Abstract
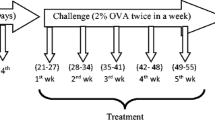
Allergic asthma is an inflammatory condition accompanied by inflammation as well as oxidative stress. Supplementation of an anti-inflammatory agent having antioxidant properties may have therapeutic effects against this disease. Over the recent decades, the interest in combination therapy as new alternative medication has increased and it offers numerous benefits along with noticeable lack of toxicity as well as side effects. In this study, protective effects of curcumin alone and in combination with piperine were evaluated in mouse model of allergic asthma. Balb/c mice were sensitized on days 0, 7, and 14 and challenged from days 16–30 on alternate days with ovalbumin (OVA). Mice were pretreated with curcumin (Cur; 10 and 20 mg/kg) and piperine (Pip; 5 mg/kg) alone and in combination via the intraperitoneal route on days 16–30 and compared with intranasal curcumin (5 mg/kg) treatment. Blood, bronchoalveolar lavage fluid (BALF), and lungs were collected after mice were sacrificed on day 31st. Mice immunized with OVA have shown significant increase in airway inflammation and oxidative stress as determined by oxidative stress markers. A significant suppression was observed with all the treatments, but intranasal curcumin treatment group has shown maximum suppression. So, among all the treatment strategies utilized, intranasal curcumin administration was most appropriate in reducing inflammation and oxidative stress and possesses therapeutic potential against allergic asthma. Present study may prove the possibility of development of curcumin nasal drops towards treatment of allergic asthma.










Similar content being viewed by others
References
Braman, S.S. 2006. The global burden of asthma. Chest 130: 4–12.
Dworski, R. 2000. Oxidant stress in asthma. Thorax 55: 51–53.
Calhoun, W.J., H.E. Reed, D.R. Moest, and C.A. Stevens. 1992. Enhanced superoxide production by alveolar macrophages and air-space cells, airway inflammation, and alveolar macrophage density changes after segmental antigen bronchoprovocation in allergic subjects. The American Review of Respiratory Research 145: 317–325.
Sedgwick, J.B., K.M. Geiger, and W.W. Busse. 1990. Superoxide generation by hypodense eosinophils from patients with asthma. American Review of Respiratory Disease 142: 120–125.
Vachier, I., M. Damon, C. Le Doucen, A.C. De Paulet, P. Chanez, F.B. Michel, and P. Godard. 1992. Increased oxygen species generation in blood monocytes of asthmatic patients. American Review of Respiratory Disease 146: 1161–1168.
Hulsmann, A.R., H.R. Raatgeep, J.C. Den Hollander, T.H.E.O. Stijnen, P.R. Saxena, K.F. Kerrebijn, and J.C. de Jongste. 1994. Oxidative epithelial damage produces hyperresponsiveness of human peripheral airways. American Journal of Respiratory and Critical Care Medicine 149: 519–525.
Franco, R., A.C. Santos, H.F. do Nascimento, C. Souza-Machado, E. Ponte, A. Souza-Machado, S. Loureiro, M.L. Barreto, L.C. Rodrigues, and A.A. Cruz. 2007. Cost-effectiveness analysis of a state funded programme for control of severe asthma. Bio Med Central Public Health 7: 82.
Kumar, D., V. Arya, R. Kaur, Z.A. Bhat, V.K. Gupta, and V. Kumar. 2012. A review of immunomodulators in the Indian traditional health care system. Journal of Microbiology, Immunology and Infection 45: 165–184.
Manson, M. M., P. B. Farmer, A. Gescher, and W. P. Steward. 2005. Innovative agents in cancer prevention. In Tumor Prevention and Genetics III. Springer, Berlin, Heidelberg 257–275.
World Health Organization. 2008. Traditional Medicine Fact Sheet No. 134.
Aggarwal, B. B., Y. J. Surh, and S. Shishodia. 2007.Curcumin: The indian solid gold. The molecular targets and therapeutic uses of curcumin in health and disease. Springer Science & Business Media 595
Sandur, S.K., H. Ichikawa, M.K. Pandey, A.B. Kunnumakkara, B. Sung, G. Sethi, and B.B. Aggarwal. 2007. Role of pro-oxidants and antioxidants in the anti-inflammatory and apoptotic effects of curcumin (diferuloylmethane). Free Radical Biology and Medicine 43: 568–580.
Reyes-Gordillo, K., J. Segovia, M. Shibayama, P. Vergara, M.G. Moreno, and P. Muriel. 2007. Curcumin protects against acute liver damage in the rat by inhibiting NF-κB, proinflammatory cytokines production and oxidative stress. Biochimica et Biophysica Acta (BBA)-General Subjects 1770: 989–996.
Xia, Y., L. Jin, B. Zhang, H. Xue, Q. Li, and Y. Xu. 2007. The potentiation of curcumin on insulin-like growth factor-1 action in MCF-7 human breast carcinoma cells. Life Sciences 80: 2161–2169.
Polasa, K., A.N. Naidu, I. Ravindranath, and K. Krishnaswamy. 2004. Inhibition of B (a) P induced strand breaks in presence of curcumin. Mutation Research/Genetic Toxicology and Environmental Mutagenesis 557: 203–213.
Ammon, H.P., and M.A. Wahl. 1991. Pharmacology of Curcuma longa. Planta Medica 57: 1–7.
Lee, S.A., S.S. Hong, X.H. Han, J.S. Hwang, G.J. Oh, K.S. Lee, M.K. Lee, B.Y. Hwang, and J.S. Ro. 2005. Piperine from the fruits of piper longum with inhibitory effect on monoamine oxidase and antidepressant-like activity. Chemical and Pharmaceutical Bulletin 53: 832–835.
Pradeep, C.R., and G. Kuttan. 2002. Effect of piperine on the inhibition of lung metastasis induced B16F-10 melanoma cells in mice. Clinical & Experimental Metastasis 19: 703–708.
Panda, S., and A. Kar. 2003. Piperine lowers the serum concentrations of thyroid hormones, glucose and hepatic 5′ D activity in adult male mice. Hormone and Metabolic Research 35: 523–526.
Koul, I.B., and A. Kapil. 1993. Evaluation of the liver protective potential of piperine, an active principle of black and long peppers. Planta Medica 59: 413–417.
Atal, C.K., R.K. Dubey, and J. Singh. 1985. Biochemical basis of enhanced drug bioavailability by piperine: evidence that piperine is a potent inhibitor of drug metabolism. Journal of Pharmacology and Experimental Therapeutics 232: 258–262.
Reen, R.K., D.S. Jamwal, S.C. Taneja, J.L. Koul, R.K. Dubey, F.J. Wiebel, and J. Singh. 1993. Impairment of UDP-glucose dehydrogenase and glucuronidation activities in liver and small intestine of rat and guinea pig in vitro by piperine. Biochemical Pharmacology 46: 229–238.
Shoba, G., D. Joy, T. Joseph, M. Majeed, R. Rajendran, and P.S.S.R. Srinivas. 1998. Influence of piperine on the pharmacokinetics of curcumin in animals and human volunteers. Planta Medica 64: 353–356.
Subhashini, P., S. Chauhan, S. Kumari, J.P. Kumar, R. Chawla, D. Dash, M. Singh, and R. Singh. 2013. Intranasal curcumin and its evaluation in murine model of asthma. International Immunopharmacology 17: 733–743.
Chauhan, P.S., D. Dash, and R. Singh. 2014. Intranasal curcumin attenuates airway remodeling in murine model of chronic asthma. International Immunopharmacology 21: 63–75.
Kumari, A., D. Dash, and R. Singh. 2015. Lipopolysaccharide (LPS) exposure differently affects allergic asthma exacerbations and its amelioration by intranasal curcumin in mice. Cytokine 76: 334–342.
Karaman, M., F. Firinci, S. Cilaker, P. Uysal, K. Tugyan, O. Yilmaz, N. Uzuner, and O. Karaman. 2012. Anti-inflammatory effects of curcumin in a murine model of chronic asthma. Allergologia et Immunopathologia 40: 210–214.
Bishnoi, M., K. Chopra, L. Rongzhu, and S.K. Kulkarni. 2011. Protective effect of curcumin and its combination with piperine (bioavailability enhancer) against haloperidol-associated neurotoxicity: cellular and neurochemical evidence. Neurotoxicity Research 20: 215–225.
Kim, S.H., and Y.C. Lee. 2009. Piperine inhibits eosinophil infiltration and airway hyperresponsiveness by suppressing T cell activity and Th2 cytokine production in the ovalbumin-induced asthma model. Journal of Pharmacy and Pharmacology 61: 353–359.
Ram, A., M. Das, and B. Ghosh. 2003. Curcumin attenuates allergen-induced airway hyperresponsiveness in sensitized guinea pigs. Biological and Pharmaceutical Bulletin 26: 1021–1024.
Sahiner, U.M., E. Birben, S. Erzurum, C. Sackesen, and O. Kalayci. 2011. Oxidative stress in asthma. World Allergy Organization Journal 4: 151–158.
Kirkham, P., and I. Rahman. 2006. Oxidative stress in asthma and COPD: antioxidants as a therapeutic strategy. Pharmacology & Therapeutics 111: 476–494.
Parra, A., M.L. Sanz, L. Vila, I. Prieto, I. Dieguez, and A.K. Oehling. 1999. Eosinophil soluble protein levels, eosinophil peroxidase and eosinophil cationic protein in asthmatic patients. Journal of Investigational Allergology & Clinical Immunology 9: 27.
Platts-Mills, T.A. 2001. The role of immunoglobulin E in allergy and asthma. American Journal of Respiratory and Critical Care Medicine 164: 1–5.
Cho, Y.S., and H.B. Moon. 2010. The role of oxidative stress in the pathogenesis of asthma. Allergy, Asthma & Immunology Research 2: 183–187.
Wood, L.G., P.G. Gibson, and M.L. Garg. 2003. Biomarkers of lipid peroxidation, airway inflammation and asthma. European Respiratory Journal 21: 177–186.
Acknowledgements
The authors are thankful to Prof. Dash for providing spectrofluorometer facility to analyze reactive oxygen species (ROS) by using DCF-DA fluorescence at the Department of Biochemistry, Institute of Medical Sciences, Banaras Hindu University, Varanasi. We are also thankful to University Grants Commission (UGC), DST-Science and Engineering Research Board (DST-SERB), and Council of Scientific and Industrial Research (CSIR), New Delhi, India for financial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study design was approved by the Institutional Animal Ethical Committee, Banaras Hindu University, Varanasi.
Rights and permissions
About this article
Cite this article
Chauhan, P.S., Jaiswal, A., Subhashini et al. Combination Therapy with Curcumin Alone Plus Piperine Ameliorates Ovalbumin-Induced Chronic Asthma in Mice. Inflammation 41, 1922–1933 (2018). https://doi.org/10.1007/s10753-018-0836-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-018-0836-1