Abstract
The NOD-like receptor (NLR) family pyrin domain-containing protein 3 (NLRP3) inflammasome is implicated in the pathogenesis of multiple diseases including neuroinflammation associated with multiple sclerosis (MS). However, the extent to which NLRP3 has a pathobiological role in MS-associated central neuropathic pain (CNP) is unknown. Hence, the present study was designed to address this issue using an optimised relapsing–remitting experimental encephalomyelitis (RR-EAE)-mouse model of MS-associated neuropathic pain. RR-EAE mice with fully developed mechanical allodynia in the bilateral hindpaws (paw withdrawal thresholds (PWTs) ≤ 1 g) at day 16 post-immunisation (p.i.) were administered single oral bolus doses of MCC950, a selective and potent small-molecule inhibitor of NLRP3, once daily for 21 consecutive days. Following administration of the first dose of MCC950 at 50 mg kg−1, the mean (± SEM) peak anti-allodynic effect was observed at ~ 1 h post-dosing with a duration of action of ~ 2 h. Following chronic dosing with MCC950, mechanical allodynia in the bilateral hindpaws was progressively reversed by oral treatment with MCC950 (50 mg kg−1 day−1), but not vehicle. Specifically, by day 25 p.i. and continuing until study completion on day 36 p.i., bilateral hindpaw PWTs of RR-EAE mice treated with MCC950 (50 mg kg−1 day−1) did not differ significantly (P > 0.05) from the corresponding hindpaw PWTs for the sham (control) group. In addition, MCC950 at 50 mg kg−1 day−1 attenuated disease relapses in RR-EAE mice indicated by tail limpness as well as hindlimb weakness. Together, our findings suggest that inhibition of NLRP3 inflammasome activation may be a potential therapeutic approach to alleviate MS-associated CNP and disease relapses in patients with RR-MS.




Similar content being viewed by others
Abbreviations
- CNP:
-
Central neuropathic pain
- NLRP3:
-
NOD-like receptor (NLR) family pyrin domain-containing protein 3
- PWT:
-
Paw withdrawal threshold
- RR-EAE:
-
Relapsing–remitting experimental autoimmune encephalomyelitis
References
Bauernfeind FG, Horvath G, Stutz A, Alnemri ES, Macdonald K, Speert D, Fernandes-Alnemri T, Wu J, Monks BG, Fitzgerald KA, Hornung V, Latz E (2009) Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J Immunol 183:787–791
Beiske AG, Pedersen ED, Czujko B, Myhr KM (2004) Pain and sensory complaints in multiple sclerosis. Eur J Neurol 11:479–482
Bielekova B, Martin R (2004) Development of biomarkers in multiple sclerosis. Brain 127:1463–1478
Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL (1994) Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53:55–63
Chen L, Li X, Huang L, Wu Q, Chen L, Wan Q (2014) Chemical stimulation of the intracranial dura activates NALP3 inflammasome in trigeminal ganglia neurons. Brain Res 1566:1–11
Chen W, Foo S-S, Zaid A, Teng T-S, Herrero LJ, Wolf S, Tharmarajah K, Vu LD, Van Vreden C, Taylor A, Freitas JR, Li RW, Woodruff TM, Gordon R, Ojcius DM, Nakaya HI, Kanneganti T-D, O’Neill LAJ, Robertson AAB, King NJ, Suhrbier A, Cooper MA, Ng LFP, Mahalingam S (2017) Specific inhibition of NLRP3 in chikungunya disease reveals a role for inflammasomes in alphavirus-induced inflammation. Nat Microbiol. doi:10.1038/s41564-017-0015-4
Coll RC, Robertson AA, Chae JJ, Higgins SC, Munoz-Planillo R, Inserra MC, Vetter I, Dungan LS, Monks BG, Stutz A, Croker DE, Butler MS, Haneklaus M, Sutton CE, Nunez G, Latz E, Kastner DL, Mills KH, Masters SL, Schroder K, Cooper MA, O’neill LA (2015) A small-molecule inhibitor of the NLRP3 inflammasome for the treatment of inflammatory diseases. Nat Med 21:248–255
Compston A, Coles A (2008) Multiple sclerosis. Lancet 372:1502–1517
Cordero MD, Alcocer-Gómez E, Culic O, Carrión AM, de Miguel M, Díaz-Parrado E, Pérez-Villegas EM, Bullón P, Battino M, Sánchez-Alcazar JA (2014) NLRP3 Inflammasome is activated in fibromyalgia: the effect of Coenzyme Q10. Antioxid Redox Signal 20:1169–1180
Curto-Reyes V, Kirschmann G, Pertin M, Drexler SK, Decosterd I, Suter MR (2015) Neuropathic pain phenotype does not involve the NLRP3 inflammasome and its end product interleukin-1beta in the mice spared nerve injury model. PLoS ONE 10:e0133707
Deuis JR, Yin K, Cooper MA, Schroder K, Vetter I (2017) Role of the NLRP3 inflammasome in a model of acute burn-induced pain. Burns 43:304–309
Dworkin RH, O’connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, Kent JL, Krane EJ, Lebel AA, Levy RM, Mackey SC, Mayer J, Miaskowski C, Raja SN, Rice ASC, Schmader KE, Stacey B, Stanos S, Treede R-D, Turk DC, Walco GA, Wells CD (2010) Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 85:S3–S14
Franchi L, Eigenbrod T, Munoz-Planillo R, Ozkurede U, Kim YG, Chakrabarti A, Gale M Jr, Silverman RH, Colonna M, Akira S, Nunez G (2014) Cytosolic double-stranded RNA activates the NLRP3 inflammasome via MAVS-induced membrane permeabilization and K+ efflux. J Immunol 193:4214–4222
Grace PM, Strand KA, Galer EL, Urban DJ, Wang X, Baratta MV, Fabisiak TJ, Anderson ND, Cheng K, Greene LI, Berkelhammer D, Zhang Y, Ellis AL, Yin HH, Campeau S, Rice KC, Roth BL, Maier SF, Watkins LR (2016) Morphine paradoxically prolongs neuropathic pain in rats by amplifying spinal NLRP3 inflammasome activation. Proc Natl Acad Sci USA 113:E3441–E3450
Gris D, Ye Z, Iocca HA, Wen H, Craven RR, Gris P, Huang M, Schneider M, Miller SD, Ting JP (2010) NLRP3 plays a critical role in the development of experimental autoimmune encephalomyelitis by mediating Th1 and Th17 responses. J Immunol 185:974–981
Guo H, Callaway JB, Ting JPY (2015) Inflammasomes: mechanism of action, role in disease, and therapeutics. Nat Med 21:677–687
Hadjimichael O, Kerns RD, Rizzo MA, Cutter G, Vollmer T (2007) Persistent pain and uncomfortable sensations in persons with multiple sclerosis. Pain 127:35–41
Heneka MT, Kummer MP, Stutz A, Delekate A, Schwartz S, Vieira-Saecker A, Griep A, Axt D, Remus A, Tzeng TC, Gelpi E, Halle A, Korte M, Latz E, Golenbock DT (2013) NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature 493:674–678
Inoue M, Williams KL, Gunn MD, Shinohara ML (2012) NLRP3 inflammasome induces chemotactic immune cell migration to the CNS in experimental autoimmune encephalomyelitis. Proc Natl Acad Sci USA 109:10480–10485
Jha S, Srivastava SY, Brickey WJ, Iocca H, Toews A, Morrison JP, Chen VS, Gris D, Matsushima GK, Ting JP (2010) The inflammasome sensor, NLRP3, regulates CNS inflammation and demyelination via caspase-1 and interleukin-18. J Neurosci 30:15811–15820
Kallaur AP, Oliveira SR, Colado Simao AN, Delicato De Almeida ER, Kaminami Morimoto H, Lopes J, De Carvalho Jennings Pereira WL, Marques Andrade R, Muliterno Pelegrino L, Donizete Borelli S, Kaimen Maciel DR, Reiche EM (2013) Cytokine profile in relapsing-remitting multiple sclerosis patients and the association between progression and activity of the disease. Mol Med Rep 7:1010–1020
Khan N, Smith MT (2014) Multiple sclerosis-induced neuropathic pain: pharmacological management and pathophysiological insights from rodent EAE models. Inflammopharmacology 22:1–22
Khan N, Woodruff TM, Smith MT (2014) Establishment and characterization of an optimized mouse model of multiple sclerosis-induced neuropathic pain using behavioral, pharmacologic, histologic and immunohistochemical methods. Pharmacol Biochem Behav 126:13–27
Khan N, Gordon R, Woodruff TM, Smith MT (2015) Antiallodynic effects of alpha lipoic acid in an optimized RR-EAE mouse model of MS-neuropathic pain are accompanied by attenuation of upregulated BDNF-TrkB-ERK signaling in the dorsal horn of the spinal cord. Pharmacol Res Perspect 3:e00137
Kilkenny C, Browne W, Cuthill IC, Emerson M, Altman DG, NCRRGW Group (2010) Animal research: reporting in vivo experiments: the ARRIVE guidelines. Br J Pharmacol 160:1577–1579
Latz E, Xiao TS, Stutz A (2013) Activation and regulation of the inflammasomes. Nat Rev Immunol 13:397–411
Lu A, Magupalli VG, Ruan J, Yin Q, Atianand MK, Vos MR, Schroder GF, Fitzgerald KA, Wu H, Egelman EH (2014) Unified polymerization mechanism for the assembly of ASC-dependent inflammasomes. Cell 156:1193–1206
Malhotra S, Rio J, Urcelay E, Nurtdinov R, Bustamante MF, Fernandez O, Oliver B, Zettl U, Brassat D, Killestein J, Lechner-Scott J, Drulovic J, Chan A, Martinelli-Boneschi F, Garcia-Merino A, Montalban X, Comabella M (2015) NLRP3 inflammasome is associated with the response to IFN-beta in patients with multiple sclerosis. Brain 138:644–652
Mifflin KA, Kerr BJ (2016) Pain in autoimmune disorders. J Neurosci Res 95(6):1282–1294
Ming X, Li W, Maeda Y, Blumberg B, Raval S, Cook SD, Dowling PC (2002) Caspase-1 expression in multiple sclerosis plaques and cultured glial cells. J Neurol Sci 197:9–18
National Health and Medical Research Council (NHMRC) (2013) Australian code of practice for the care and use of animals for scientific purposes, 8th edn. NHMRC, Canberra
O’Connor AB, Schwid SR, Herrmann DN, Markman JD, Dworkin RH (2008) Pain associated with multiple sclerosis: systematic review and proposed classification. Pain 137:96–111
Osterberg A, Boivie J, Thuomas KA (2005) Central pain in multiple sclerosis-prevalence and clinical characteristics. Eur J Pain 9:531–542
Patti CL, Frussa-Filho R, Silva RH, Carvalho RC, Kameda SR, Takatsu-Coleman AL, Cunha JLS, Abílio VC (2005) Behavioral characterization of morphine effects on motor activity in mice. Pharmacol Biochem Behav 81:923–927
Puthenparampil M, Poggiali D, Causin F, Rolma G, Rinaldi F, Perini P, Gallo P (2016) Cortical relapses in multiple sclerosis. Mult Scler 22:1184–1191
Solaro C, Trabucco E, Messmer Uccelli M (2013) Pain and multiple sclerosis: pathophysiology and treatment. Curr Neurol Neurosci Rep 13:320–329
Vande Walle L, Van Opdenbosch N, Jacques P, Fossoul A, Verheugen E, Vogel P, Beyaert R, Elewaut D, Kanneganti TD, Van Loo G, Lamkanfi M (2014) Negative regulation of the NLRP3 inflammasome by A20 protects against arthritis. Nature 512:69–73
Weber KT, Alipui DO, Sison CP, Bloom O, Quraishi S, Overby MC, Levine M, Chahine NO (2016) Serum levels of the proinflammatory cytokine interleukin-6 vary based on diagnoses in individuals with lumbar intervertebral disc diseases. Arthritis Res Ther 18:3
Wei H, Hu C, Xie J, Yang C, Zhao Y, Guo Y, Mei Z, Chen L, Lan Z (2014) Doliroside A attenuates monosodium urate crystals-induced inflammation by targeting NLRP3 inflammasome. Eur J Pharmacol 740:321–328
Zhou Y, Lu M, Du RH, Qiao C, Jiang CY, Zhang KZ, Ding JH, Hu G (2016) MicroRNA-7 targets Nod-like receptor protein 3 inflammasome to modulate neuroinflammation in the pathogenesis of Parkinson’s disease. Mol Neurodegener 11:28
Acknowledgements
This work was supported by an Australian Research Council (ARC) Linkage Grant [LP120200623] and by a National Health and Medical Research Council (NHMRC) Grant [APP1059239]. The authors also acknowledge the Queensland Government Smart State Research Programme for supporting CIPDD research infrastructure. CIPDD is also supported by Therapeutic Innovation Australia (TIA). TIA is supported by the Australian Government through the National Collaborative Research Infrastructure Strategy (NCRIS) program. We also gratefully acknowledge Avril A.B. Robertson for formulating MCC950 and Ruby Pelingon and Mark Butler for conducting the LC-MS/MS of MCC950 in RR-EAE-mouse plasma samples at the Institute for Molecular Bioscience (IMB), The University of Queensland, Australia.
Author information
Authors and Affiliations
Contributions
NK and AK contributed to the research design and performance of the in vivo experiments. NK performed the data analysis of the in vivo experiments and drafted the manuscript; DB performed in vitro experiments and the associated data analysis. The study was conceived and supervised by MS and MC. All authors edited, read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Professor Matt Cooper is CEO and a shareholder in Inflazome Ltd. This company is developing drugs to address clinical unmet needs in inflammatory disease by targeting inflammasomes. All other authors have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.

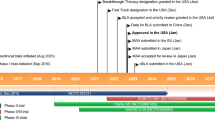
Fig. S1
Optimisation of the anti-allodynic dose of MCC950 in our optimised RR-EAE-mouse model of MS-neuropathic pain. The RR-EAE mice, but not sham mice, developed robust mechanical allodynia in the bilateral hindpaws (mean PWT ≤ 1 g) by day 14 (p.i.) that was persistent in vehicle-treated RR-EAE mice until study completion (day 36 p.i.). By contrast, mechanical allodynia in the bilateral hindpaws of RR-EAE treated with oral MCC950 at 20 mg kg−1 day−1 for days 16–26 p.i. followed by 50 mg kg−1 day−1 for days 27–36 p.i. was significantly attenuated compared with vehicle (PBS)-treated RR-EAE. The higher dose of MCC950 (50 mg kg−1 day−1) produced more robust anti-allodynic effects in RR-EAE mice, such that PWTs in these mice were comparable to sham mice by study completion on day 36 p.i.. The shaded area highlights the chronic MCC950 or vehicle treatment period (days 16–36 p.i.). PWT at or below the horizontal dotted line (PWT ≤ 1 g) indicates fully developed mechanical allodynia. Vertical dotted line indicating day 27, whereby RR-EAE mice receiving MCC950 at 50 mg kg−1 day−1 for 10 days. *P ≤ 0.05 (two-way ANOVA, post hoc: Bonferroni). EAE, experimental autoimmune encephalomyelitis; g, gram; kg, kilogram; mg, milligram; PWT, Paw withdrawal threshold; p.i., post-immunisation (JPEG 216 kb)

Fig. S2
Impact of repeated oral dosing of MCC950 (20–50 mg kg−1 day−1) on the mild relapsing–remitting (RR) disease course in our optimised RR-EAE-mouse model of MS-neuropathic pain. In RR-EAE mice, but not sham mice, the onset of clinical disease (mean score ≥ 0.5 a.u.) was evident by day 4 p.i. followed by consecutive episodes of relapse (mean score ≥ 1 a.u.) and remission (mean score < 0.5 a.u.). This RR-EAE disease course was not changed significantly (P > 0.05) by oral MCC950 at 20 mg kg−1 day−1 for days 16–26 (p.i.) followed by 50 mg kg−1 day−1 for days 27–36 (p.i.) in a manner similar to vehicle-treated RR-EAE mice. The shaded area highlights the chronic treatment (MCC950 or vehicle) period (days 16–36 p.i.). *P ≤ 0.05 (two-way ANOVA, post hoc: Bonferroni). a.u., arbitrary units; EAE, experimental autoimmune encephalomyelitis; kg, kilogram; mg, milligram; PWT, Paw withdrawal threshold; p.i., post-immunisation (JPEG 294 kb)

Fig. S3
Mean (± SEM) plasma concentrations of TNF-α, IL-5, and CXCL1 in RR-EAE mice treated with chronic oral dosing of MCC950 at 50 mg kg−1 day−1 for 21 consecutive days (days 16–36 p.i.). Treatment of RR-EAE mice with MCC950 did not significantly alter the plasma cytokine concentrations at the four timepoints investigated, i.e., day 0, 15, 25, and 36 post-immunisation compared with vehicle-treated RR-EAE mice. The only exception was that the IL-5 concentration was significantly lower in the RR-EAE mice assigned to MCC950 treatment group compared with the vehicle group at day 0. *P ≤ 0.05 (one-way ANOVA with Tukey’s multiple comparison test). pg, picogram; mL, millilitre (JPEG 273 kb)
Table S1
Individual plasma concentrations of IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-10, and IL-12p70 on Day 0 in RR-EAE mice treated chronically with MCC950 at 50 mg.kg−1.day−1 from day 16 to day 36 p.i.; †, plasma pooled from multiple mice; ND, not determinable as value was below the standard curve range (DOCX 16 kb)
Table S2
Individual plasma concentrations of IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-10, and IL-12p70 on Day 15 p.i. in RR-EAE mice treated chronically with MCC950 at 50 mg.kg−1.day−1 from day 16 to day 36 p.i.; †, plasma pooled from multiple mice; ND, not determinable as value was below the standard curve range (DOCX 16 kb)
Table S3
Individual plasma concentrations of IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-10, and IL-12p70 on Day 25 p.i. in RR-EAE mice treated chronically with MCC950 at 50 mg.kg−1.day−1 from day 16 to day 36 p.i.; †, plasma pooled from multiple mice; ND, not determinable as value was below the standard curve range (DOCX 16 kb)
Table S4
Individual plasma concentrations IFN-γ, IL-1β, IL-2, IL-4, IL-6, IL-10, and IL-12p70 on Day 36 p.i. in RR-EAE mice treated with chronically with MCC950 at 50 mg.kg−1.day−1 from day 16 to day 36 p.i.; †, plasma pooled from multiple mice; ND, not determinable as value was below the standard curve range (DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Khan, N., Kuo, A., Brockman, D.A. et al. Pharmacological inhibition of the NLRP3 inflammasome as a potential target for multiple sclerosis induced central neuropathic pain. Inflammopharmacol 26, 77–86 (2018). https://doi.org/10.1007/s10787-017-0401-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-017-0401-9