Abstract
Purpose
To evaluate the intrasession repeatability for non-invasive break-up time (NIBUT) and tear meniscus height (TMH) measurements provided by a new multi-diagnostic platform, and to assess the interobserver reproducibility of TMH measures.
Methods
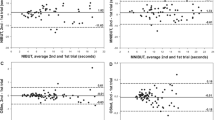
Twenty-one healthy eyes of 21 patients (age, 23–65 years) were enrolled. A complete eye examination was performed in all cases with the VX120+ device (Visionix-Luneau Technologies), including an analysis with the new Dry Eye module, performing three consecutive measurements. The within-subject standard deviation (Sw) and Bland–Altman plots were used to assess intersession repeatability. Differences between examiners for TMH were also analysed.
Results
No statistically significant differences were found between repeated measures of NIBUT (time associated with the first break) and TMH (p > 0.05). However, significant differences were found for NIBUT50% (time associated with half of breaks of the tear film) (p < 0.05). Mean Sw was 0.9 s, 1.4 s and 0.05 mm for NIBUT, NIBUT50% and TMH, respectively. Ranges of agreement between consecutive measures were below 3.5 s and 4.5 s for NIBUT and NIBUT50%, respectively, and below 0.16 mm for TMH. Furthermore, no significant differences were found between examiners in TMH measure, with an inter-examiner range of agreement of 0.12 mm.
Conclusions
The new dry eye platform of the VX120+ platform evaluated provides objective automated measures of NIBUT and TMH, with acceptable level of intrasession repeatability for clinical screening purposes.





Similar content being viewed by others
References
Wei A, Le Q, Hong J et al (2016) Assessment of lower tear meniscus. Optom Vis Sci 93:1420–1425
Santodomingo-Rubido J, Wolffsohn JS, Gilmartin B (2006) Comparison between graticule and image capture assessment of lower tear film meniscus height. Cont Lens Anterior Eye 29:169–173
Imamura H, Tabuchi H, Nakakura S et al (2018) Usability and reproducibility of tear meniscus values generated via swept-source optical coherence tomography and the slit lamp with a graticule method. Int Ophthalmol 38:679–686
Binotti WW, Bayraktutar B, Ozmen MC et al (2020) A review of imaging biomarkers of the ocular surface. Eye Contact Lens 46:S84–105
Hong J, Sun X, Wei A et al (2013) Assessment of tear film stability in dry eye with a newly developed Keratograph. Cornea 32:716–721
Gumus K, Crockett CH, Rao K et al (2011) Noninvasive assessment of tear stability with the tear stability analysis system in tear dysfunction patients. Invest Ophthalmol Vis Sci 52:456–461
Ozulken K, Aydemir GA, Tekin K, Mumcuoğlu T (2020) Correlation of non-invasive tear break-up time with tear osmolarity and other invasive tear function tests. Semin Ophthalmol 35:78–85
Bandlitz S, Peter B, Pflugi T et al (2020) Agreement and repeatability of four different devices to measure non-invasive tear breakup time (NIBUT). Cont Lens Anterior Eye. https://doi.org/10.1016/j.clae.2020.02.018
Lee R, Yeo S, Aung HT, Tong L (2016) Agreement of noninvasive tear break-up time measurement between tomey RT-7000 auto refractor-keratometer and oculus keratograph 5M. Clin Ophthalmol 10:1785–1790
Piñero DP, López-Navarro A, Cabezos I et al (2017) Intrasession repeatability of refractive and ocular aberrometric measurements obtained using a multidiagnostic device in healthy eyes. Clin Optom 9:91–96
Piñero DP, Cabezos I, López-Navarro A et al (2017) Intrasession repeatability of ocular anatomical measurements obtained with a multidiagnostic device in healthy eyes. BMC Ophthalmol 17:193
Piñero DP, López-Navarro A, Cabezos I et al (2017) Corneal topographic and aberrometric measurements obtained with a multidiagnostic device in healthy eyes: intrasession repeatability. J Ophthalmol 2017:2149145
Sanchez I, Ortiz-Toquero S, Martin R (2018) Intrasession repeatability and intersession reproducibility measurements using VX120 multidiagnostic unit. Eye Contact Lens 44:S266–S272
Gordon-Shaag A, Piñero DP, Kahloun C et al (2018) Validation of refraction and anterior segment parameters by a new multi-diagnostic platform (VX120). J Optom 11:242–251
Fernández J, Rodríguez-Vallejo M, Martínez J et al (2018) Agreement and repeatability of objective systems for assessment of the tear film. Graefes Arch Clin Exp Ophthalmol 256:1535–1541
Best N, Drury L, Wolffsohn JS (2012) Clinical evaluation of the Oculus Keratograph. Cont Lens Anterior Eye 35:171–174
Cox SM, Nichols KK, Nichols JJ (2015) Agreement between automated and traditional measures of tear film breakup. Optom Vis Sci 92:e257–e263
Wolffsohn JS, Arita R, Chalmers R et al (2017) TFOS DEWS II diagnostic methodology report. Ocul Surf 15:539–574
Arriola-Villalobos P, Fernández-Vigo JI, Díaz-Valle D et al (2015) Assessment of lower tear meniscus measurements obtained with Keratograph and agreement with Fourier-domain optical-coherence tomography. Br J Ophthalmol 99:1120–1125
Akiyama R, Usui T, Yamagami S (2015) Diagnosis of dry eye by tear meniscus measurements using anterior segment swept source optical coherence tomography. Cornea 34:S115–S120
Singh A, Vanathi M, Kishore A et al (2019) Evaluation of strip meniscometry, tear meniscus height and depth in the diagnosis of dry eye disease in asian Indian eyes. Ocul Surf 17:747–752
Zhu K, Xie W, Ying J et al (2016) Evaluation of tear film and meibomian gland function in dry eye patients using Keratograph 5M. Zhejiang Da Xue Xue Bao Yi Xue Ban 45:422–428
Tian L, Qu JH, Zhang XY et al (2016) Repeatability and reproducibility of noninvasive keratograph 5m measurements in patients with dry eye disease. J Ophthalmol 2016:8013621
Nichols JJ, Nichols KK, Puent B et al (2002) Evaluation of tear film interference patterns and measures of tear break-up time. Optom Vis Sci 79:363–369
Markoulli M, Duong TB, Lin M et al (2018) Imaging the tear film: a comparison between the subjective Keeler Tearscope-PlusTM and the objective Oculus® Keratograph 5M and LipiView® interferometer. Curr Eye Res 43:155–162
Papas EB, Vajdic CM (2000) Inter-ocular characteristics of the pre-contact lens tear film. Curr Eye Res 20:248–250
Funding
The author David P Piñero has been supported by the Ministry of Economy, Industry and Competitiveness of Spain within the program Ramón y Cajal, RYC-2016-20471.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author David P Piñero has been supported by the Ministry of Economy, Industry and Competitiveness of Spain within the program Ramón y Cajal, RYC-2016-20471. The rest of authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Molina-Martín, A., de Fez, D. & Piñero, D.P. Repeatability of non-invasive break-up time measures with a new automated dry eye platform in healthy eyes. Int Ophthalmol 40, 2855–2864 (2020). https://doi.org/10.1007/s10792-020-01470-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01470-w