Abstract
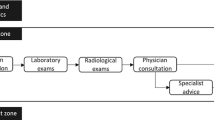
Modeling and analysis of patient flow in hospital emergency department (ED) is of significant importance. In a hospital ED, the patients spend most of their time in the patient room and most of the care delivery services are carried out during this time period. In this paper, we propose a system model to study patient (or work) flow in the patient room of an ED when the resources are partially available. A closed and re-entrant process model is developed to characterize the care service activities in the patient room with limited resources of doctors, nurses, and diagnosis tests. Analytical calculation of patient’s length of stay in the patient room is derived, and monotonic properties with respect to care service parameters are investigated.




Similar content being viewed by others
References
Bernstein SL, Asplin BR (2006) Emergency department crowding: old problems, new solutions. Emerg Med Clin North Am 24(4):821–837
Jayaprakash N et al (2009) Crowding and delivery of healthcare in emergency departments: the european perspective. West J Emerg Med 10(4):233–239
Sacchetti A et al (2002) Contribution of ED admissions to inpatient hospital revenue. Am J Emerg Med 20(1):30–31
Kennedy J et al (2004) Access to emergency care: restricted by long waiting times and cost and coverage concerns. Ann Emerg Med 43(5):567–573
Hoot NR, Aronsky DA (2008) Systematic review of emergency department crowding: causes, effects and solutions. Ann Emerg Med 52(2):126–136
Brenner S et al (2010) Modeling and analysis of the emergency department at university of kentucky chandler hospital using simulations. J Emerg Nurs 36(3):303–310
Zeng Z et al (2012) A simulation study to improve quality of care in the emergency department of a community hospital. J Emerg Nurs 38(3):322–328
Wang J et al (2012) Reducing length of stay in emergency department: a simulation study at a community hospital. IEEE Trans Syst Man Cybern Syst Hum 42(6):1314–1322
Jacobson SH et al (2006) Discrete-event simulation of health care systems. In: Hall RW (ed) Patient flow: reducing delay in healthcare delivery, vol 91. Springer, International Series in Operations Research & Management Science, pp 211–252
Brailsford SC (2007) Advances and challenges in healthcare simulation modeling: tutorial. In: Proceedings of the 39th winter simulation conference, pp 1436–1448
Wiler JL, Griffey RT, Olsen T (2011) Review of modeling approaches for emergency department patient flow and crowding research. Acad Emerg Med 18(12):1371–1379
Fomundam S, Herrmann J (2007) A survey of queuing theory applications in health care. Technicial report No. 2007–24, the Institute for Systems Research, University of Maryland, College Park
Koizumi N (2002) A queueing network model with blocking: analysis of congested patients flows in mental health systems. PhD dissertation, University of Pensylvania, Philadelphia
Caglar T (2005) A queueing theoretic approach to gridlock prediction in emergency departments. Master Thesis, Virginia Polytechnic Institute and State University, Blacksburg
Au L et al (2009) Predicting overflow in an emergency department. IMA J Manag Math 20(1):39–49
Green LV (2006) Queueing analysis in healthcare. In: Hall RW (ed) Patient flow: reducing delay in healthcare delivery, vol 91. Springer, New York, pp 281–308
Green LV et al (2006) Using queueing theory to increase the effectiveness of emergency department provider staffing. Acad Emerg Med 13(1):61–68
Au-Yeung SWM, Harrison PG, Knottenbelt WJ (2007) Approximate queueing network analysis of patient treatment times. In: Proceedings of the 2nd international conference on performance evaluation methodologies and tools. 321 ariticle 45
Mayhew L, Smith D (2008) Using queuing theory to analyse the governments 4-h completion time target in accident and emergency departments. Health Care Manag Sci 11(1):11–21
de Bruin AM et al (2007) Modeling the emergency cardiac in-patient flow: an application of queuing theory. Health Care Manag Sci 10(2):125–137
Saghafian S et al (2012) Complexity-based triage: a tool for improving patient safety and operational efficiency. Ross School of Business Paper No. 1161
Saghafian S et al (2012) Patient streaming as a mechanism for improving responsiveness in emergency departments. Oper Res 60(5):1080–1097
Helm JE, Beygi SA, Van Oyen MP (2012) Design and analysis of hospital admission control for operational effectiveness. Prod Oper Manag 20(3):359–374
Armony M et al (2011) Patient flow in hospitals: a data-based queueing-science perspective. Stoch Syst 6(3)
Li J, Meerkov SM (2009) Production systems engineering. Springer, New York
Liu Y, Li J (2010) Split and merge production systems: performance analysis and structural properties. IIE Trans 42(6):422–434
Biller S et al (2009) Closed Bernoulli production lines: analysis, continuous improvement, and leanness. IEEE Trans Autom Sci Eng 6(1):168–180
Wang C, Li J (2010) Approximate analysis of re-entrant lines with Bernoulli reliability models. IEEE Trans Autom Sci Eng 7(3):708–715
Wang J et al (2012) Modeling and analysis of work flow and staffing level in a computed tomography division of university of wisconsin medical foundation. Health Care Manag Sci 15(2):108–120
Xie X et al (2013) Improving response-time performance in acute care delivery: a systems approach. Conditionally accepted by IEEE Transactions on Automation Science and Engineering
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper is supported in part by NSF Grants No. CMMI 1063671 and 1233807.
Appendix: Proofs
Appendix: Proofs
Proof of Proposition 1
By adding the balance equations and eliminating the identical terms, the process throughput TP follows immediately. The patients may leave the system when they are ready for the second service and the provider is available, i.e.,
From the Little’s law, the length of stay is obtained through the inverse of TP since only one patient is in the system. □
Proof of Corollary 1
Define the steady state probabilities as follows:
By adding Eqs. 1, 2, 3, and 4 with Eqs. 5, 6, 7, and 8, respectively, we obtain
Then, it follows that
Replacing with \(\pi _{i},i=0,1,2,3\) to rewrite Eqs. 1–4, we have
Then, it implies that
where
Since now the matrix dimension is small, it is possible to express its inverse in an explicit format. Thus, after some manipulation, we obtain
where
Then, \(P(1;0,1)=\pi _{5}\) and \(P(1;1,1)=\pi _{7}\) are obtained and \(T_{s}=\frac {1}{c_{2}[P(1;0,1)+P(1;1,1)]}\) can be calculated. □
Rights and permissions
About this article
Cite this article
Wang, J., Li, J. & Howard, P.K. A system model of work flow in the patient room of hospital emergency department. Health Care Manag Sci 16, 341–351 (2013). https://doi.org/10.1007/s10729-013-9235-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-013-9235-1