Abstract
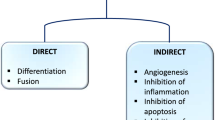
A growing body of evidence supports the hypothesis that autocrine and paracrine mechanisms, mediated by factors released by the resident cardiac cells, could play an essential role in the reparative process of the failing heart. Such signals may influence the function of cardiac stem cells via several mechanisms, among which the most extensively studied are cardiomyocyte survival and angiogenesis. Moreover, besides promoting cytoprotection and angiogenesis, paracrine factors released by resident cardiac cells may alter cardiac metabolism and extracellular matrix turnover, resulting in more favorable post-injury remodeling. It is reasonable to believe that critical intracellular signals are activated and modulated in a temporal and spatial manner exerting different effects, overall depending on the microenvironment changes present in the failing myocardium. The recent demonstration that chemically, mechanically or genetically activated cardiac cells may release peptides to protect tissue against ischemic injury provides a potential route to achieve the delivery of specific proteins produced by these cells for innovative pharmacological regenerative therapy of the heart. It is important to keep in mind that therapies currently used to treat heart failure (HF) and leading to improvement of cardiac function fail to induce tissue repair/regeneration. As a matter of facts, if specific autocrine/paracrine cell–derived factors that improve cardiac function will be identified, pharmacological-based therapy might be more easily translated into clinical benefits than cell-based therapy. This review will focus on the recent development of potential pharmacologic targets to promote and drive at molecular level the cardiac repair/regeneration in HF.



Similar content being viewed by others
References
Jessup M, Brozena S (2003) Heart failure. N Engl J Med 348(20):2007–2018
Bergmann O, Bhardwaj RD, Bernard S et al (2009) Evidence for cardiomyocyte renewal in humans. Science 324(5923):98–102
Segers VF, Lee RT (2008) Stem-cell therapy for cardiac disease. Nature 451(7181):937–942
Herrmann JL, Abarbanell AM, Weil BR, Wang Y, Wang M, Tan J, Meldrum DR (2009) Cell-based therapy for ischemic heart disease: a clinical update. Ann Thorac Surg 88(5):1714–1722
Chachques JC (2009) Cellular cardiac regenerative therapy in which patients? Expert Rev Cardiovasc Ther 7(8):911–919
Menasche P (2009) Cell-based therapy for heart disease: a clinically oriented perspective. Mol Ther 17(5):758–766
Zsolt B, Kaley G (2009) Where have all stem cells gone? Circ Res 104:280–281
Leiker M, Suzuki G, Iyer VS, Canty JMJ, Lee T (2008) Assessment of a nuclear affinity labeling method for tracking implanted mesenchymal stem cells. Cell Transplant 17:911–922
Breitbach M, Bostani T, Roell W et al (2007) Potential risks of bone marrow cell transplantation into infarcted hearts. Blood 110:1362–1369
Barbash IM, Chouraqui P, Baron J et al (2003) Systemic delivery of bone marrow-derived mesenchymal stem cells to the infarcted myocardium: feasibility, cell migration, and body distribution. Circulation 108:863–868
Gnecchi M, Zhang Z, Ni A, Dzau VJ (2008) Paracrine mechanisms in adult stem cell signaling and therapy. Circ Res 103:1204–1219
Gnecchi M, He H, Noiseux N et al (2006) Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. FASEB J 20:661–669
Lin H, Shabbir A, Molnar M, Yang J, Marion S, Canty JMJ, Lee T (2008) Adenoviral expression of vascular endothelial growth factor splice variants differen-tially regulate bone marrow-derived mesenchymal stem cells. J Cell Physiol 216:458–468
Shabbir A, Zisa D, Suzuki G, Lee T (2009) Heart failure therapy mediated by the trophic activities of bone marrow mesenchymal stem cells: a noninvasive therapeutic regimen. Am J Physiol Heart Circ Physiol 296(6):H1888–H1897
Ince H, Petzsch M, Kleine HD et al (2005) Preservation from left ventricular remodeling by front-integrated revascularization and stem cell liberation in evolving acute myocardial infarction by use of granulocyte colony-stimulating factor (FIRSTLINE-AMI). Circulation 112:3097–3106
Saxena A, Fish JE, White MD et al (2008) Stromal cell-derived factor-1alpha is cardioprotective after myocardial infarction. Circulation 117(17):2224–2231
Hamada H, Kim MK, Iwakura A et al (2006) Estrogen receptors alpha and beta mediate contribution of bone marrow-derived endothelial progenitor cells to functional recovery after myocardial infarction. Circulation 114(21):2261–2270
Forini F, Lionetti V, Ardehali H et al. (2010) Early long-term L-T3 replacement rescues mitochondria and prevents ischemic cardiac remodeling in rats. J Cell Mol Med. doi:10.1111/j.1582-4934.2010.01014.x
Lionetti V, Cantoni S, Cavallini C et al. (2010) Hyaluronan mixed esters of butyric and retinoic acid affording myocardial survival and repair without stem cell transplantation. J Biol Chem. doi:10.1074/jbc.M109.087254
Dhalla NS, Saini-Chohan HK, Rodriguez-Leyva D et al (2009) Subcellular remodeling may induce cardiac dysfunction in congestive heart failure. Cardiovasc Res 81(3):429–438
St John Sutton M, Ghio S, Plappert T et al (2009) Cardiac resynchronization induces major structural and functional reverse remodeling in patients with New York Heart Association class I/II heart failure. Circulation 120(19):1858–1860
Qanud K, Mamdani M, Pepe M et al (2008) Reverse changes in cardiac substrate oxidation in dogs recovering from heart failure. Am J Physiol Heart Circ Physiol 295(5):2098–2105
Zacà V, Brewer R, Khanal S et al (2007) Left atrial reverse remodeling in dogs with moderate and advanced heart failure treated with a passive mechanical containment device: an echocardiographic study. J Card Fail 13(4):312–317
Lionetti V, Linke A, Chandler MP et al (2005) Carnitine palmitoyl transferase-I inhibition prevents ventricular remodeling and delays decompensation in pacing-induced heart failure. Cardiovasc Res 66(3):454–461
Zentilin L, Puligadda U, Lionetti V et al. (2009) Cardiomyocyte VEGFR-1 activation by VEGF-B induces compensatory hypertrophy and preserves cardiac function after myocardial infarction. FASEB J. doi:10.1096/fj.09-143180
Ventura C, Cantoni S, Bianchi F et al (2007) Hyaluronan mixed esters of butyric and retinoic Acid drive cardiac and endothelial fate in term placenta human mesenchymal stem cells and enhance cardiac repair in infarcted rat hearts. J Biol Chem 282(19):14243–14252
Ventura C, Maioli M, Asara Y et al (2005) Turning on stem cell cardiogenesis with extremely low frequency magnetic fields. FASEB J 19(1):155–157
Lionetti V, Fittipaldi A, Agostini S, Giacca M, Recchia FA, Picano E (2009) Enhanced caveolae-mediated endocytosis by diagnostic ultrasound in vitro. Ultrasound Med Biol 35(1):136–143
Wang BW, Hung HF, Chang H, Kuan P, Shyu KG (2007) Mechanical stretch enhances the expression of resist in gene in cultured cardiomyocytes via tumor necrosis factor-alpha. Am J Physiol Heart Circ Physiol 293(4):H2305–H2312
Linke WA (2008) Sense and stretchability: the role of titin and titin-associated proteins in myocardial stress-sensing and mechanical dysfunction. Cardiovasc Res 77(4):637–648
Lange S, Ehler E, Gautel M (2006) From A to Z and back? Multicompartment proteins in the sarcomere. Trends Cell Biol 16:11–18
Krüger M, Kötter S, Grützner A et al (2009) Protein kinase G modulates human myocardial passive stiffness by phosphorylation of the titin springs. Circ Res 104(1):87–94
Daniels LB, Maisel AS (2007) Natriuretic peptides. J Am Coll Cardiol 50:2357–2368
Rastaldo R, Pagliaro P, Cappello S, Penna C, Mancardi D, Westerhof N, Losano G (2007) Nitric oxide and cardiac function. Life Sci 81:779–793
Mizote I, Yamaguchi O, Hikoso S et al (2010) Activation of MTK1/MEKK4 induces cardiomyocyte death and heart failure. J Mol Cell Cardiol 48(2):302–309
Shahbazian MD, Grunstein M (2007) Functions of site-specific histone acetylation and deacetylation. Annu Rev Biochem 76:75–100
Bush EW, McKinsey TA (2009) Targeting histone deacetylases for heart failure. Expert Opin Ther Targets 13(7):767–784
Premont RT, Gainetdinov RR (2007) Physiological roles of G protein-coupled receptor kinases and arrestins. Annu Rev Physiol 69:511–534
Rockman HA, Koch WJ, Lefkowitz RJ (2002) Seven-transmembrane-spanning receptors and heart function. Nature 415:206–212
Martini JS, Raake P, Vinge LE et al (2008) Uncovering G protein-coupled receptor kinase-5 as a histone deacetylase kinase in the nucleus of cardiomyocytes. Proc Natl Acad Sci USA 105(34):12457–12462
Chang S, McKinsey TA, Zhang CL, Richardson JA, Hill JA, Olson EN (2004) Histone deacetylases 5 and 9 govern responsiveness of the heart to a subset of stress signals and play redundant roles in heart development. Mol Cell Biol 24(19):8467–8476
Makino S, Fukuda K, Miyoshi S et al (1999) Cardiomyocytes can be generated from marrow stromal cells in vitro. J Clin Invest 103(5):697–705
Hare JM, Chaparro SV (2008) Cardiac regeneration and stem cell therapy. Curr Opin Organ Transplant 13(5):536–542
Yun BG, Matts RL (2005) Differential effects of Hsp90 inhibition on protein kinases regulating signal transduction pathways required for myoblast differentiation. Exp Cell Res 307(1):212–223
Xaymardan M, Cimini M, Fazel S et al (2009) c-Kit function is necessary for in vitro myogenic differentiation of bone marrow hematopoietic cells. Stem Cells 27(8):1911–1920
Roussel M, Moreau P, Huynh A et al (2010) Bortezomib and high dose melphalan as conditioning regimen before autologous stem cell transplantation in patients with de novo multiple myeloma: a phase II study of the Intergroupe Francophone du Myelome (IFM). Blood 115(1):32–37
Erker T, Schreder ME, Studenik C (2000) Studies on the chemistry of thienoannelated O,N- and S,N- containing heterocycles. Part 19: thieno[2,3-b][1,4]thiazines with calcium antagonistic and potassium opening activities. Arch Pharm (Weinheim) 333(2-3):58–62
Wei L, Malhotra SV (2009) Recent development of cyclic amide (Pyridone/Lactam) moiety containing heterocycles as protein kinase inhibitors. Curr Med Chem 17(3):234–253
Desbordes SC, Placantonakis DG, Ciro A, Socci ND, Lee G, Djaballah H, Studer L (2008) High-throughput screening assay for the identification of compounds regulating self-renewal and differentiation in human embryonic stem cells. Cell Stem Cell 2(6):602–612
Hou J, Charters AM, Lee SC et al (2007) A systematic screen for genes expressed in definitive endoderm by serial analysis of gene expression (SAGE). BMC Dev Biol 7:92
Butler GS, Overall CM (2009) Proteomic identification of multitasking proteins in unexpected locations complicates drug targeting. Nat Rev Drug Discov 8(12):935–948
Ventura C, Maioli M, Asara Y et al (2004) Butyric and retinoic mixed ester of hyaluronan. A novel differentiating glycoconjugate affording a high throughput of cardiogenesis in embryonic stem cells. J Biol Chem 279(22):23574–23579
Beltrami AP, Urbanek K, Kajstura J et al (2001) Evidence that human cardiac myocytes divide after myocardial infarction. N Engl J Med 344(23):1750–1757
Ventura C, Guarnieri C, Vaona I, Campana G, Pintus G, Spampinato S (1994) Dynorphin gene expression and release in the myocardial cell. J Biol Chem 269(7):5384–5386
Ventura C, Zinellu E, Maninchedda E, Maioli M (2003) Dynorphin B is an agonist of nuclear opioid receptors coupling nuclear protein kinase C activation to the transcription of cardiogenic genes in GTR1 embryonic stem cells. Circ Res 92(6):623–629
Weil J, Zolk O, Griepentrog J, Wenzel U, Zimmermann WH, Eschenhagen T (2006) Alterations of the preproenkephalin system in cardiac hypertrophy and its role in atrioventricular conduction. Cardiovasc Res 69(2):412–422
Ventura C, Zinellu E, Maninchedda E, Fadda M, Maioli M (2003) Protein kinase C signaling transduces endorphin-primed cardiogenesis in GTR1 embryonic stem cells. Circ Res 92(6):617–622
Ventura C, Pintus G, Vaona I, Bennardini F, Pinna G, Tadolini B (1995) Phorbol ester regulation of opioid peptide gene expression in myocardial cells. Role of nuclear protein kinase. J Biol Chem 270(50):30115–30120
Re RN, Cook JL (2008) The physiological basis of intracrine stem cell regulation. Am J Physiol Heart Circ Physiol 295(2):H447–H453
Wu X, Ding S, Ding Q, Gray NS, Schultz PG (2004) Small molecules that induce cardiomyogenesis in embryonic stem cells. J Am Chem Soc 126(6):1590–1591
Kuhn B, Del Monte F, Hajjar RJ et al (2007) Periostin induces proliferation of differentiated cardiomyocytes and promotes cardiac repair. Nat Med 13:962–969
Bersell K, Arab S, Haring B, Kuhn B (2009) Neuregulin1/ErbB4 signaling induces cardiomyocyte proliferation and repair of heart injury. Cell 138:257–270
Novoyatleva T, Diehl F, van Amerongen MJ et al (2010) TWEAK is a positive regulator of cardiomyocyte proliferation. Cardiovasc Res 85:681–690
Hellström M, Johansson B, Engström-Laurent A (2006) Hyaluronan and its receptor CD44 in the heart of newborn and adult rats. Anat Rec A Discov Mol Cell Evol Biol 288(6):587–592
Rodgers LS, Lalani S, Hardy KM et al (2006) Depolymerized hyaluronan induces vascular endothelial growth factor, a negative regulator of developmental epithelial-to-mesenchymal transformation. Circ Res 99(6):583–589
Gao F, Yang CX, Mo W, Liu YW, He YQ (2008) Hyaluronan oligosaccharides are potential stimulators to angiogenesis via RHAMM mediated signal pathway in wound healing. Clin Invest Med 31(3):E106–E116
Lee JL, Wang MJ, Chen JY (2009) Acetylation and activation of STAT3 mediated by nuclear translocation of CD44. J Cell Biol 185(6):949–957
Heo H, Yoo L, Shin KS, Kang J (2009) Suppression of caspase-11 expression by histone deacetylase inhibitors. Biochem Biophys Res Commun 378(1):79–83
Rochais F, Mesbah K, Kelly RG (2009) Signaling pathways controlling second heart field development. Circ Res 104(8):933–942
Engel FB, Hsieh PC, Lee RT, Keating MT (2006) FGF1/p38 MAP kinase inhibitor therapy induces cardiomyocyte mitosis, reduces scarring, and rescues function after myocardial infarction. Proc Natl Acad Sci USA 103:15546–15551
Fuller SJ, Sivarajah K, Sugden PH (2008) ErbB receptors, their ligands, and the consequences of their activation and inhibition in the myocardium. J Mol Cell Cardiol 44:831–854
Crisan M, Yap S, Casteilla L et al (2008) A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell 3:301–313
Popescu LM, Gherghiceanu M, Manole CG, Faussone-Pellegrini MS (2000) Cardiac renewing: interstitial Cajal-like cells nurse cardiomyocyte progenitors in epicardial stem cell niches. J Cell Mol Med 13:866
Son BR, Marquez-Curtis LA, Kucia M et al (2006) Migration of bone marrow and cord blood mesenchymal stem cells in vitro is regulated by stromal-derived factor-1-CXCR4 and hepatocyte growth factor-c-met axes and involves matrix metalloproteinases. Stem Cells 24:1254–1264
Napoli C, Maione C, Schiano C, Fiorito C, Ignarro LJ (2007) Bone marrow cell-mediated cardiovascular repair: potential of combined therapies. Trends Mol Med 13:278–286
Kawakami M, Tsutsumi H, Kumakawa T et al (1990) Levels of serum granulocyte colony stimulating factor in patients with infections. Blood 76:1962–1964
Leone AM, Rutella S, Bonanno G et al (2006) Endogenous G-CSF and CD34(+) cell mobilization after acute myocardial infarction. Int J Cardiol 111:202–208
Wojakowski W, Tendera M, Michalowska A et al (2004) Mobilization of CD34/CXCR4+, CD34/CD117+, c-met+ stem cells, and mononuclear cells expressing early cardiac, muscle, and endothelial markers into peripheral blood in patients with acute myocardial infarction. Circulation 110:3213–3220
Bussolino F, Wang JM, Defilippi P et al (1989) Granulocyte- and granulocyte macrophage-colony stimulating factors induce human endothelial cells to migrate and proliferate. Nature 337:471–473
Bussolino F, Ziche M, Wang JM et al (1991) In vitro and in vivo activation of endothelial cells by colony-stimulating factors. J Clin Invest 87:986–995
Pelletier L, Regnard J, Fellmann D, Charbord P (2000) An in vitro model for the study of human bone marrow angiogenesis: role of hematopoietic cytokines. Lab Invest 80:501–511
Chen X, Kelemen SE, Autieri MV (2004) AIF-1 expression modulates proliferation of human vascular smooth muscle cells by autocrine expression of G-CSF. Arterioscler Thromb Vasc Biol 24:1217–1222
Lee M, Aoki M, Kondo T, Kobayashi K et al (2005) Therapeutic angiogenesis with intramuscular injection of low-dose recombinant granulocyte-colony stimulating factor. Arterioscler Thromb Vasc Biol 25:2535–2541
Buschmann IR, Hoefer IE, van Royen N et al (2001) GM-CSF: a strong arteriogenic factor acting by amplification of monocyte function. Atherosclerosis 159:343–356
Anghelina M, Krishnan P, Moldovan L, Moldovan NI (2006) Monocytes/macrophages cooperate with progenitor cells during neovascularization and tissue repair: conversion of cell columns into fibrovascular bundles. Am J Pathol 168:529–541
Harada M, Qin Y, Takano H et al (2005) G-CSF prevents cardiac remodeling after myocardial infarction by activating the Jak-Stat pathway in cardiomyocytes. Nat Med 11:305–311
Ueda K, Takano H, Hasegawa H et al (2006) Granulocyte colony stimulating factor directly inhibits myocardial ischemia–reperfusion injury through Akt-endothelial NO synthase pathway. Arterioscler Thromb Vasc Biol 26:e108–e113
Kuhlmann MT, Kirchhof P, Klocke R et al (2006) G-CSF/SCF reduces inducible arrhythmias in the infarcted heart potentially via increased connexin43 expression and arteriogenesis. J Exp Med 203:87–97
Miyata S, Takemura G, Kawase Y et al (2006) Autophagic cardiomyocyte death in cardiomyopathic hamsters and its prevention by granulocyte colony-stimulating factor. Am J Pathol 168:386–397
Shimoji K, Yuasa S, Onizuka T et al (2010) G-CSF promotes the proliferation of developing cardiomyocytes in vivo and in derivation from ESCs and iPSCs. Cell Stem Cell 6:227–237
Ausoni S, Sartore S (2009) The cardiovascular unit as a dynamic player in disease and regeneration. Trends Mol Med 15:543–552
Lagos-Quintana M, Rauhut R, Lendeckel W, Tuschl T (2001) Identification of novel genes coding for small expressed RNAs. Science 294:853–858
Baek D, Villen J, Shin C, Camargo FD, Gygi SP, Bartel DP (2008) The impact of microRNAs on protein output. Nature 455:64–71
Terentyev D, Belevych AE, Terentyeva R et al (2009) miR-1 overexpression enhances Ca2+ release and promotes cardiac arrhythmogenesis by targeting PP2A regulatory subunit B56{alpha} and causing CaMKII-dependent hyperphosphorylation of RyR2. Circ Res 104:514–521
van Rooij E, Sutherland LB, Liu N et al (2006) A signature pattern of stress-responsive microRNAs that can evoke cardiac hypertrophy and heart failure. Proc Natl Acad Sci USA 103:18255–18260
Wang S, Aurora AB, Johnson BA et al (2008) The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell 15(2):261–271
Bonauer A, Carmona G, Iwasaki M et al (2009) MicroRNA-92a controls angiogenesis and functional recovery of ischemic tissues in mice. Science 324(5935):1710–1713
Cordes KR, Sheehy NT, White MP et al (2009) miR-145 and miR-143 regulate smooth muscle cell fate and plasticity. Nature 460(7256):705–710
Acknowledgments
This work was supported by intramural funds from the Scuola Superiore Sant’Anna grants and “Bando Giovani Ricercatori RF 2007” from Ministero del Lavoro, della Salute e delle Politiche Sociali, Italy (V.L.), in part from Ministero dell’ Istruzione, dell’ Universita` e della Ricerca, Italy (C.V.). F.A. Recchia is an Established Investigator of the AHA. We are grateful to Dr. Silvia Agostini for her comments and helpful discussion.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lionetti, V., Bianchi, G., Recchia, F.A. et al. Control of autocrine and paracrine myocardial signals: an emerging therapeutic strategy in heart failure. Heart Fail Rev 15, 531–542 (2010). https://doi.org/10.1007/s10741-010-9165-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-010-9165-7