Abstract
Over 1300 federally-qualified health centers (FQHCs) in the US provide care to vulnerable populations in different contexts, addressing diverse patient health and socioeconomic characteristics. In this study, we use data envelopment analysis (DEA) to measure FQHC performance, applying several techniques to account for both quality of outputs and heterogeneity among FQHC operating environments. To address quality, we examine two formulations, the Two-Model DEA approach of Shimshak and Lenard (denoted S/L), and a variant of the Quality-Adjusted DEA approach of Sherman and Zhou (denoted S/Z). To mitigate the aforementioned heterogeneities, a data science approach utilizing latent class analysis (LCA) is conducted on a set of metrics not included in the DEA, to identify latent typologies of FQHCs. Each DEA quality approach is applied in both an aggregated (including all FQHCs in a single DEA model) and a partitioned case (solving a DEA model for each latent class, such that an FQHC is compared only to its peer group). We find that the efficient frontier for the aggregated S/L approach disproportionately included smaller FQHCs, whereas the aggregated S/Z approach’s reference set included many larger FQHCs. The partitioned cases found that both the S/L and S/Z aggregated models disproportionately disfavored (different) members of certain classes with respect to efficiency scores. Based on these results, we provide general insights into the trade-offs of using these two models in conjunction with a clustering approach such as LCA.







Similar content being viewed by others
References
Charnes A, Cooper WW, Rhodes E (1978) Measuring the efficiency of decision making units. Eur J Oper Res 2(6):429–444
Charnes A, Cooper WW, Rhodes E (1981) Evaluating program and managerial efficiency: an application of data envelopment analysis to program follow through. Manag Sci 27(6):668–697
Nunamaker TR (1983) Measuring routine nursing service efficiency: a comparison of cost per patient day and data envelopment analysis models. Health Serv Res 18(2 Pt 1):183–208
Banker RD, Charnes A, Cooper WW (1984) Some models for estimating technical and scale inefficiencies in data envelopment analysis. Manag Sci 30(9):1078–1092
Health Resources and Service Administration (2017) FY 2017 Annual Performance Report. Available online at https://www.hrsa.gov/about/budget/fy17annualperformancereport.pdf Accessed 22 February, 2018
Rosenbaum S (2015) Will health centers go over the “funding cliff”? Milbank Q 93(1):32–35
Marathe S, Wan TTH, Zhang J, Sherin K (2007) Factors influencing community health centers’ efficiency: a latent growth curve modeling approach. J Med Syst 31:365–374
Amico PR, Chilingerian JA, van Hasselt M (2014) Community health center efficiency: the role of grant revenues in health center efficiency. Health Serv Res 49(2):666–682
VanderWielen LM, Ozcan YA (2015) An assessment of the health care safety net: performance evaluation of free clinics. Nonprof Volunt Sec Q 44(3):474–486
Lazarsfeld PF, Henry NW (1968) Latent structure analysis. Houghton Mifflin, Boston
Agrell PJ, Farsi M, Filippini M, Koller M (2013) Unobserved heterogeneous effects in the cost efficiency analysis of electricity distribution systems. CERETH Economics working papers series 13/171, CER-ETH - Center of Economic Research (CER-ETH) at ETH Zurich
Llorca M, Orea L, Pollitt MG (2014) Using the latent class approach to cluster firms in benchmarking: an application to the US electricity transmission industry. Oper Res Perspect 1:6–17
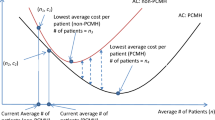
Shimshak D, Lenard ML (2007) A two-model approach to measuring operating and quality efficiency with DEA. INFOR 45(3):143–151
Sherman HD, Zhu J (2006) Benchmarking with quality-adjusted DEA (Q-DEA) to seek lower-cost high-quality service: evidence from a US bank application. Ann Oper Res 145(1):301–319
Emrouznejad A, Yang GL (2017) A survey and analysis of the first 40 years of scholarly literature in DEA: 1978–2016. Socio Econ Plan Sci 61:4–8
Hollingsworth B, Dawson PJ, Maniadakis N (1999) Efficiency measurement of health care: a review of non-parametric methods and applications. Health Care Manag Sc 2(3):161–172
Worthington AC (2004) Frontier efficiency measurement in health care: a review of empirical techniques and selected applications. Med Care Res Rev 61(2):135–170
Hollingsworth B (2008) The measurement of efficiency and productivity of health care delivery. Health Econ 17(10):1107–1128
Ozcan YA (2014) Health care benchmarking and performance evaluation: an assessment using data envelopment analysis (DEA), 2nd edn. Springer, Boston
Sherman HD, Zhu J (2006) Service productivity management: improving service performance using data envelopment analysis (DEA). Springer, New York
DePuccio M, Ozcan YA (2017) Exploring efficiency differences between medical home and non-medical home hospitals. Intl J Heathcare Manage 10(3):147–153
VanderWielen LM, Ozcan YA (2015) An assessment of the healthcare safety net: performance evaluation of free clinics. Nonprof Volunt Sec Q 44(3):474–486
Khushalani J, Ozcan YA (2017) Are hospitals producing quality care efficiently? An analysis using dynamic network data envelopment analysis (DEA). Socio-Econ Plan Sci 60:15–23
Ozcan YA, Khushalani J (2017) Assessing efficiency of public health and medical care provision in OECD countries after a decade of reform. Cent Eur J Oper Res 25(2):325–343
Highfill T, Ozcan YA (2016) Productivity and quality of hospitals that joined the Medicare shared savings accountable care organization program. Intl J Heathcare Manage 9(3):210–217
Nayar P, Ozcan YA, Yu F, Nguyen AT (2013) Benchmarking urban acute care hospitals: efficiency and quality perspectives. Health Care Manage R 38(2):137–145
Mark BA, Jones CB, Lindley L, Ozcan YA (2009) An examination of technical efficiency, quality and patient safety on acute care nursing units. Policy Polit Nurs Pract 10(3):180–186
Rahman MA, Capitman JA (2012) Can more use of supporting primary care health practitioners increase efficiency of health clinics? Evidence from California's San Joaquin Valley. J Health Care Finance 38(3):78–92
Hollingsworth B, Street A (2006) The market for efficiency analysis of health care organisations. Health Econ 15(10):1055–1059
Giuffrida A, Gravelle H (2001) Measuring performance in primary care: econometric analysis and DEA. Appl Econ 33:163–175
Bastian ND, Kang H, Swenson ER, Fulton LV, Griffin PM (2016) Evaluating the impact of hospital efficiency on wellness in the military system. Mil Med 181(8):827–834
Collins LM, Lanza ST (2010) Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. Wiley, Hoboken
McCutcheon AL (1987) Latent class analysis. Sage, Newbury Park
Agresti A (1990) Categorical data analysis. Wiley, New York
Vermunt JK, Magidson J (2002) Latent class cluster analysis. In: Hagenaars J, McCutcheon A (eds) Applied latent class analysis. Cambridge University Press, Cambridge, pp 89–106
Clogg CC (1995) Latent class models: recent developments and prospects for the future. In: Arminger G, Clogg CC, Sobel MW (eds) Handbook of statistical modeling for the social and behavioral sciences. Plenum Press, New York, pp 311–359
Nyland KL, Asparouhov T, Muthén BO (2007) Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model 14(4):535–569
Corbella S, Taschieri S, Del Fabbro M, Francetti L, Weinstein R, Ferrazzi E (2016) Adverse pregnancy outcomes and periodontitis: a systematic review and meta-analysis exploring potential association. Quintessence Int 47(3):193–204
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ (2010) A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 67(10):1012–1024
Kelly RH, Russo J, Holt VL, Danielsen BH, Zatzick DF, Walker E, Katon W (2002) Psychiatric and substance use disorders as risk factors for low birth weight and preterm delivery. Obstet Gynecol 100(2):297–304
Hellström A, Smith LEH, Dammann O (2013) Retinopathy of prematurity. Lancet 382(9902):1445–1457
Zhang S, Cardarelli K, Shim R, Ye J, Booker KL, Rust G (2013) Racial disparities in economic and clinical outcomes of pregnancy among Medicaid recipients. Matern Child Health J 17(8):1518–1525
Chilingerian JA, Sherman HD (2011) Health-care applications: from hospitals to physicians, from productive efficiency to quality frontiers. In: Cooper WW, Seiford LM, Zhu J (eds) Handbook on data envelopment analysis. Springer, Berlin, pp 445–490
Dziak JJ, Coffman DL, Lanza ST, Li R (2012) Sensitivity and specificity of information criteria. The methodology at the Pennsylvania State University. Tech Rep Ser:12–119 https://methodology.psu.edu/media/techreports/12-119.pdf
Chilingerian JA, Sherman HD (1990) Managing physician efficiency and effectiveness in providing hospital services. Health Serv Manag Res 3(1):3–15
Centers for Disease Control (2017) National Center for Health Statistics, Birthweight and Gestation, https://www.cdc.gov/nchs/fastats/birthweight.htm Accessed 22 February 2018
Luo X (2003) Evaluating the profitability and marketability efficiency of large banks an application of data envelopment analysis. J Bus Res 56(8):627–635
Amado CAF, Dyson RG (2008) On comparing the performance of primary care providers. Eur J Oper Res 185(3):915–932
Acknowledgements
Research reported in this publication was supported by the National Institute of General Medical Sciences (NIGMS) of the National Institutes of Health under Award Number 5P20GM104417. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Statistical analyses for data sets
Appendix 2: Algorithms for implementation of S/L and S/Z procedures
Sets:
-
R: DEA production outputs; R = r1,…,r2
-
Q: DEA quality outputs; Q = q1,…,q2
q1: Quality_Access
q2: Quality_LBWI
-
J: FQHCs; J = j1,…,j1111
Parameters:
-
k: iteration counter
-
Ek: number of FQHCs excluded due to iteration k



Rights and permissions
About this article
Cite this article
McGarvey, R.G., Thorsen, A., Thorsen, M.L. et al. Measuring efficiency of community health centers: a multi-model approach considering quality of care and heterogeneous operating environments. Health Care Manag Sci 22, 489–511 (2019). https://doi.org/10.1007/s10729-018-9455-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-018-9455-5