Abstract
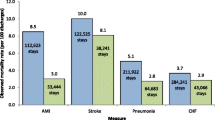
The hospitals selected by or for Medicare beneficiaries might depend on whether the patient is enrolled in a Medicare Advantage (MA) plan. A theoretical model of profit maximization by MA plans takes into account the tradeoffs of consumer preferences for annual premium versus outcomes of care in the hospital and other attributes of the plan. Hospital discharge databases for 13 states in 2006, maintained by the Agency for Healthcare Research and Quality, are the main source of data. Risk-adjusted mortality rates are available for all non-maternity adult patients in each of 15 clinical categories in about 1,500 hospitals. All-adult postoperative safety event rates covering 9 categories of events are calculated for surgical cases in about 900 hospitals. Instrumental variables are used to address potential endogeneity of the choice of a MA plan. The key findings are these: enrollees in MA plans tend to be treated in hospitals with lower resource cost and higher risk-adjusted mortality compared to Fee-for-Service (FFS) enrollees. The risk-adjusted mortality measure is about 1.5 percentage points higher for MA plan enrollees than the overall mean of 4%. However, the rate of safety events in surgical patients favors MA plan enrollees—the rate is 1 percentage point below the average of 3.5%. These discrepant results are noteworthy and are plausibly due to greater discretion by the health plan in approving patients for elective surgery and as well as selecting hospitals for surgical patients. Emergency patients are generally excluded for the safety outcome measures. In addition, the current mortality measures may not adequately represent all surgical patients. Such caveats should be prominently highlighted when presenting comparative data. With that proviso, the study justifies informing Medicare beneficiaries about the mortality and safety outcome measures for hospitals being used by a MA plan compared to hospitals used by FFS enrollees.
Similar content being viewed by others
References
Agency for Healthcare Research and Quality, US DHHS. (2008). 2007 National Healthcare Quality Report, AHRQ Publication No. 08-0040.
Averill R. (2000) Development of the All Patient Refined DRGs (APR-DRGs). 3M Inc. HIS Research Report; 8-97: 1–22
Brenner, M. H. (June 1984). Estimating the effects of economic change on national health and social well-being. Joint economic committee of the US congress. Washington, DC: Government Printing Office.
Brown R. (1987) Biased selection in the Medicare competition demonstrations, Report prepared for the health care financing administration. Princeton, NJ, athematica Policy Research
Eggers P. W., Prihoda R. (1982) Pre-enrollment reimbursement patterns of Medicare beneficiaries enrolled in “at-risk” HMOs. Health Care Financing Review 4: 55–72
Elixhauser A., Steiner C., Harris R., Coffey R. M. (1998) Comorbidity measures for use with administrative data. Medical Care 36: 8–27
Encinosa W., Hellinger F. (2008) The impact of medical errors on 90-day costs and outcomes: An examination of surgical patients. Health Services Research 43(6): 2067–2085
Escarce J. J., Van Horn R. L., Pauly M., Willians S. V., Shea J. A., Chen W. (1999) Health maintenance organizations and hospital quality for coronary artery bypass surgery. Medical Care Research and Review 56(3): 340–362
Friedman, B., Jiang, H. J., & Russo, C. A. (2008). Medicare hospital stays: Comparisons between the fee-for-service plan and alternative plans, 2006. HCUP Statistical Brief #66. January 2009. Agency for Healthcare Research and Quality, Rockville, MD. Mhttp://www.hcup-us.ahrq.gov/reports/statbriefs/sb66.pdf. Accessed 15 April 2009.
Friedman B., Encinosa W., Jiang H. J., Mutter R. (2009) Do patient safety events increase readmissions?. Medical Care 47(5): 1–8
Glied S. (2000) Managed care. In: Culyer A., Newhouse J. P. (eds) Handbook of health economics (Vol. 1). Elsevier, New York
Greene W. H. (2000) Econometric analysis (Chap. 9.5.2, 4th ed.). Prentice Hall, Upper Saddle River, New Jersey
Hansen L. (1982) Large sample properties of generalized method of moments estimators. Econometrica 70(1): 163–189
Luft H.S. (2003) Variations in patterns of care and outcomes after acute myocardial infarction for Medicare beneficiaries in fee-for-service and HMO settings. Health Services Research 38(4): 1065–1079 plus S1-S12
McDonald, K. M., Romano, P. S., Geppert, J., Davies, S., Duncan, B. W., & Shojania, K. G. (2002). Measures of patient safety based on hospital administrative data-the patient safety indicators. Technical Review 5, (Prepared under Contract No. 290-97-0013). AHRQ Publication No. 02-0038.
Mello M. M., Stearns S. C., Norton E. C. (2002) Do Medicare HMOs still reduce health services use after controlling for selection bias?. Health Economics 11: 323–340
Romano P. S., Geppert J. J., Davies S., Miller M. R., Elixhauser A., McDonald K. M. (2003) A national profile of patient safety in US hospitals. Health Affairs 22(2): 154–166
US Congressional Budget Office. (2007). Statement of Peter Orszag, Director, before the Senate Finance Committee, published 4/11/2007.
Zhan C., Miller M. R. (2003) Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. Journal of the American Medical Association 290(14): 1868–1874
Zhan C., Friedman B., Mosso A., Pronovost P. (2006) Medicare payment for adverse events under the prospective payment system: Building the business case for investing in patient safety improvement. Health Affairs 25(5): 1386–1393
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Friedman, B., Jiang, H.J. Do Medicare Advantage enrollees tend to be admitted to hospitals with better or worse outcomes compared with fee-for-service enrollees?. Int J Health Care Finance Econ 10, 171–185 (2010). https://doi.org/10.1007/s10754-010-9076-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-010-9076-0