Abstract
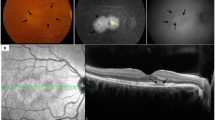
The purpose of this study was to review unilateral acute maculopathy associated with hand–foot–mouth disease with a representative case. Clinical course of a 24-year-old male case with unilateral acute idiopatic maculopathy documented by multimodal imaging is presented, and a review of similar cases is given. On initial examination, best-corrected visual acuity was 20/200 in the left eye. Fundoscopy revealed grayish-yellowish subretinal exudate, and fluorescein angiography demonstrated irregular mottled hyperfluorescence at the central macula. Spectral domain optical coherence tomography demonstrated disruption of ellipsoid layer, which partially resolved on follow-up examinations. Best-corrected visual acuity increased to 20/20 at 3 months, with persistent retinal changes, and mild disruption of ellipsoid layer and persistent mild metamorphopsia. Although hand–foot–mouth disease is usually benign and self-limited in childhood, it may be rarely associated with unilateral vision loss due to maculopathy, especially at early adulthood in both sexes. Vision loss associated with this eruption is acute and reversible in most cases, despite some residual pigmentary and scarring changes in all cases and persistent mild visual loss in some cases. Exact pathophysiology, the causes of variability of clinical features, adulthood onset, unilateral involvement, and role of multimodal imaging are issues which need to be clarified with further research.


Similar content being viewed by others
References
Flor de Lima B, Silva J, Rodrigues AC et al (2013) Hand, foot, and mouth syndrome in an immunocompetent adult: a case report. BMC Res Notes 6:441
Yanuzzi LA, Jampol LM, Rabb MF et al (1991) Unilateral acute idiopathic maculopathy. Arch Ophthalmol 109:1411–1416
Freund KB, Yannuzzi LA, Barile GR et al (1996) The expanding clinical spectrum of unilateral acute idiopathic maculopathy. Arch Ophthalmol 114:555–559
Vaz-Pereira S, Macedo M, De Salvo G, Pal B (2014) Multimodal imaging of exudative maculopathy associated with hand-foot-mouth disease. Ophthalmic Surg Lasers Imaging Retina 45:e14–e17
Haamann P, Kesel L, Larsen M (2000) Monofocal outer retinitis associated with hand, foot, and mouth disease caused by coxackievirus. Am J Ophthalmol 129:552–553
Beck AP, Jampol LM, Glaser DA, Pollack JS (2004) Is coxsackievirus the cause of unilateral acute idiopathic maculopathy? Arch Ophthalmol 122:121–123
Jung CS, Payne JF, Bergstrom CS et al (2012) Multimodality diagnostic imaging in unilateral acute idiopathic maculopathy. Arch Ophthalmol 130:50–56
Hughes EH, Hunyor AP, Gorbatov M, Ho IV (2012) Acute idiopathic maculopathy with coxsackievirus infection. Retin Cases Brief Rep 6:19–21
Ng SK, Ebneter A, Gilhotra JS (2013) Atypical findings in delayed presentation of unilateral acute idiopathic maculopathy. Int Ophthalmol 33:387–389
Sheyman A, Pahk P, Tannen B (2013) Unilateral acute idiopathic maculopathy associated with hand-foot-mouth disease. J Ocular Biol 1:2
Demirel S, Batioğlu F, Özmert E, Batioglu F (2014) Unilateral acute maculopathy related to hand, foot, and mouth disease: OCT and fluorescein angiography findings of a very rare disease. Eur J Ophthalmol 24:131–133
Agrawal R, Bhan K, Balaggan K et al (2015) Unilateral acute maculopathy associated with adult onset hand, foot and mouth disease: case report and review of literature. J Ophthalmic Inflamm Infect 5:2
Huemer HP, Larcher C, Kirchebner W et al (1996) Susceptibility of human retinal pigment epithelial cells to different viruses. Graefes Arch Clin Exp Ophthalmol 234:177–185
Ercolini AM, Miller SD (2009) The role of infections in autoimmune disease. Clin Exp Immunol 155:1–15
Suh MH, Seo JM, Park KH, Yu HG (2009) Associations between macular findings byoptical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol 147:473–480
Oster SF, Mojana F, Brar M et al (2010) Disruption of the photoreceptor inner segment/outer segment layer on spectral domain optical coherence tomography is a predictor of poor visual acuity in patients withepiretinal membranes. Retina 30:713–718
Maheshwary AS, Oster SF, Yuson RM et al (2010) The association between percent disruption of the photoreceptor inner segment-outer segment junction and visual acuity in diabetic macular edema. Am J Ophthalmol 150:63–67
Funding source
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Duman, R., Duman, N., Kutluksaman, B. et al. A review of unilateral acute idiopatic maculopathy related to hand–foot–mouth disease with a representative case. Int Ophthalmol 36, 445–452 (2016). https://doi.org/10.1007/s10792-015-0147-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-015-0147-6