological correlation of parapapillary atrophy in monkeys with experimental glaucoma and temporary central retinal artery occlusion. Indian J Ophthalmol 62:219–223
Dysli C, Wolf S, Berezin MY, Sauer L, Hammer M, Zinkernagel MS (2017) Fluorescence lifetime imaging ophthalmoscopy. Prog Retin Eye Res 60:120–143
Grewal DS, Merlau DJ, Giri P, Munk MR, Fawzi AA, Jampol LM, Tanna AP (2017) Peripapillary retinal splitting visualized on OCT in glaucoma and glaucoma suspect patients. PLoS One 23(12):e0182816. https://doi.org/10.1371/journal.pone.0182816
Miki A, Ikuno Y, Weinreb RN, Yokoyama J, Asai T, Usui S, Nishida K (2017) Measurements of the parapapillary atrophy zones in en face optical coherence tomography images. PLoS One 12:1–12
Dagdelen K, Dirican E (2018) The assessment of structural changes on optic nerve head and macula in primary open angle glaucoma and ocular hypertension. Int J Ophthalmol 11:1631–1637
Sun J, Wang J, You R, Wang Y (2018) Is the retinal vasculature related to β-peripapillary atrophy in nonpathological high myopia? an optical coherence tomography angiography study in Chinese adults. J Ophthalmol. https://doi.org/10.1155/2018/7895238
Wang Y, Xu L, Zhang L, Yang H, Ma Y, Jonas JB (2008) Peripapillary atrophy in elderly Chinese in rural and urban Beijing. Eye 22:261–266
Kolář R, Laemmer R, Jan J, Mardin ChY (2009) The segmentation of zones with increased autofluorescence in the junctional zone of parapapillary atrophy. Physiol Meas 30:505–516
Garg A, Blumberg DM, Al-Aswad LA, Oll M, Yzer S, Forbes M, Allikmets RL, Bearelly S (2017) Associations between β-peripapillary atrophy and reticular pseudodrusen in early age-related macular degeneration. Invest Ophthalmol Vis Sci 58:2810–2815
Alasil T, Wang K, Yu F, Field MG, Lee H, Baniasadi N, de Boer JF, Coleman AL, Chen TC (2014) Correlation of retinal nerve fiber layer thickness and visual fields in glaucoma: a broken stick model. Am J Ophthalmol 157:953–959
Jonas JB, Bergua A, Schmitz-Valckenberg P, Papastathopoulos KI, Budde WM (2000) Ranking of optic disc variables for detection of glaucomatous optic nerve damage. Invest Ophthalmol Vis Sci 41:1764–1773
Ehrlich JR, Radcliffe NM (2010) The role of clinical parapapillary atrophy evaluation in the diagnosis of open angle glaucoma. Clin Ophthalmol 4:971–976
Viestenz A, Langenbucher A, Mardin CY (2006) Parapapilläre autofluoreszenz als glaukomindikator. Klin Monatsbl Augenheilkd 223:315–320. https://doi.org/10.1055/s-2005-858856
Yoo YJ, Lee EJ, Kim TW (2016) Intereye difference in the microstructure of parapapillary atrophy in unilateral primary open-angle glaucoma. Invest Ophthalmol Vis Sci 57:4187–4193
Seidensticker F, Reznicek L, Mann T, Hübert I, Kampik A, Ulbig M, Hirneiss C, Neubauer AS, Kernt M (2014) Assessment of β-zone peripapillary atrophy by optical coherence tomography and scanning laser ophthalmoscopy imaging in glaucoma patients. Clin Ophthalmol 8:1233–1239
Funding
None.
Author information
Authors and Affiliations
Contributions
SY was involved in examination, performing investigations and data collection (investigation, resources and data curation). KA helped in conceptualization, review editing and supervision. RAA contributed to conceptualization, participation in revising patients’ selection criteria and manuscript revision. RSHMA was involved in conceptualization, writing original draft, review editing, supervision and corresponding author. All authors have seen and approved the final version of the manuscript being submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Consent for publication
Written informed consent was obtained from all participants, provided that no data are published that could lead to personal identification.
Consent for participate
Written informed consent was obtained from all participants.
Ethical approval
Data collection conformed to all local laws and complied with the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants. The protocol was revised and approved by the review board of the Ophthalmology Department, Cairo University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sayed, S.Y., Raafat, K.A., Ahmed, R.A. et al. Evaluation of peripapillary atrophy in early open-angle glaucoma using autofluorescence combined with optical coherence tomography. Int Ophthalmol 41, 2405–2415 (2021). https://doi.org/10.1007/s10792-021-01795-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-01795-0