Abstract
Purpose
To compare the results of treatment of idiopathic full-thickness macular holes (MHs) with and without the use of autologous platelet-rich plasma (APRP).
Methods
This partially retrospective study included 152 patients (152 eyes) with MHs operated in the years 2010–2014 using conventional technology with internal limiting membrane peeling (control group) and 62 patients (62 eyes), operated by the same surgeons in 2015–2017 with additional application of APRP on MH (platelet group). Pre and postoperative best-corrected visual acuities (BCVA) were recorded, and retinal microstructure was studied using optical coherence tomography. Thirty-seven patients in the platelet group and 80 controls were followed for at least 12 months (for visual outcomes 15 controls were followed for 15–24 months). The data of 72 controls (72 eyes) were analyzed retrospectively.
Results
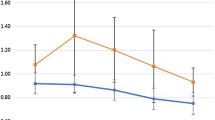
The minimum diameter of the MH in the platelet group was larger than in controls: 454 ± 186 vsersus 381 ± 148 μm (P = 0.003). Despite this, all MHs in the platelet group were closed, while in the control group 11 holes (7.2%) remained open (P = 0.036). The final mean BCVA, standardized by the minimum diameter of the macular hole, was higher in the platelet group by 3.9 ETDRS letters (P = 0.012). After surgery with APRP, foveal hyperreflective lesion (presumably glial proliferation) was found, which persisted in most large MHs, but gradually disappeared in small and most medium MHs.
Conclusion
The use of APRP significantly improves the anatomical and functional results of treatment of idiopathic MHs. In very large MHs, APRP presumably enhances glial proliferation, which ensures their closure.


Similar content being viewed by others
Availability of data and materials
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Gaudric A, Massin P, Paques M, Santiago PY, Guez JE, Le Gargasson JF, Mundler O, Drouet L (1995) Autologous platelet concentrate for the treatment of full-thickness macular holes. Graefes Arch Clin Exp Ophthalmol 233(9):549–554. https://doi.org/10.1007/BF00404704
Paques M, Chastang C, Mathis A, Sahel J, Massin P, Dosquet C, Korobelnik JF, Le Gargasson JF, Gaudric A (1999) Effect of autologous platelet concentrate in surgery for idiopathic macular hole: results of a multicenter, double-masked, randomized trial. Platelets in Macular Hole Surgery Group. Ophthalmology 106(5):932–938. https://doi.org/10.1016/s0161-6420(99)00512-6
Vote BJ, Membrey WL, Casswell AG (2004) Autologous platelets for macular hole surgery: the Sussex Eye Hospital experience. Clin Experiment Ophthalmol 32(5):472–477. https://doi.org/10.1111/j.1442-9071.2004.00866.x
Cheung CMG, Munshi V, Mughal S, Mann J, Hero M (2005) Anatomical success rate of macular hole surgery with autologous platelet without internal-limiting membrane peeling. Eye 19(11):1191–1193. https://doi.org/10.1038/sj.eye.6701733
Kapoor KG, Khan AN, Tieu BC, Khurshid GS (2012) Revisiting autologous platelets as an adjuvant in macular hole repair: chronic macular holes without prone positioning. Ophthalmic Surg Lasers Imaging 43(4):291–295. https://doi.org/10.3928/15428877-20120426-03
Konstantinidis A, Hero M, Nanos P, Panos GD (2013) Efficacy of autologous platelets in macular hole surgery. Clin Ophthalmol 7:745–750. https://doi.org/10.2147/OPTH.S44440
Engelmann K, Sievert U, Hölig K, Wittig D, Weßlau S, Domann S, Siegert G, Valtink M (2015) Wirkung von autologem Thrombozytenkonzentrat auf den anatomischen und funktionellen Erfolg bei der Chirurgie des Makulaforamens im Spatstadium: Eine retrospektive Analyse: [Effect of autologous platelet concentrates on the anatomical and functional outcome of late stage macular hole surgery: a retrospective analysis]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 58(11–12):1289–1298. https://doi.org/10.1007/s00103-015-2251-1
Figueroa MS, Govetto A, Arriba-Palomero Pd (2016) Short-term results of platelet-rich plasma as adjuvant to 23-G vitrectomy in the treatment of high myopic macular holes. Eur J Ophthalmol 26(5):491–496. https://doi.org/10.5301/ejo.5000729
Purtskhvanidze K, Frühsorger B, Bartsch S, Hedderich J, Roider J, Treumer F (2018) Persistent full-thickness idiopathic macular hole: anatomical and functional outcome of revitrectomy with autologous platelet concentrate or autologous whole blood. Ophthalmologica 239(1):19–26. https://doi.org/10.1159/000481268
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, Sadda SR, Sebag J, Spaide RF, Stalmans P (2013) The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120(12):2611–2619. https://doi.org/10.1016/j.ophtha.2013.07.042
R Core Team R: A language and environment for statistical computing (2020) R Foundation for Statistical Computing, Vienna, Austria. Available at: https://www.R-project.org/. Accessed on February 12.
Naing NN (2000) Easy way to learn standardization: direct and indirect methods. Malays J Med Sci 7(1):10–15
Tripepi G, Jager KJ, Dekker FW, Zoccali C (2010) Stratification for confounding——part 2: direct and indirect standardization. Nephron Clin Pract 116(4):c322–c325. https://doi.org/10.1159/000319591
Shpak AA, Shkvorchenko DO, Sharafetdinov IK, Yukhanova OA (2016) Predicting anatomical results of surgical treatment of idiopathic macular hole. Int J Ophthalmol 9(2):253–257. https://doi.org/10.18240/ijo.2016.02.13
Nugent RB, Lee GA (2015) Ophthalmic use of blood-derived products. Surv Ophthalmol 60(5):406–434. https://doi.org/10.1016/j.survophthal.2015.03.003
Kung YH, Wu TT (2013) The effect of autologous serum on vitrectomy with internal limiting membrane peeling for idiopathic macular hole. J Ocul Pharmacol Ther 29(5):508–511. https://doi.org/10.1089/jop.2012.0121
Olsen TW, Sternberg P Jr, Capone A Jr, Martin DF, Lim JI, Grossniklaus HE, Aaberg TM Sr (1998) Macular hole surgery using thrombin-activated fibrinogen and selective removal of the internal limiting membrane. Retina 18(4):322–329. https://doi.org/10.1097/00006982-199807000-00005
Dimopoulos S, William A, Voykov B, Ziemssen F, Bartz-Schmidt KU, Spitzer MS (2017) Anatomical and visual outcomes of autologous thrombocyte serum concentrate in the treatment of persistent full-thickness idiopathic macular hole after ILM peeling with brilliant blue G and membrane blue dual. Acta Ophthalmol 95(5):e429–e430. https://doi.org/10.1111/aos.12971
Degenhardt V, Busch C, Jochmann C, Meier P, Unterlauft JD, Mößner A, Edel E, Tewari R, Wiedemann P, Rehak M (2019) Prognostic factors in patients with persistent full-thickness idiopathic macular holes treated with re-vitrectomy with autologous platelet concentrate. Ophthalmologica 242(4):214–221. https://doi.org/10.1159/000502386
Babu N, Kohli P, Ramachandran NO, Adenuga OO, Ahuja A, Ramasamy K (2020) Comparison of platelet-rich plasma and inverted internal limiting membrane flap for the management of large macular holes: a pilot study. Indian J Ophthalmol 68(5):880–884. https://doi.org/10.4103/ijo.IJO_1357_19
Coca M, Makkouk F, Picciani R, Godley B, Elkeeb A (2017) Chronic traumatic giant macular hole repair with autologous platelets. Cureus 9:e955. https://doi.org/10.7759/cureus.955
Ko TH, Witkin AJ, Fujimoto JG, Chan A, Rogers AH, Baumal CR, Schuman JS, Drexler W, Reichel E, Duker JS (2006) Ultrahigh-resolution optical coherence tomography of surgically closed macular holes. Arch Ophthalmol 124(6):827–836. https://doi.org/10.1001/archopht.124.6.827
Christensen U, Krøyer K, Sander B, Larsen M, la Cour M (2009) Prognostic significance of delayed structural recovery after macular hole surgery. Ophthalmology 116(12):2430–2436. https://doi.org/10.1016/j.ophtha.2009.06.001
Michalewska Z, Michalewski J, Nawrocki J (2010) Continuous changes in macular morphology after macular hole closure visualized with spectral optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 248(9):1249–1255. https://doi.org/10.1007/s00417-010-1370-5
Wakabayashi T, Fujiwara M, Sakaguchi H, Kusaka S, Oshima Y (2010) Foveal microstructure and visual acuity in surgically closed macular holes: spectral-domain optical coherence tomographic analysis. Ophthalmology 117(9):1815–1824. https://doi.org/10.1016/j.ophtha.2010.01.017
Kawano H, Uemura A, Sakamoto T (2011) Incidence of outer foveal defect after macular hole surgery. Am J Ophthalmol 151(2):318–322. https://doi.org/10.1016/j.ajo.2010.08.034
Funata M, Wendel RT, de la Cruz Z, Green WR (1992) Clinicopathologic study of bilateral macular holes treated with pars plana vitrectomy and gas tamponade. Retina 12(4):289–298. https://doi.org/10.1097/00006982-199212040-00001
Madreperla SA, Geiger GL, Funata M, de la Cruz Z, Green WR (1994) Clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade. Ophthalmology 101(4):682–686. https://doi.org/10.1016/s0161-6420(94)31278-4
Rosa RH Jr, Glaser BM, de la Cruz Z, Green WR (1996) Clinicopathologic correlation of an untreated macular hole and a macular hole treated by vitrectomy, transforming growth factor-beta 2, and gas tamponade. Am J Ophthalmol 122(6):853–863. https://doi.org/10.1016/s0002-9394(14)70382-4
Hara S, Sakuraba T, Nakazawa M (2000) Morphological changes of retinal pigment epithelial and glial cells at the site of experimental retinal holes. Graefes Arch Clin Exp Ophthalmol 238(8):690–695. https://doi.org/10.1007/s004170000168
Castelnovo L, Dosquet C, Gaudric A, Sahel J, Hicks D (2000) Human platelet suspension stimulates porcine retinal glial proliferation and migration in vitro. Invest Ophthalmol Vis Sci 41(2):601–609
Burmeister SL, Hartwig D, Limb GA, Kremling C, Hoerauf H, Müller M, Geerling G (2009) Effect of various platelet preparations on retinal Müller cells. Invest Ophthalmol Vis Sci 50(10):4881–4886. https://doi.org/10.1167/iovs.08-3057
Acknowledgements
The authors are grateful to Ilias Kh. Sharafetdinov, MD, Ph.D for performing part of the surgeries and to Olga A. Yukhanova for performing optical coherence tomography in the control group.
Funding
None
Author information
Authors and Affiliations
Contributions
AS conceived and designed the research, drafted the manuscript. DS performed surgeries. EK performed examinations. AS, DS, and EK analyzed and interpreted the data. DS, EK made critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Ethical approval
This study adhered to the tenets of the HELSINKI declaration and was approved by the Local Ethics Committee of The S. Fyodorov Eye Microsurgery Federal State Institution. Informed consent was obtained from all subjects included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shpak, A.A., Shkvorchenko, D.O. & Krupina, E.A. Surgical treatment of macular holes with and without the use of autologous platelet-rich plasma. Int Ophthalmol 41, 1043–1052 (2021). https://doi.org/10.1007/s10792-020-01662-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01662-4