Abstract
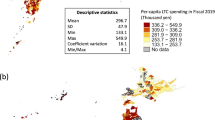
In Stockholm County Council (SLL), budgets for hospital care have been allocated to geographically responsible authorities for a long time. This hospital care includes all publicly financed specialist care, also privately owned hospitals, except private practitioner care. The old needs-index model, a 6D capitation matrix based on demography and socio-economy, was generated on linked individual data for 1994–96. In this paper the power of the old allocation model is evaluated by the use of new data for 2006. The analysis shows that most of the socioeconomic variables have lost their descriptive power in 10 years. Using a methodical search we also find an improved need-based allocation model for hospital care using the new data for 2006. By focusing on costly diagnoses, where the descriptive power has increased between 1996 and 2006, and by using some new socioeconomic variables, and by relying on birth and death prognoses, we are able to generate a matrix model with much higher coefficients-of-determinations in 1 year predictions. In addition, a more careful modelling of multi-morbidity, part-of-the-year inhabitants, episode definition and cost transformation is developed. The area-level cost residuals of registered versus predicted costs show stable signs over the years, indicating unexplained systematics. For the reduction of the residuals, accepting proven inpatient diagnoses but not the full costs, a mixed capitation/fee-for-service strategy is discussed. Once equivalent (e.g. full-year) observations are determined, the link between background and consumption is not on individual-level but on cell-level, as in current resource allocation studies in the United Kingdom.



Similar content being viewed by others
References
Andersson P-Å, Varde E, Diderichsen F (2000) Modelling of resource allocation to health care authorities in Stockholm County. Health Care Manag Sci 3:141–149
Morris RW, Whincup PH, Papacosta O, Walker M, Thomson A (2005) Inequalities in coronary revascularisation during the 1990s: evidence from the British regional heart study. Heart 91:635–640
Carlisle DM, Leake BD (1998) Differences in the effect of patients’ socioeconomic status on the use of invasive cardiovascular procedures across health insurance categories. Am J Pub Health 88(7):1089–1092
Peake MD, Thompson S, Lowe D, Pearson MG (2003) Ageism in the management of lung cancer. Age Ageing 32(2):171–177
Rice N, Smith PC (2002) Strategic resource allocation and funding decisions. In: Mossialos E, Dixon A, Figueras J, Kutzin J (eds) Funding health care: options for Europe. Open University Press, Buckingham, Philadelphia, pp 250–271. www.euro.who.int/__data/assets/pdf_file/0003/98310/E74485.pdf. Accessed 9 September 2010
Iezzoni LI, Ayanian JZ, Bates DW, Burstin HR (1998) Paying more fairly for Medicare capitated care. N Engl J Med 339(26):1933–1938
WHO (1980) International statistical classification of diseases, 9th revision (ICD-9)
Socialstyrelsen. (The national board of health and welfare) (1986) Klassifikation av sjukdomar 1987. (Swedish version of ICD-9). Liber/Allmänna Förlaget, Stockholm
CRC (2008) NHS resource allocation. Commission for Rural Communities, Cheltenham Glos. Tackling rural disadvantage. www.ruralcommunities.gov.uk/files/ResourceAllocation%20Fact%20Sheet%20Tagged.pdf. Accessed 9 September 2010
Sutton M, Gravelle H, Morris S et al (2002) Allocation of resources to English areas, Individual and small area determinants of morbidity and use of healthcare resources. DH Report. www.show.scot.nhs.uk/isd/isd_services. Accessed 9 September 2010
Asthana S, Gibson A, Moon G, Dicker J, Brigham P (2004) The pursuit of equity in NHS resource allocation: should morbidity replace utilisation as the basis for setting health care capitations? Soc Sci Med 58:539–551
Asthana S, Flowers J, Gibson A (2007) Review of the Weighted Capitation Formula, on behalf of the East of England Strategic Health Authority. Univ. of Plymouth and Erpho. www.eoe.nhs.uk/document_store_public/1210754845_xybJ_review_of_the_weighted_capitation_formula.pdf. Accessed 9 September 2010
WHO (2007) International statistical classification of diseases and related health problems, 10th rev (ICD-10). http://apps.who.int/classifications/apps/icd/icd10online/. Accessed 9 September 2010
Socialstyrelsen. (The national board of health and welfare) (1996) Klassifikation av sjukdomar och hälsoproblem 1997. (Swedish version of ICD-10). www.socialstyrelsen.se/publikationer1996/1996-4-1. Accessed 9 September 2010
Vallejo-Torres L, Morris S, Carr-Hill R, Dixon P, Law M, Rice N, Sutton M (2009) Can regional resource shares be based only on prevalence data? An empirical investigation of the proportionality assumption. Soc Sci Med 69:1634–1642
Diderichsen F, Spetz C-L (1987) Behovsbaserad planering inom hälso- och sjukvården. (Needs based planning in healthcare). Memorandum 172/87, Socialstyrelsen, Stockholm.
Statistics Sweden (2008) Longitudinal integration database for health insurance and labour market studies. www.scb.se/Pages/List____257743.aspx. Accessed 9 September 2010
Diderichsen F, Varde E, Whitehead M (1997) Resource allocation to health authorities—the quest for an equitable formula in Britain and Sweden. BMJ 315:875–8
Socialdepartementet. (Ministry of Health and Social Affairs) (1996) HSU 2000, Behov och resurser i vården—en analys. (Needs and resources in healthcare—an analysis). SOU 1996:163, Allmänna Förlaget, Stockholm
Inrikesdepartementet. (Ministry of the Interior) (1998) Kostnadsutjämning för kommuner och landsting—en översyn av statsbidrags- och utjämningssystemet. (Cost compensation for municipalities and county councils—a revision of the governmental subsidy and transfer system). SOU 1998:151, Allmänna Förlaget, Stockholm
Finansdepartementet och Sveriges kommuner och landsting. (Ministry of Finance and Swedish Association of Local Authorities and Regions) (2008) Local government financial equalisation—Information about the equalisation system for Swedish municipalities and county councils in 2008. http://brs.skl.se/publikationer/. Accessed 9 September 2010
Wolff JL, Starfield B, Anderson G (2002) Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med 162:2269–2276
Walander A (2010) Sjukvård under sista levnadstiden: Sociala skillnader i vårdkontakter och vårdkostnader. (Health care during the last year of life: Social differences in healthcare contacts and costs). Rep 2010:1, KI and SLL. www.folkhalsoguiden.se. Accessed 9 September 2010
Stacy EW (1962) A generalization of the Gamma distribution. Ann Math Statist 33(3):1187–1192
Martin-Löf P (1974) The notion of redundancy and its use as a quantitative measure of discrepancy between a statistical hypothesis and a set of observational data. Scand J Statist 1:3–18
SLL (2008) Årsredovisning. (Annual financial report) 2007. Landstingsstyrelsens förvaltning. http://www.sll.se/sll/templates/NormalPage.aspx?id=854. Accessed 9 September 2010
Rice N, Smith PC (2001) Ethics and geographical equity in health care. J Med Ethics 27:256–261
Acknowledgements
The study has been supervised by Prof. Bo Burström, Div. of Social Medicine, Karolinska Institutet (KI), as part of the SLL-KI-common project on the follow-up of resource usage and healthcare on equal conditions.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
1.1 A1 Illustrations of basic variation principles
Focusing on the principles, we choose to consider one healthcare discipline and primarily study the effects of two- versus one-cell matrix models on the HCA-allocations. We use episode def. 1 (see Subsection 3.1) for the comparison of the per capita (one cell) model versus allocations by a 1D-split into two cells (categories/classes) c = 1,2 to an unspecified number of areas a. The number of full-year inhabitants is denoted n ca , with dot-index for sums, e.g.:
The population index for c = 2 is defined as:
where q2a > 1 (<1) means a greater (smaller) proportion of cell-2-individuals in area a than for SLL as a whole.Example A1.1 Let p c denote the risk of healthcare in cell c, and assume (without restriction) p 1 ≥ p 2. The cost-per-episode Y distribution is of an unspecified type F(μ,σ), common to both cells, with E[Y]=μ, V[Y] = σ 2. Constant E[Z] for all allocation models (cf. Subsection 3.1) means \( {n_{ \bullet \bullet }}{p_\bullet } = {n_{1 \bullet }}{p_1} + {n_{2 \bullet }}{p_2} \). The allocation ratio between two-cell and one-cell, based on the expected-values, becomes:
○ If the cell-2-proportions \( {n_{2a}}/{n_{ \bullet a}} \) are constant in each area a (for, e.g., gender), then q 2a = 1 and ρ a = 1, irrespective of
○ If the two risks p c are equal, then ρ a = 1, irrespective of
Hence a two-cell split is motivated, only if both p c and q 2a vary.
-
○ If, e.g., \( {{{{p_1}}} \left/ {{{p_\bullet }}} \right.} = 2 \) and q 2a = 0.75 (or, e.g., \( {{{{p_1}}} \left/ {{{p_\bullet }}} \right.} = 1.5 \) and q 2a = 0.5), then ρ a = 1.25, i.e. two-cell allocates 25% more than one-cell to area a. ■
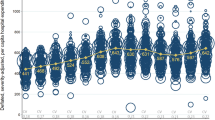
Even for a perfect allocation model the random cost variations may cause drastic deviations from the predicted HCA-costs. The sum of squared such (area-based) deviations is of special interest as a quality measure. By assuming independent outcome-events, the expected sum of squares can be shown to coincide with the total Z-variance, forming the individual-based R2-value. For area-based models R2-values of magnitude 90–99% are frequent (at the calibration) but for individual-based models R2-values of a few percent are normal.
Example A1.1, continued
Let \( \kappa : = \sigma /\mu \) be the coefficient-of-variation. For two-cell and population (distribution) based variances we have:
A high R2-value is favoured by \( {p_1}/{p_\bullet } \) big (good risk discrimination), \( {n_{ \bullet \bullet }}/{n_{1 \bullet }} \approx 1 \) (large population in high-risk cell), κ small (low cost variation), \( {p_\bullet } \) big (overall high risks)—but is unaffected by area properties.
-
○ If, e.g., \( {p_\bullet } = 0.2 \), \( {n_{ \bullet \bullet }}/{n_{1 \bullet }} = 3 \), \( {p_1}/{p_\bullet } = 2p \) and κ = 2, we get R2 = 2%, i.e. modest, but it generates 25% allocation changes for an a with \( {n_{2a}}/{n_{ \bullet a}} = 0.5 \) (see above for q 2a = 0.75).■
Example A1.2
Another special case is a two-cell split based on different cost distributions F c (μ c ,σ c ) for c = 1,2 but a common risk \( {p_\bullet } \). The R2-value becomes (A1.2) with the cell-1-risk ratio \( {p_1}/{p_\bullet } \) replaced by the cost ratio \( \mu /{\mu_\bullet } \). ■
Example A1.3
(A1.2) is not limited to two-cell versus one-cell. Consider a large number of 1D-cells of equal population size (e.g., for income quantiles), with cell risks that vary uniformly between \( {p_1} \) and p 2 (p 1 > p 2). Constant E[Z] means \( {p_\bullet } = ({p_1} + {p_2})/2 \). The quality measure R2 becomes (A1.2) with \( {n_\bullet }/{n_1} = 4 \). ■
The basic cost variation is controlled by the V[Z]-expression in Subsection 3.1; where the two terms measure the relative contributions from the two means of variation, Y and X.
Example A1.4
For the per capita model the relative importance ν of the Y-variation is determined by the ratio \( (1 - {p_\bullet })/{\kappa^2} \), as \( \nu = 1/(1 + (1 - {p_\bullet })/{\kappa^2}) \). Since the healthcare costs vary a lot (cf. Subsection 3.3) we usually have \( \kappa \geqslant {1}\,\,( > \sqrt {{1 - {p_\bullet }}} ) \), i.e. ν > 0.5: the Y-variation dominates. ■
1.2 A2 Poisson-distributed number of episodes per year
Proposition If, in every matrix cell, the number of episodes per year is Poisson-distributed, then—irrespective of the cost-per-episode distribution—we expect the R2-value to be approximately zero.
Proof
Let the stochastic variable (s.v.) Z c denote the patient cost per year, equally distributed for each individual \( i = 1, \ldots, {n_c} \) in matrix cell c, and let E[Z c ], V[Z c ] denote its expected value and variance, respectively. The total variance is:
and for a per capita model, with s.v. \( {Z_\bullet } \) equally distributed for all persons in all cells:
If each E[Z c ] in V[Z] is estimated by the corresponding sample mean value, then one degree of freedom disappears for each cell c, and the unbiased estimators (* indicates s.v.) of the total variances become
For the compound Z c -distribution, composed of the number of episodes per year X c and the patient cost per episode Y c , we have (cf. Subsection 3.1)
If X c is Poisson-distributed, then E[X c ] = V[X c ] and \( V{[}{Z_c}{] = }E{[}{X_c}{]} \cdot E{[}{Y_c}^2{]} \). If E[X c ], \( E{[}{Y_c}^2{]} \) are estimated by the sample mean values:
then:
where the final approximation is motivated by a large sample, such that every \( {n_c} > > 1 \).
Analogously we estimate:
Hence \( {V^* }{[}{\mathbf{Z}}{]} \approx V_{\rm{cap}}^* {[}{\mathbf{Z}}{]} \). The coefficient-of-determination R2-estimator satisfies: \( {(R2)^* }: = 1 - {V^* }{[}{\mathbf{Z}}{]}/V_{\rm{cap}}^* {[}{\mathbf{Z}}{]} \approx {0} \). ■
1.3 A3 Basic χ 2- and redundancy tests
We compare pairs of cells or cell-clusters by asymptotically χ 2-distributed test quantities, and use the property that also sums of χ 2-distributed quantities are χ 2-distributed. Either we form one χ 2-sum for X and Y (cf. Subsection 3.1) together, or two separate sums. Two test options:
Option 1
Expected value comparison. Two cells (or clusters) c = 1,2.
Null hypotheses: E[X 1] = E[X 2], E[Y 1] = E[Y 2].
As for X we consider the samples of sizes n c , averages \( {\bar{X}_c} \) and weighted variance \( S_X^2 \). Let:
We rely on CLT for \( {\bar{X}_c} \), whence \( {Q_X}\sim {\hbox{As}}t(r = {n_1} + {n_2} - 2) \), Student-t. From the distribution relations \( t(r) = N(0,1)/\sqrt {{{\chi^2}(r)/r}} \) and \( {t^2}(r) = {{{{\chi^2}(1)}} \left/ {{{\chi^2}(r)/r}} \right.} = F(1,r) \), Fisher-F, follows \( {Q′_X}(r): = {Q_X}^2\sim {\hbox{As}}F(1,r) \), where F(1,r) approaches χ 2(1) for r big. On behalf of the distribution means, an unbiased test quantity is \( (1 - 2/r) \cdot {Q′_X}(r)\sim {\hbox{As}}{\chi^2}(1) \). Thus each cell-pair comparison contributes 1 d.f. (degree of freedom). For Y a corresponding test quantity is used.
Option 2
χ2 homogeneity test.
For each cell-pair comparison a number r of X-values are distinguished, e.g., x = 0,1+ for r = 2. The Y-distribution is split into r quantiles, e.g., r = 2 above/below the median.
The r values contribute 2 r terms and r-1 d.f.s to the χ 2-sum.
For large samples any χ 2-test leads to significant results, even for the smallest deviations from the null hypothesis. In such cases the redundancy measure [25] is applicable, since it determines whether a model is sufficient for the data description. The redundancy ρ describes the relative entropy H change of a parameter reduction. Its scale is universal, with ρ = 0.01 denoting bad and ρ = 0.001 good, according to [25]. Like F-tests for model comparisons by R2-values, the ρ-tests are for the comparison of two models where one is an extension (as to the parameter set) of the other. For a final model choice, where models A, B of different types are to be compared, we extend the tests as follows. Let \( | \cdot | \) denote cardinality, here the number of parameters, and assume \( |{\mathbf{A}}| > |{\mathbf{B}}| \). For an evaluation of the R2-values of A and B we introduce a fictitious model A base , a simplification of A and equivalent to B in the sense \( R_{{{\mathbf{A}}_{base}}}^2 = R_{\mathbf{B}}^2 \), \( |{{\mathbf{A}}_{base}}| = |{\mathbf{B}}| \), and then compare A, A base as usual. For sample size n, with the null hypothesis that the \( |{\mathbf{A}}| - |{{\mathbf{A}}_{base}}| \) extra parameters equal zero, for the F-like test quantity we get
Analogously, for an entropy comparison we assume \( {H_{{{\mathbf{A}}_{base}}}} = {H_{\mathbf{B}}} \) and compute the redundancy:
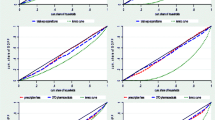
1.4 A4 Generalised Gamma distribution
Y > 0, \( Y\sim {\hbox{GenGamma(}}a,b,c) \), \( \tilde{Y}: = {(Y/a)^{1/b}} \) implies
Density function—see Subsection 3.3. Distribution function:
where \( \tilde{\Gamma } \) is the incomplete Γ-function, with:
The mth statistical moment:
Moment-based estimation: \( \hat{E}[Y] = \bar{y} \), \( \hat{E}[{Y^2}] = \overline {{y^2}} \), where \( \hat{b}: = b \) solves the equation
for fixed c. This determines \( \hat{a} = \bar{y} \cdot \frac{{\Gamma \left( {\hat{b} \cdot (c + 1)} \right)}}{{\Gamma \left( {\hat{b} \cdot (c + 2)} \right)}} \).
Rights and permissions
About this article
Cite this article
Andersson, PÅ., Bruce, D., Walander, A. et al. Time for a new budget allocation model for hospital care in Stockholm?. Health Care Manag Sci 14, 36–55 (2011). https://doi.org/10.1007/s10729-010-9140-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-010-9140-9