ABSTRACT
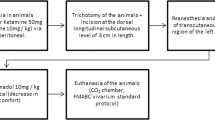
The purpose of this study was to evaluate transcutaneous electrical nerve stimulation (TENS) and other common treatment methods used in the process of wound healing in terms of the expression levels of pro-inflammatory cytokines. In the study, 24 female and 24 male adult Wistar–Albino rats were divided into five groups: (1) the non-wounded group having no incision wounds, (2) the control group having incision wounds, (3) the TENS (2 Hz, 15 min) group, (4) the physiological saline (PS) group and (5) the povidone iodine (PI) group. In the skin sections, interleukin-1 beta (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α) were assessed with enzyme-linked immunosorbent assay and immunohistochemical methods. In the non-wounded group, the expression of IL-1β, IL-6, and TNF-α signaling molecules was weaker in the whole tissue; however, in the control group, significant inflammatory response occurred, and strong cytokine expression was observed in the dermis, granulation tissue, hair follicles, and sebaceous glands (P < 0.05). In the TENS group, the decrease in TNF-α, IL-1β, and IL-6 immunoreaction in the skin was significant compared to the other forms of treatment (P < 0.05). Distinctive decreases of pro-inflammatory cytokines observed in the dermis in the TENS group suggest that TENS shortened the healing process by inhibating the inflammation phase.






Similar content being viewed by others
REFERENCES
Singer, A.J., and R.A.F. Clark. 1999. Cutaneous wound healing. The New England Journal of Medicine 341: 738–746.
Schaffer, M., and A. Barbul. 1998. Lymphocyte function in wound healing and following injury. The British Journal of Surgery 85: 444–460.
Heo, S.C., E.S. Jeon, I.H. Lee, H.S. Kim, M.B. Kim, and J.H. Kim. 2011. Tumor necrosis factor-α-activated human adipose tissue-derived mesenchymal stem cells accelerate cutaneous wound healing through paracrine mechanisms. The Journal of Investigative Dermatology 131: 1559–1567.
Efron, P., and L. Moldawer. 2004. Cytokines and wound healing: the role of cytokine and anticytokine therapy in the repair response. Journal of Burn Care and Research 25: 149.
Werner, S., and R. Grose. 2003. Regulation of wound healing by growth factors and cytokines. Physiological Reviews 83: 835–870.
Alvarez, O.M., P.M. Mertz, R.V. Smerbeck, and W.H. Eaglstein. 1983. The healing of superficial skin wounds is stimulated by external electrical current. The Journal of Investigative Dermatology 81: 144–148.
Brown, M., M.K. McDonnell, and D.N. Menton. 1989. Polarity effects on wound healing using electric stimulation in rabbits. Archives of Physical Medicine and Rehabilitation 70: 624–627.
Stromberg, B.V. 1988. Effects of electrical currents on wound contraction. Annals of Plastic Surgery 21: 121–123.
Kjartansson, J., T. Lundeberg, U.E. Samuelson, and C.J. Dalsgaard. 1988. Transcutaneous electrical nerve stimulation (TENS) increases survival of ischaemic musculocutaneous flaps. Acta Physiologica Scandinavica 13: 95–99.
Koca Kutlu, A., D. Ceçen, S.G. Gürgen, O. Sayın, and F. Cetin. A comparison study of growth factor expression following treatment with transcutaneous electrical nerve stimulation, saline solution, povidone–ıodine, and lavender oil in wounds healing. Evidence-based complementary and alternative medicine: eCAM 2013; 361832. doi:10.1155/2013/361832.
Morgan, D.A. 1999. Wound management products in the Drug Tariff. The Pharmaceutical Journal 263: 820–825.
Jacobson, S. 2004. The wrong solution. Emergency Medicine 36: 13.
Huxtable, K. 1993. Ritual cleansing. Nursing New Zealand 1: 14–16.
Kramer, S.A. 1999. Effect of povidone–iodine on wound healing: a review. Journal of Vascular Nursing 17: 17–23.
Vermeulen, H., S.J. Westerbos, and D.T. Ubbink. 2010. Benefit and harm of iodine in wound care: a systematic review. The Journal of Hospital Infection 76: 191–199.
Goldenheim, P.D. 1993. An appraisal of povidone iodin and wound healing. Post Graduate Medical Journal 69: 97–105.
Lineaweaver, W., R. Howard, D. Soucy, S. McMorris, J. Freeman, C. Crain, J. Robertson, and T. Rumley. 1985. Topical antimicrobial toxicity. Archives of Surgery 120: 267–270.
Burks, R.I. 1998. Povidone–iodine solution in wound treatment. Physical Therapy 78: 212–218.
Kondo, T., and T. Ohshima. 1996. The dynamics of inflammatory cytokines in the healing process of mouse skin wound: a preliminary study for possible wound age determination. International Journal of Legal Medicine 108: 231–236.
Lusby, P.E., A.L. Coombes, and J.M. Wilkinson. 2006. A comparison of wound healing following treatment with Lavandula x allardii honey or essential oil. Phytotherapy Research 20: 755–757.
Gürgen, S.G., D. Erdoğan, C. Elmas, G.T. Kaplanoğlu, and C. Ozer. 2013. Chemoprotective effect of ascorbic acid, α-tocopherol, and selenium on cyclophosphamide-induced toxicity in the rat ovarium. Nutrition 16: 1–8.
Cheing, G.L., and C.W. Hui-Chan. 1999. Transcutaneous electrical nevre stimulation: nonparallel antinociceptive effects on chronic clinical pain and acute experimental pain. Archives of Physical Medicine and Rehabilitation 80: 305–312.
Scudds, R.J., A. Helewa, and R.A. Scudds. 1995. The effects of transcutaneous electrical nerve stimulation on skin temperature in assintomatic subjects. Physical Therapy 75: 622–628.
Kaada, B., E. Olsen, and O. Eielsen. 1984. In search of mediators of skin vasodilation induced by transcutaneous nerve stimulation: III. Increase in plasma VIP in normal subjects and in Raynaud's disease. General Pharmacology 15: 107–113.
Cosmo, P., H. Svensson, S. Bornmyr, and S. Wikström. 2000. Effects of transcutaneous nerve stimulation on the microcirculation in chronic leg ulcers. Scandinavian Journal of Plastic and Reconstructive Surgery and Hand Surgery 34: 61–64.
Cramp, A.F.L., C. Gilsenan, A.S. Lowe, and D.M. Walsh. 2000. The effect of high- and low-frequency transcutaneous electrical nevre stimulation upon cutaneous blood flow and skin temperature in healthy subjects. Clinical Physiology 20: 150–157.
Kloth, L.C., and J.M. McCulloch. 1996. Promotion of wound healing with electrical stimulation. Advances in Skin and Wound Care 9: 42–45.
Sebastian, A., F. Syed, D. Perry, V. Balamurugan, J. Colthurst, I.H. Chaudhry, and A. Bayat. 2011. Acceleration of cutaneous healing by electrical stimulation: degenerate electrical waveform down-regulates inflammation, up-regulates angiogenesis and advances remodeling in temporal punch biopsies in a human volunteer study. Wound Repair and Regeneration 19: 693–708.
Khalil, Z., and M. Merhi. 2000. Effects of aging on neurogenic vasodilator responses evoked by transcutaneous electrical nerve stimulation: relevance to wound healing. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 55: 257–263.
Liebano, R.E., L.E. Abla, and L.M. Ferreira. 2008. Effect of low-frequency transcutaneous electrical nerve stimulation (TENS) on the viability of ischemic skin flaps in the rat: an amplitude study. Wound Repair and Regeneration 16: 65–69.
Khalil, Z., and R.D. Helme. 1996. Sensory peptides as neuromodulators of wound healing in aged rats. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 51: 354–361.
Barrientos, S., O. Stojadinovic, M.S. Golinko, H. Brem, and M. Tomic-Canic. 2008. Growth factors and cytokines in wound healing. Wound Repair and Regeneration 16: 585–601.
Zhou, L.J., R. Matsui, and I. Ono. 2000. Development of a chronic skin defect model and a study of cytokine secretion using the model. Wound Repair and Regeneration 8: 304–318.
Mast, B.A., and G.S. Schultz. 1996. Interactions of cytokines, growth factors, and proteases in acute and chronic wounds. Wound Repair and Regeneration 4: 411–420.
Mateo, R.B., J.S. Reichner, and J.E. Albina. 1994. Interleukin-6 activity in wounds. The American Journal of Physiology 266: 1840–1844.
Akira, S., and T. Kishimoto. 1992. IL-6 and NF-IL6 in acute-phase response and viral infection. Immunological Reviews 127: 25–50.
Lin, Z.Q., T. Kondo, Y. Ishida, T. Takayasu, and N. Mukaida. 2003. Essential involvement of IL-6 in the skin wound-healing process as evidenced by delayed wound healing in IL-6-deficient mice. Journal of Leukocyte Biology 73: 713–721.
Hübner, G., M. Brauchle, H. Smola, M. Madlener, R. Fässler, and S. Werner. 1996. Differential regulation of pro-inflammatory cytokines during wound healing in normal and glucocorticoid-treated mice. Cytokine 8: 548–556.
Locksley, R.M., N. Killeen, and M.J. Lenardo. 2001. The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell 104: 487–501.
Sainson, R.C., D.A. Johnston, H.C. Chu, M.T. Holderfield, M.N. Nakatsu, S.P. Crampton, J. Davis, E. Conn, and C.C. Hughes. 2008. TNF primes endothelial cells for angiogenic sprouting by inducing a tip cell phenotype. Blood 111: 4997–5007.
Cassatella, M.A. 1999. Neutrophil-derived proteins: selling cytokines by the pound. Advances in Immunology 73: 369–509.
Ries, C., V. Egea, M. Karow, H. Kolb, M. Jochum, and P. Neth. 2007. MMP-2, MT1-MMP, and TIMP-2 are essential for the invasive capacity of human mesenchymal stem cells: differential regulation by inflammatory cytokines. Blood 109: 4055–4063.
Grellner, W., T. Georg, and J. Wilske. 2000. Quantitative analysis of proinflammatory cytokines (IL-1beta, IL-6, TNF-alpha) in human skin wounds. Forensic Science International 113: 251–264.
ACKNOWLEDGMENTS
We appreciate the assistance of Celal Bayar of the University Scientific Research Center for provision of financial support for this study. This study was supported by Scientific Research Projects Committee of Celal Bayar University, and No. 2010-31.
CONFLICT OF INTEREST
None of the authors declared any conflict of interests with financial and personal relationships with other people or organizations that could inappropriately influence (bias) our work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gürgen, S.G., Sayın, O., Çetin, F. et al. Transcutaneous Electrical Nerve Stimulation (TENS) Accelerates Cutaneous Wound Healing and Inhibits Pro-inflammatory Cytokines. Inflammation 37, 775–784 (2014). https://doi.org/10.1007/s10753-013-9796-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-013-9796-7