Abstract
Healthcare systems are facing a resources scarcity so they must be efficiently managed. On the other hand, it is commonly accepted that the higher the consumed resources, the higher the hospital production, although this is not true in practice. Congestion on inputs is an economic concept dealing with such situation and it is defined as the decreasing of outputs due to some resources overuse. This scenario gets worse when inpatients’ high severity requires a strict and effective resources management, as happens in Intensive Care Units (ICU). The present paper employs a set of nonparametric models to evaluate congestion levels, sources and determinants in Portuguese Intensive Care Units. Nonparametric models based on Data Envelopment Analysis are employed to assess both radial and non-radial (in)efficiency levels and sources. The environment adjustment models and bootstrapping are used to correct possible bias, to remove the deterministic nature of nonparametric models and to get a statistical background on results. Considerable inefficiency and congestion levels were identified, as well as the congestion determinants, including the ICU specialty and complexity, the hospital differentiation degree and population demography. Both the costs associated with staff and the length of stay are the main sources of (weak) congestion in ICUs. ICUs management shall make some efforts towards resource allocation to prevent the congestion effect. Those efforts shall, in general, be focused on costs with staff and hospital days, although these congestion sources may vary across hospitals and ICU services, once several congestion determinants were identified.

Similar content being viewed by others
Notes
Hereinafter, stars * stand for linear programming models’ variables optima.
ρ0 -* is achieved by minimizing the linear program in Eq. (10), instead of maximizing.
We are aware that data can be somehow old. Still, there is no apparent reason to believe that both congestion sources and the environment impact on congestion could significantly change till the present days.
We do not include “work force” variables, such as number of nurses and doctors, as inputs, once they are multidisciplinary, working in different hospital dimensions, but the information provided by the official sources do not allow to disentangle the staff number working in ICU from other departments.
All required data for this research is available at the official database of the Portuguese Ministry of Health, the Central Administration of Health Systems, cf. http://www.acss.min-saude.pt/, in lawful annual reports of each hospital, and in http://www.pordata.pt/en/Municipalities.
The adjustment for environment (subsection 3.3) shall be enough for inpatients complexity accounting, as claimed by Ferreira and Marques [27].
This results into \( \sqrt[{\vartheta}_w+4]{\frac{16}{n^2{\left({\vartheta}_w+2\right)}^2}}=\sqrt[9+4]{\frac{16}{630^2{\left(9+2\right)}^2}}\approx 0.3175 \), which represents a bandwidth for the multidimensional kernel function.
The authors, using the software Matlab®, developed all computational frameworks.
Multiple optima (solutions) are not problematic in the present case. Indeed, our results are consistent with those ones obtained through the approach proposed by Sueyoshi and Sekitani [31]. However, so as to avoid a too long paper and to keep the analysis as simple as possible, those results are not displayed but can be provided upon request.
Mutatis mutandis, it can be easily adapted to the other two hypotheses.
Abbreviations
- CapC:
-
Capital Costs
- CI:
-
Confidence Interval
- CGSC:
-
Costs of Goods Sold and Consumed
- CRS:
-
Constant Returns to Scale
- DEA:
-
Data Envelopment Analysis
- DMU:
-
Decision Making Unit
- DSE:
-
Degree of Scale Economies
- EPE:
-
Entidade Pública Empresarial
- EU:
-
European Union
- GDP:
-
Gross Domestic Product
- GSI:
-
Gini’s Specialization Index
- HC:
-
Hospital Center
- HospDays:
-
Hospital Day(s)
- ICU:
-
Intensive Care Unit
- InpD:
-
Inpatient Discharge(s)
- LHU:
-
Local Health Unit
- LVP:
-
Law of Variable Proportions
- MP:
-
Marginal Product
- RTS:
-
Returns to Scale
- SA:
-
Sociedade Anónima
- SDH:
-
Strong Disposability Hull
- SEServ:
-
Supplies and External Services
- SH:
-
Singular Hospital
- SMI:
-
Service-Mix Index
- SPA:
-
Serviço Público Administrativo
- StaffC:
-
Staff Costs
- VRS:
-
Variable Returns to Scale
- WDH:
-
Weak Disposability Hull
References
Cooper WW, Seiford LM, Zhu J (2000) A unified additive model approach for evaluating inefficiency and congestion with associated measures in DEA. Socio-Econ Plan Sci 34:1–25
Nayar P, Ozcan YA, Yu F, Nguyen AT (2013) Benchmarking urban acute care hospitals: Efficiency and quality perspectives. Health Care Manag Rev 38(2):137–145
Hsieh HM, Clement DG, Bazzoli GJ (2010) Impacts of market and organizational characteristics on hospital efficiency and uncompensated care. Health Care Manag Rev 35(1):77–87
Kahn JM, Goss CH et al (2006) Hospital volume and the outcomes of mechanical ventilation. N Engl J Med 355(1):41–50
Khandelwal N, Benkeser DC, Coe NB, Curtis JR (2016) Potential Influence of Advance Care Planning and Palliative Care Consultation on ICU Costs for Patients with Chronic and Serious Illness. Crit Care Med 44(8):1474–1481
Halpern NA, Pastores SM, Greenstein RJ (2004) Critical care medicine in the United States 1985-2000: An analysis of bed numbers, use, and costs. Crit Care Med 32(6):1254–1259
Barrett, M.L., Smith, M.W., Elixhauser, A., Honigman, L.S., Pines, J.M., 2014. Utilization of Intensive Care Services, 2011. HCUP Statistical Brief #185. Agency for Healthcare Research and Quality, Rockville. Retrieved from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb185-Hospital-Intensive-Care-Units-2011.jsp, 15th September 2016.
Puig-Junoy J (1998) Technical Efficiency in the Clinal Management of Critically Ill Patients. Health Econ 7:263–277
Tsekouras K, Papathanassopoulos F, Kounetas K, Pappous G (2010) Does the adoption of new technology boost productive efficiency in the public sector? The case of ICUs system. Int J Prod Econ 128:427–433
Dervaux B, Leleu H, Minvielle E, Valdmanis V, Aegerter P, Guidet B (2009) Performance of French intensive care units: A directional distance function approach at the patient level. Int J Prod Econ 120:585–594
Clement J, Valdmanis V, Bazzoli G, Zhao M, Chukmaitov A (2008) Is more, better? An analysis of hospital outcomes and efficiency with a DEA model of output congestion. Health Care Manag Sci 11:67–77
Valdmanis V, Rosko M, Muller R (2008) Hospital quality, efficiency, and input slack differentials. Health Serv Res 43:1830–1848
Ferrier GD, Rosko M, Valdmanis V (2006) Analysis of uncompensated hospital care using a DEA model of output congestion. Health Care Manag Sci 9:181–188
Arrieta A, Guillén J (2015) Output congestion leads to compromised care in Peruvian public hospital neonatal units. Health Care Manag Sci. doi:10.1007/s10729-015-9346-y
Matranga D, Sapienza F (2015) Congestion analysis to evaluate the efficiency and appropriateness of hospitals in Sicily. Health Policy 119(3):324–332
Simões P, Marques RC (2011) Performance and Congestion Analysis of the Portuguese Hospital Services. CEJOR 19:39–63
Mathews KS, Long EF (2015) A Conceptual Framework for Improving Critical Care Patient Flow and Bed Use. Ann Am Thorac Soc 12(6). doi:10.1513/AnnalsATS.201409-419OC
Chan CW, Farias VF, Escobar GJ (2016) The Impact of Delays on Service Times in the Intensive Care Unit. Manag Sci. doi:10.1287/mnsc.2016.2441
Farrell MJ (1957) The measurement of productive efficiency. J R Stat Soc Ser A 120:253–281
Charnes A, Cooper WW, Rhodes E (1978) Measuring efficiency of decision-making units. Eur J Oper Res 2:429–444
Ozcan YA (2008) Health Care Benchmarking and Performance Evaluation: An Assessment using Data Envelopment Analysis (DEA). Springer, New York
Hollingsworth B (2003) Non-parametric and parametric applications measuring efficiency in health care. Health Care Manag Sci 6:203–218
Ruggiero J (2007) A comparison of DEA and the stochastic frontier model using panel data. Int Trans Oper Res 14:259–266
De Witte K, Marques R (2009) Capturing the environment, a metafrontier approach to the drinking water sector. Int Trans Oper Res 16:257–271
Jacobs R, Smith PC, Street A (2006) Measuring Efficiency in Health Care: Analytic Techniques and Health Policy. Cambridge University Press, Cambridge
Hollingsworth B (2008) The Measurement of Efficiency and Productivity of Health Care Delivery. Health Econ 17(10):1107–1128
Ferreira D, Marques RC (2016) Should inpatients be adjusted by their complexity and severity for efficiency assessment? Evidence from Portugal. Health Care Manag Sci 19(1):43–57
Ferreira D, Marques RC (2015) Did the corporatization of Portuguese hospitals significantly change their productivity? Eur J Health Econ 16(3):289–303
Marques RC, Carvalho P (2012) Estimating the efficiency of Portuguese hospitals using an appropriate production technology. Int Trans Oper Res 20(2):1–17
Cooper WW, Seiford LM, Tone K (2007) Data Envelopment Analysis: A Comprehensive Text with Models, Applications, References and DEA-solver Software. Kluwer Academic Publishers, Boston
Sueyoshi T, Sekitani K (2009) DEA congestion and returns to scale under an occurrence of multiple optimal projections. Eur J Oper Res 194(2):592–607
Färe R, Grosskopf S, Lovell CAK (1985) The measurement of efficiency of production. Kluwer-Nijhoff Publishing
Färe R, Grosskopf S, Lovell CAK (1994) Production Frontiers. Cambridge University Press, Cambridge
Färe R, Svensson L (1980) Congestion of production factors. Econometrica 48:1745–1753
Sueyoshi T (2003) DEA Implications of Congestion. Asia Pacific Manag Rev 8(1):59–70
Tone K, Sahoo BK (2004) Degree of scale economies and congestion: a unified DEA approach. Eur J Oper Res 158:755–772
Ferreira, D., Marques, R.C. 2016. Malmquist and Hicks-Moorsteen Productivity Indexes for Clusters Performance Evaluation. International Journal of Information Technology & Decision Making, forthcoming.
Herr A (2008) Cost and technical efficiency of German hospitals: does ownership matter? Health Econ 17(9):1057–1071
Daraio C, Simar L (2007) Advanced robust and nonparametric methods in efficiency analysis: Methodology and applications. Springer Science + Business Media, LLC, New York
Ferreira, D., Marques, R.C., Pedro, I., 2016. Comparing efficiency of holding business model and individual management model of airports. Journal of Air Transport Management, forthcoming
Rego G, Nunes R, Costa J (2010) The challenge of corporatisation: the experience of Portuguese public hospitals. Eur J Health Econ 11:367–381
Ozcan YA, Luke RD (1993) A national study of the efficiency of hospitals in urban markets. Health Serv Res 28(6):719–739
Ozcan YA (1993) Sensitivity analysis of hospital efficiency under alternative output/input and peer groups: a review. Knowl Policy 5(4):1–29
Lobo MSC, Ozcan YA, Lins MPE, Silva ACM, Fiszman R (2014) Teaching hospitals in Brazil: findings on determinants for efficiency. Int J Healthcare Manag 7(1):60–68
Daidone S, D’Amico F (2009) Technical efficiency, specialization and ownership form: evidences from a pooling of Italian hospitals. J Prod Anal 32:203–216
Lindlbauer I, Schreyögg J (2014) The relationship between hospital specialization and hospital efficiency: do different measures of specialization lead to different results? Health Care Manag Sci 17:365–378
Simar L, Wilson PW (1998) Sensitivity analysis of efficiency scores: how to bootstrap in nonparametric frontier models. Manag Sci 44:49–61
Grossman M (1972) On the Concept of Health Capital and the Demand for Health. J Polit Econ 80(2):223–255
Kuntz L, Sülz S (2011) Modeling and notation of DEA with strong and weak disposable outputs. Health Care Manag Sci 14(4):385–388
Acknowledgments
We would like to thank to three anonymous referees who kindly and significantly have improved this paper’s quality, clarity and structure, due to their beneficial comments. We also acknowledge the financial support of the Portuguese Foundation for Scientific and Technology (FCT): SFRH/BD/113038/2015. The second author thanks the FCT (Portuguese national funding agency for science, research and technology) for the possibility of being under sabbatical leave in the University of Cornell in the USA for the period when part of this research took place.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix
1.1 Literature review
Please, see Table 5
Service-Mix Index
The inefficiency-corrected SMI for the ICU service (DMU0) defined by the pair \( \left({x}_{i0},{y}_{r0}\right)\in {\mathbb{R}}_{+}^{5+1} \) can be computed as follows:
Use Eq. (19) to obtain the optima \( {\left\{{\theta}_0^{*},{p}_1^{-*},\dots, {p}_5^{-*},{p}_1^{+*}\right\}}_{SDH} \) and project (x i0, y r0) in the SDH frontier using the transformation \( \left({\overset{\vee }{x}}_{i0},{\overset{\vee }{y}}_{10}\right)=\left({\theta}_0^{*}\cdot {x}_{i0}-{p}_i^{-*},{y}_{10}+{p}_1^{+*}\right)\in {\mathbb{R}}_{+}^{5+1} \). This projection removes the technical inefficiency of units. To obtain Ω we follow the strategy proposed by subsection 3.3, considering all environment variables but Z6 (by obvious reasons).
-
1)
Re-run the step 1) for all DMUs and obtain the set \( \nabla =\left\{\left({\displaystyle \sum_{i=1}^4}{\overset{\vee }{x}}_{ij},{\overset{\vee }{y}}_{1j}\right)=\left({\theta}_0^{*}\cdot {\displaystyle \sum_{i=1}^4}{x}_{ij}-{\displaystyle \sum_{i=1}^4}{p}_i^{-*},{\overset{\vee }{y}}_{1j}\right)\in {\mathbb{R}}_{+}^2,j=1,\dots, n\right\} \). ∇ only contains data from the single output and the first 4 inputs (monetary resources).
-
2)
Compute the ratio for the j-th unit \( {\boldsymbol{\xi}}_{\boldsymbol{j}}=\left({\displaystyle \sum_{\boldsymbol{i}=1}^4}{\overset{\vee }{\boldsymbol{x}}}_{\boldsymbol{i}\boldsymbol{j}}\right)/{\overset{\vee }{\boldsymbol{y}}}_{1\boldsymbol{j}},\boldsymbol{j}=1,\dots, \boldsymbol{n} \), which represents the efficient unitary cost of such DMU j .
-
3)
Compute \( \mathbf{\mathcal{B}}={\displaystyle \prod_{\boldsymbol{j}=1}^{\boldsymbol{n}}}\left({{\boldsymbol{\xi}}_{\boldsymbol{j}}}^{1/\boldsymbol{n}}\right) \), which represents the unitary costs’ national average (baseline).
-
4)
The SMI for the DMU0 is then SMI0 = ξ0/\( \boldsymbol{\mathcal{B}} \), where \( {\boldsymbol{\xi}}_0=\left({\displaystyle \sum_{\boldsymbol{i}=1}^4}{\overset{\vee }{\boldsymbol{x}}}_{\boldsymbol{i}0}\right)/{\overset{\vee }{\boldsymbol{y}}}_{10} \)
Gini’s Specialization Index
The GSI k for the hospital k is computed as follows, [45, 46]:
-
1)
Let ℒ be the number of Disease Related Groups (DRG);
-
2)
Sort DRGs by discharges treated, in ascending order;
-
3)
Let \( {\mathbf{\mathcal{D}}}_{\boldsymbol{w}}^{\boldsymbol{k}} \) be the number of the w-th DRG group discharges;
-
4)
Let \( {\boldsymbol{q}}_{\boldsymbol{i}}^{\boldsymbol{k}},\boldsymbol{i}=1,\dots, \mathbf{\mathcal{L}}-1 \), be the ratio of total discharges treated by the first i DRGs, i.e., \( {\boldsymbol{q}}_{\boldsymbol{i}}^{\boldsymbol{k}}={\varSigma}_{\ell =1}^i{\mathbf{\mathcal{D}}}_{\ell}^{\boldsymbol{k}}/{\displaystyle \sum_{\boldsymbol{w}=1}^{\mathbf{\mathcal{L}}-1}}{\mathbf{\mathcal{D}}}_{\boldsymbol{w}}^{\boldsymbol{k}} \)
-
5)
Compute GSI k ∈ [0; 1] using Eq. (20).
Bootstrapping
Based on Simar and Wilson [47] and Daraio and Simar [38], the output-oriented bootstrap algorithm is as follows:
-
1)
Compute the n output-oriented DEA efficiency scores, under the strong or the weak disposability assumption, Eqs. (6) and (7), respectively; for the sake of generality, let’s suppose we obtain the set of efficiency scores, Φ = {θ j , j = 1, … , n}, with a standard \( {\sigma}_{\varPhi^{"}} \) deviation and an interquartile range \( {r}_{\varPhi^{"}} \).
-
2)
Reflect Φ and obtain the 2n-length set Φ ' = {2 − θ 1, 2 − θ 2, ... , 2 − θ n , θ 1, θ 2, ... , θ n }.
-
3)
Consider only those p DMUs such that θ b > 1 , b = 1 , . . . , p < n; from Φ′, create the 2p-length set Φ″ = {2 − θ 1, 2 − θ 2, … , 2 − θ p , θ 1, θ 2, … , θ p } ⊂ Φ′;Φ ' ' has a standard deviation \( {\sigma}_{\varPhi^{{\prime\prime} }} \) and an interquartile range r Φ ' '.
-
4)
Compute a bandwidth \( d\approx \left(1.06\cdot {\sigma}_{\boldsymbol{\Phi}}\cdot \min \left\{{\sigma}_{{\boldsymbol{\Phi}}^{\mathbf{{\prime\prime}}}},\kern0.5em \frac{r_{{\boldsymbol{\Phi}}^{\mathbf{{\prime\prime}}}}}{1.34}\right\}{(2p)}^{4/5}\right)/\left(\boldsymbol{n}\cdot {\sigma}_{{\boldsymbol{\Phi}}^{\mathbf{{\prime\prime}}}}\right) \).
-
5)
Randomly (with reposition) draw a n-length sample from Φ' (step 2)) and obtain the set \( {\varPhi}^{\star }=\left\{\tilde{\theta_j^{\star }},\mathrm{j}=1,\dots, n\right\} \), with a standard deviation σ ⋆ and an arithmetic mean m ⋆.
-
6)
Use a perturbation χ j = d ⋅ ζ j , where \( {\boldsymbol{\zeta}}_{\boldsymbol{j}}\sim \mathbf{\mathcal{N}}\left(\boldsymbol{\mu} =0,\boldsymbol{\sigma} =1\right) \), to obtain the set
$$ {\varPhi}^{\star \star }=\left\{\tilde{\theta_j^{\star \star }}=\frac{\tilde{\theta_j^{\star }}+{\chi}_j-{m}^{\star }}{\sqrt{1+{\left(\frac{d}{\&^{\star }}\right)}^2}}+{m}^{\star };\mathrm{s}.t.{\chi}_j=d\cdot {\zeta}_j;{\zeta}_j\sim \mathbf{\mathcal{N}}\left(\mu =0,\sigma =1\right);\mathrm{j}=1,\dots, n;\tilde{\theta_j^{\star }}\in {\varPhi}^{\star}\right\} $$(21) -
7)
Reflect those n units from Φ ⋆⋆, as follows:
$$ {\theta}_j^{\star \star }=\left\{\begin{array}{cc}\hfill 2-\tilde{\theta_j^{\star \star }}\hfill & \hfill if\ \tilde{\theta_j^{\star \star }}<1\hfill \\ {}\hfill \tilde{\theta_j^{\star \star }}\hfill & \hfill otherwise\hfill \end{array}\right. $$(22) -
8)
Create the set \( {\Im}^{\star \star }=\left\{\left({x}_{ij}^{\star },{y}_{rj}^{\star}\right)\in {\mathbb{R}}_{+}^{m+s}:\kern0.5em {x}_{ij}^{\star }={x}_{ij}\cap {y}_{rj}^{\star }={y}_{rj}\frac{\theta_j}{\theta_j^{\star \star }},\mathrm{j}=1,\dots, n\right\} \), and re-run Eqs. (6) and (7) to project units in the new frontier and to obtain the bootstrap-based efficiency scores, under the strong or the weak disposability assumption, resp.
-
9)
Repeat steps 5)-8) B times, where B is large, say B ~ 1,000 iterations.
-
10)
Let m Bj and σ Bj be the arithmetic mean and the standard deviation of those B bootstrap-based efficiency score for unit j. Bias is then bias j ≈ m Bj − θ j and the bias-corrected DEA efficiency score is \( \hat{\theta_j}={\theta}_j-bia{s}_j\approx 2\cdot {\theta}_j-{m}_{Bj} \). Still, this bias correction shall not be performed if |bias j | ≤ σ Bj /4.
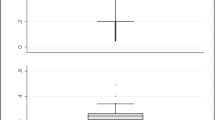
Some additional graphics and tables
Please check Figs. 2, 3, 4 and 5, as well as Tables 6, 7 and 8.
Rights and permissions
About this article
Cite this article
Ferreira, D., Marques, R.C. Identifying congestion levels, sources and determinants on intensive care units: the Portuguese case. Health Care Manag Sci 21, 348–375 (2018). https://doi.org/10.1007/s10729-016-9387-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-016-9387-x