Abstract
The sugar moiety of IgA is known to provide a link between the innate and adaptive immune systems. Terminally located glycotopes on IgA are potential ligands engaged in the interactions which may modulate the biological activities of IgA. In the present work the expressions of Maackia amurensis (MAA), Sambucus nigra (SNA), Lens culinaris (LCA), Tetragonolobus purpureus (LTA), and Ulex europaeus (UEA) reactive glycotopes on maternal plasma and amniotic IgA were evaluated in relation to the progression of a normal human pregnancy, from the 2nd trimester, throughout the 3rd trimester, perinatal period, post-date pregnancy and delivery, by lectin-IgA-ELISA, using specific biotinylated lectins. The amniotic and maternal plasma IgA concentrations and a degree of SNA and LCA reactivity of maternal plasma IgA were almost unaltered during the normal pregnancy. The amniotic IgA from the 2nd trimester was decorated by MAA-, SNA-reactive and LCA-, LTA-, and UEA-reactive glycotopes. At the turn of the 2nd and 3rd trimesters the expression of MAA-, SNA-, LTA-, and UEA-reactive glycotopes, except for LCA-reactive, increased and remained almost at unaltered levels throughout the perinatal period and delivery. However, in the post-date pregnancy the expression of LCA-, LTA-, and UEA-reactive and SNA-reactive glycotopes were significantly higher. The unique fucosylated and sialylated glycovariants of amniotic IgA associated with the progression of the normal pregnancy may illustrate a general importance of carbohydrate-lectin receptor interactions in the control and modulation of biological events to ensuring homeostasis during pregnancy, protection and well-being of fetus.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
In the biological development processes the defined oligosaccharide structures appear in specific spatial and temporal patterns [1]. During pregnancy, when intensive growth and development of the fetus occur, glycans terminated with sialic acid and/or fucose are known to control and modulate biological reactions involved in cell-cell signaling, adhesion, and stimulate cell growth and differentiation [2–4]. Additionally, the glycoconjugates bearing sialyl-Lewis antigens participate in the prevention of leucocyte adhesion to the fetal syncytiotrophoblast [5], and can interact with amniotic selectins and play an immunomodulatory role in the late pregnancy [4, 6].
The glycosylation process during the pregnancy is stimulated and controlled by the endocrine changes [7], different sets and ratios of glycosyltransferases produced and activated in many clones of B-cells [8], as well as cytokines (IL-6) [7, 9]. Some glycoproteins of amniotic fluid, such as glycodelin, transferrin [10], human chorionic gonadotropin [11], α1-acid glycoprotein [12], fibronectin [13] and IgG [14], represent different schemes of glycosylation, particulary fucosylation and sialylation, in comparison with the glycoproteins of the maternal serum [4]. Moreover, glycosylation patterns of amniotic glycoproteins are reported to change throughout gestation because of different sites of biosynthesis (maternal, fetal, and placental) at subsequent stages of pregnancy [4, 15, 16].
In human amniotic fluid IgA is much less abundant than IgG. It can originate from maternal, fetal and placental tissues. The share of IgA in amniotic fluid derived from different sites of synthesis (local production in the decidua as well as by fetal mucosa), and forms of its transport (a nonspecific diffusion and receptor-mediated transport of maternal IgA) is known to vary with gestational age [17, 18]. The maternal IgA, like IgG, is potentially available to the embryo as early as on the 6th week of gestation [19]. The placental transfer of IgA starts when the first placental villi are formed and increases as gestation advances [19]. In contrast to IgG, amniotic IgA of fetal origin is more in favor of a preimmune role by natural polyreactive IgA antibodies similar to that reported for secretion [20]. Moreover, IgA in amniotic fluid is involved in the protection of the fetus against maternal IgG autoantibodies [21]. According to Quan et al. [18] the amniotic immunoglobulins, both IgG and IgA, can serve as a protection against pathogens and act through mechanisms similar to those observed in the female genital fluid. The amniotic pool of IgA, similarly to the serum IgA [22], consists mainly of monomeric form with a low level of secretory IgA (SIgA), and with various amounts of free secretory component (SC) [18]. Additionally, an unusual form of fetal immunoglobulins, absent in the maternal serum, was observed. This molecule contains no α chain but includes a Fabγ fragment non-covalently associated with SC and can act as an immune barrier against the infection and against autoantibodies derived from the mother [18].
Immunoglobulins A, besides their high molecular heterogeneity related to the fact that they can exist as monomers, dimers and oligomers, and additionally in IgA1and IgA2 subclasses, and as a SIgA, occur in diverse glycoforms with the attached N- and O-glycans. The sugar part of IgA depends on the origin, meaning the systemic and mucosal immune systems [23, 24], and ranges from 6 % for serum IgA up to 25 % for secretory component (SC) [22, 25, 26]. IgA1, IgA2 and SIgA may carry distinct populations of N- and/or O-glycan structures, in part as the result of different glycosylation machinery for epithelial and plasma cells [22, 25–27]. Royle et al. [25] have reported that a secretory component of colostrum SIgA contains α1,4-, α1,3-, and α1,2- fucosylated and α2,3-sialylated glycans that are decoys for pathogens binding to mucosal surfaces. The glycosylation pattern of amniotic IgA during the pregnancy has not yet been elucidated and thus is of major interest since it is associated with different origins and functions.
In our study, we analyze the alternations in the expression of MAA- and SNA-reactive glycotopes and LCA-, LTA-, and UEA-reactive glycotopes of IgA in amniotic fluid during the normal human pregnancy from the 2nd trimester, throughout the 3rd trimester, perinatal period, post-date pregnancy and delivery. The levels of sialylation and fucosylation of the IgA were determined by lectin-IgA-ELISA using lectins with known specificity toward different types of sialic acid and fucose linkages Table 1 [28–32]. The sialylation and fucosylation patterns were determined on plasma and amniotic IgA, isolated by modified polyclonal anti-α chain antibodies. It should be pointed out that this approach did not determine the ‘true’ structure of the human IgA glycans, but allowed to observe the changes of glycotope expressions accessible to the interactions with lectins. Such glycan-lectin interactions between the lectin-receptors and the sialyl- and fucosyl-glycotopes are emerging as key elements in a wide range of pathophysiological processes.
Materials and methods
Patients and sampling
Samples of amniotic fluid (101) and blood plasma (101) were obtained from pregnant women (21–38 years old) with gestational age between 14 and 42 weeks, receiving prenatal care at the Department of Obstetrics and Gynaecology, Wroclaw Medical University, Wrocław, Poland. During the 2nd and 3rd trimesters, the amniotic fluid was taken by transabdominal amniocentesis under ultrasonographic guidance, and during delivery by transvaginal amniotomy. The samples used for the current study consisted of the fluid remaining after the performance of the routine diagnostic procedures. At 14–18 weeks of gestation, amniotic fluid was obtained by amniocentesis for fetal karyotyping. In all cases, an accurate gestational dating was established by obtaining knowledge about the most recent menstrual period and confirmed by the ultrasonographic evaluation. There were no signs of inflammation, vaginal infection, or chorioamnionitis. All samples were collected after the informed consent of the individual women, and the study was approved by the local ethics committee (no. KB-479/2006). Immediately after amniocentesis, all amniotic fluid samples were centrifuged at 3000xg for 20 min to separate cells from the supernatant, and then aliquoted and stored at −76 °C until use. The frozen samples were thawed at 20 °C before use. Amniotic fluid samples contaminated with blood or meconium were discarded.
The samples of amniotic fluid and plasma were divided into the following groups:
-
1)
The second trimester, n = 21: 14–18 weeks of pregnancy;
-
2)
The third trimester, n = 12: 35–37 weeks of pregnancy;
-
3)
Perinatal period, n = 11: 38–40 weeks of pregnancy;
-
4)
Delivery, n = 40: 38–42 weeks of pregnancy. Fetuses were delivered by spontaneous vaginal delivery within 3 h; and
-
5)
Post-date pregnancy, n = 17: 41–42 weeks of pregnancy. This group comprised of nine pregnancies terminated by cesarean section and seven pregnancies by spontaneous vaginal delivery lasting from 61 h to 200 h.
All women were healthy and delivered healthy newborns without malformations, chromosomal abnormalities, and postmaturity syndrome.
Additionally, plasma samples from healthy non-pregnant women (n = 15) were included in the study.
Determination of immunoglobulin A concentration
Concentrations of IgA in the amniotic fluid and plasma samples were determined by conventional ELISA. In short, Maxisorp flat-bottomed 96-well microplates (NUNC, Roskilde, Denmark) were coated for 2 h at 37 °C, and overnight at 4 °C with 100 μl of 0.05 M carbonate/bicarbonate buffer (pH 9.6) containing 3 μg/ml of polyclonal rabbit IgA isotype-specific antibodies (DAKO, Glostrup, Denmark). After blocking with 1 % bovine serum albumin (BSA) (SERVA, Heidelberg, Germany), 100 μl of twofold serial dilutions of women’s plasma (range 1:10000–1: 80000), amniotic fluid (range 1:100–1:800), or IgA standard (range 0.0078–0.5 μg/ml) (Jackson Immunoresearch) in phosphate-buffered saline with 0.05 % Tween 20 (PBS-T) containing 1 % BSA, were added to each well and incubated for 2 h at 37 °C. After the washing step, 100 μl of horseradish peroxidase-conjugated rabbit antibodies diluted 1:4000 in PBS-T-1 % BSA were added to each well, and plates were incubated for 2 h at 37 °C. After washing, 100 μl of substrate solution containing ortho-phenylenodiamine (Calbiochem, Denmark) in 0.1 M citrate buffer, pH 4.9 with H2O2 was added, and plates were incubated for 20 min at room temperature in the dark. The reaction was stopped with 1 M H2SO4, and optical density was read at λ = 490 nm with a Dynatech MR 5000 photometric reader (DYNATECH, Dynex Technologies, Sullyfield Circle Chantilly, VA, USA).
Lectin-IgA-ELISA for differentiating sialyl- and fucosyl-glycovariants
Glycotope expressions on IgA were determined by lectin-IgA-ELISA, in accordance with the procedure described earlier, slightly modified, [14, 33] using specific biotinylated lectins [34] (Vector Laboratories Inc., Burlingame, USA): Maackia amurensis lectin (MAA) [28] and Sambucus nigra lectin (SNA) [29] with binding preferences to sialic acid linked by anomeric glycosidic α2,3 and α2,6 linkages and Lens culinaris lectin (LCA) [30], Tetragonolobus purpureus lectin (LTA) [31], and Ulex europaeus lectin (UEA) [32] showing binding preferences to fucose linked by anomeric glycosidic linkages α1,6, α1,3, and α1,2, respectively. However, the binding specificity of lectins is not absolute and usually covers a range of ligands with different relative affinities. Binding will therefore vary depending on the abundance and clustering patterns.
The experimental details of lectin-IgA-ELISA are as follows: rabbit specific anti-human IgA polyclonal antibodies (DAKO, Glostrup, Denmark), defucosylated and desialylated by oxidation with sodium periodate and further desialylated with Vibrio cholera neuraminidase, were diluted 1:1000 in 10 mM TRIS-buffered saline (TBS), pH 8.5, coupled to a polystyrene microtitre ELISA plate, and used to extract and specifically bind IgA in the sample. For testing purposes, 100 μl of amniotic fluid or blood plasma samples, prediluted in 10 mM TBS pH7.5 containing 0.05 % Tween 20 to a final IgA concentration of 0.5 mg/l, were taken. The presence of the respective sialyl-glycotopes and fucosyl-glycotopes on IgA was detected by the reaction with the specific biotinylated lectins MAA (1:500) or SNA (1:20 000) and LCA (1:500), LTA (1:500), or UEA (1:500), respectively. The IgA-lectin complex was measured with phosphatase-labeled ExtrAvidin (1:20 000) (Sigma, St. Louis, MO, USA), and then detected by the reaction with disodium 4-nitrophenyl phosphate (Merck, Darmstadt, Germany). The absorbance (AU) was measured in a Stat Fax 2100 Microplate Reader (Awareness Technology INC, USA) at 405 nm with the reference filter at 630 nm. Obtained absorbance values are proportional to the relative amounts/expressions of fucosyl- and sialyl-glycotopes of IgA.
All samples were analyzed in duplicate. The positive control for MAA, SNA, LCA, LTA, and UEA was native haptoglobin and asialo-haptoglobin preparations derived from ovarian cancer fluid [35]. The negative control was a human albumin preparation included in the test instead of the amniotic fluid and plasma samples. The background absorbance was low (0.05 ± 0.02 AU) when TBS was included in the tests instead of (1) lectin and (2) ExtrAvidin-AP.
Statistical analysis
The statistical analysis was performed with STATISTICA 10 (StatSoft, Inc., Tulsa, USA). The Kruskal–Wallis test and the Mann–Whitney U test were used for statistical significance. The results were shown as the mean ± SD. The correlations were estimated according to Spearman. A two-tailed p-value of less than 0.05 was considered significant.
Results
IgA concentration
The mean values of IgA concentration in the amniotic fluid (Table 2) and plasma of pregnant women (Table 3) showed no significant differences between the 2nd trimester, the 3rd trimester, perinatal period, delivery, and post-date pregnancy groups. The calculated mean and median values of IgA in all plasmas of pregnant women (1.9 ± 1.2 g/l and 1.8 g/l, respectively), corresponded to the normal range of IgA concentration in non-pregnant women (2.1 ± 1.3 g/l and 1.9 g/l, respectively), and were nearly 1000-times higher than in the amniotic fluids (7.7 ± 4.4 mg/l and 6.5 mg/l, respectively).
Expression of MAA- and SNA-reactive glycotopes
The amniotic fluid IgA of all samples reacted with SNA and MAA indicating that the IgA glycans were potentially terminated with sialic acid linked by the α2,6 or α2,3 glycosidic bonds, respectively (Table 2). The expression of MAA-reactive glycotope on IgA showed weak positive correlation (r = 0.35) with the age of normal pregnancy, but no correlation was found for SNA-reactive glycotope (r = 0.2).
The relative reactivity of amniotic IgA with SNA (specific to α2,6-sialyl-glycoform) and MAA (specific to α2,3-sialyl-glycoform) was significantly lower (p < 0.001 and p < 0.00004, respectively) in the 2nd trimester group (0.66 ± 0.3 AU and 0.48 ± 0.3 AU, respectively) than in the 3rd trimester (1.18 ± 0.5 AU and 1.50 ± 0.5 AU, respectively). In the perinatal period (1.15 ± 0.5 AU and 1.68 ± 0.4 AU, respectively) and delivery (1.06 ± 0.6 AU and 1.4 ± 0.6 AU, respectively) groups, the sialylation were nearly at the same levels as in the 3rd trimester, however, α2,6-sialylation level became significantly higher in the post-date pregnancy group (1.42 ± 0.4 AU; p < 0.03) (Fig. 1).
Reactivity of amniotic fluid IgA with sialic acid-specific lectins in relation to pregnancy age. (a) with Maackia amurensis lectin; (b) with Sambucus nigra lectin. For experimental details, see Table 1. Box and whisker plots: the bottom and top of the box are the 25th and 75th percentile (the lower and upper quartiles, respectively), and the small box near the middle of the box is the median (the 50th percentile). The ends of the whiskers represent the minimum and maximum of all the data
The relative reactivity of plasma IgA of pregnant women with SNA (~0.22 AU) had not changed during the stages of pregnancy (Table 3) and was similar to that of non-pregnant women group (0.23 ± 0.04), however being significantly lower (p < 0.00001) when compared to that of amniotic IgA reactivity. In contrast to amniotic IgA, none of plasma IgA showed the reactivity with MAA (Table 2).
Expression of LCA-, LTA-, and UEA-reactive glycotopes
The amniotic IgA reactivity with LTA (specific to α1,3-linked fucose), UEA (specific to α1,2-linked fucose) and LCA (specific to α1,6-linked fucose) showed no correlation with the age of normal pregnancy (r = 0.16; r = 0.17 and r = 0.02, respectively). In contrast, the expressions of all types of fucosylated glycotopes showed strong or very strong positive correlations (r = 0.68 for UEA and LTA; r = 0.61 for UEA and LCA; r = 0.89 for LCA and LTA, respectively).
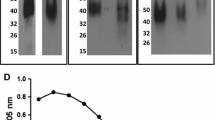
The amniotic fluid IgA from the 2nd trimester showed relatively high reactivity with LCA (for α1,6-fucose) and reacted slightly with LTA (for α1,3-linked fucose) and UEA (for α1,2-fucose) (Table 2). The reactivity of amniotic IgA with LCA remained nearly at the same level during the 2nd trimester (1.04 ± 0.3 AU), 3rd trimester (1.11 ± 0.4 AU), the perinatal period (1.01 ± 0.4 AU), and delivery (0.98 ± 0.4 AU). In contrast, the reactivity with LCA increased in the post-date pregnancy (1.24 ± 0.3 AU; p < 0.01). The significant increase of reactivity of amniotic IgA with LTA and UEA appeared in the 3rd trimester of pregnancy and remained nearly at the same level from the 3rd trimester (0.54 ± 0.4 AU for LTA and 1.05 ± 0.7 AU for UEA) throughout the perinatal period (0.42 ± 0.4 AU for LTA and 1.0 ± 0.8 AU for UEA) to the delivery (0.41 ± 0.4 AU for LTA and 0.75 ± 0.8 AU for UEA), though significantly increased in the post-date pregnancy (0.6 ± 0.3 AU; p < 0.009 for LTA and 1.07 ± 0.6 AU; p < 0.03 for UEA) (Fig. 2).
Reactivity of amniotic fluid IgA with fucose-specific lectins in relation to pregnancy age. (a) with Lens culinaris lectin; (b) with Tetragonolobus purpureus lectin; (c) with Ulex europaeus lectin. For experimental details, see Table 1. Box and whisker plots: the bottom and top of the box are the 25th and 75th percentile (the lower and upper quartiles, respectively), and the small box near the middle of the box is the median (the 50th percentile). The ends of the whiskers represent the minimum and maximum of all the data
The relative amount of LCA-reactive glycotope of plasma IgA (Table 3) was at almost unchanged level throughout pregnancy of 14–42 weeks including the delivery group, and was three times lower when compared to amniotic IgA reactivity with LCA (p < 0.00001). Plasma IgA lacked reactivity with α1-3- as well as α1-2-linked fucose specific lectins (LTA and UEA, respectively).
Discussion
Our results indicate that despite the almost unaltered concentration of IgA in amniotic fluid and pregnant women plasma, the degree of the relative sialylation and fucosylation of the amniotic IgA was connected with progression of the normal pregnancy.
Amniotic fluid might be considered a precursor of human milk feedings as an exogenous source of immunological factors that protect the infant directly and shape the responses of the infant’s own immune system. Thus, the amniotic fluid being produced by, or at least transferred across, epithelial surfaces and bathes many of the mucosal surfaces of the fetus, might be considered part of the mucosal immune system [17]. Amniotic IgA might function as an “antiseptic coating” at the mucosal surface by preventing a bacterial adherence and an invasion of microorganisms [24].
In the amniotic fluid there is more than one source of IgA, namely maternal plasma, decidua and fetus. Maternal IgA is actively transported into the amniotic fluid and can be produced locally in the decidua, since Cederqvist et al. [36] reported that up to one-half of the IgA in amniotic fluid from 11 to 40 weeks of gestation was of the IgA2, characteristic for produced by mucosa [17]. The extent to which nonspecific diffusion and receptor-mediated transport of maternal IgA and the fetal mucosa contributes to amniotic IgA vary with gestational age [17, 19].
In the 2nd trimester of normal pregnancy the amniotic IgA showed a different pattern of sialylation and fucosylation than the plasma of pregnant women (Tables 2 and 3). The amniotic IgA was more highly LCA- and SNA- reactive than the maternal IgA, suggesting that amniotic IgA was heavily α2,6-sialylated and α1,6-fucosylated. Additionally, the amniotic IgA was decorated by glycotopes reactive with MAA, LTA, and UEA. The appearance of the α2,3-sialylated glycotope on glycoproteins recognized by MAA was reported by Hampel et al. [37] to be bound with fetal development and classified as a fetal type of protein glycosylation. On the other hand, the plasma IgA of both pregnant and non-pregnant women did not show any reactivity with MAA (Table 3) and that observation shows a discrepancy with findings of Maenuma et al. [38]. They have reported a reactivity of mutated α2,3-sialic acid-specific MAA with IgA O-glycans isolated from normal and IgA nephritis patients. It should be pointed out that in our lectin-based analysis, the lack of reactivity of the plasma IgA samples with MAA might result from a different spatial accessibility of α2,3-sialylated glycotopes hidden in the structure of the hinge region of native IgA [26, 27, reviewed 39] of plasma sample compared to the isolated molecule of IgA. Moreover, the limited amount of native plasma and amniotic fluid IgA, namely 50 ng, used in our Lectin-ELISA probably also had impact on the observed lack of reactivity.
During the 3rd trimester, the last immunological phase of pregnancy, the fetus has completed its development; all the organs are functional and ready to deal with the external world [40]. Placental function is dynamic and influenced by maternal health, and has an important regulatory role in maternal and fetal well-being [41]. The glycosylation pattern of amniotic IgA seems to be a net result of maternal, fetal, and placental synthesis. Fetal urine is a major source, however, Goldblum and Hilton [17] suggest that the IgA is produced locally and excreted from the mucosal surfaces (other than urinary tract) of the fetus, namely respiratory, saliva and nasal secretions of fetus also contribute to the content of the amniotic fluid.
The presence of highly MAA-, LTA-, and UEA-reactive glycotopes at the turn of the 2nd and the 3rd trimesters is probable connected with fetal development and maturation. The fetus mucosal system production of IgA is increased and outweighs the mother’s participation and has a direct impact on the glycosylation pattern of amniotic IgA during the 3rd trimester. The same characteristic quantitative switch was previously observed for amniotic IgG [14] and other amniotic glycoconjugates [42] and glycoproteins, namely α1-acid glycoprotein [12] and fibronectin [43].
The expression of MAA-, SNA-, LCA-, LTA-, and UEA-reactive glycotopes on amniotic IgA has only slightly changed between the 3rd trimester and the perinatal period. Although the data are for limited amount of samples because of rarely occurring opportunities for the collection of amniotic fluid in this period, they are very valuable to understand the protective role of amniotic fluid. Moreover, the expression of LTA- and UEA-reactive glycotopes (α1,3- and α1,2-fucosylated glycans), which are known to create Lewis family determinants [2], valuable indicators of inflammation [44, 45] as well as molecules involved in innate immunity [25] may vary among individuals as a result of a non-secretor status [46] of mother and may reflect the sensitivity of individuals to external stimuli and efficiency of the immune system.
Delivery is characterized by an influx of immune cells into the myometrium in order to promote recrudescence of an inflammatory process. However, the proinflammatory environment which promotes the contraction of the uterus, expulsion of the baby, and rejection of the placenta [40, 47] seems to have no impact on sialylation and fucosylation of amniotic IgA during delivery. We have previously shown that during the delivery amniotic IgG [14] and fibronectin [43], glycoproteins which do not directly take part in response to inflammation (characteristic for acute phase proteins), also showed almost unaltered expression of fucosyl- and sialyl-glycotopes.
Fetal and neonatal mortality rates increase sharply after 40 weeks of pregnancy [48]. The pregnancy can be prolonged by inadequate hormone levels and maternal obesity and can increase the risk of Caesarean delivery and maternal complications. Around 41 weeks placental function may decline and become insufficient, reducing the supply of oxygen and nutrients to the fetus [41, 48]. We have observed that in the post-date pregnancy, there was the increase of the fetal or/and placental origin of highly fucosylated and sialylated amniotic IgA glycoforms compared to those at delivery. The changes observed by us for amniotic IgA in the post-date pregnancy group, apart from MAA-reactive glycotopes, overlap/correspond to those reported for the amniotic IgG [14]. These findings can lead to the hypothesis that for amniotic immunoglobulins a common gestational age-dependent mechanism of glycosylation regulation can exist, probably connected with site-dependent synthesis and/or modulation of glycosylation.
In conclusion, pregnancy is a time of life where the development, maturation of fetus, and modulation of the immune system of mother, as well as differential responses of diverse biological events may occur based on glycotope-lectin receptor interactions. During the pregnancy stages these interactions might be important for controlling the pro-inflammatory and anti-inflammatory phases characterized by the unique inflammatory environment reported by Mor et al. [40]. In this aspect, the 1st and 3rd trimesters defined as proinflammatory phases (Th1) are responsible for the implantation and placentation as well as contraction of the uterus, expulsion of the baby and rejection of the placenta, respectively. On the contrary, the 2nd trimester represents an anti-inflammatory phase, also known as the Th2 environment, in which the mother, placenta and fetus are symbiotic [40, 49]. It should be noted that the observed changes of the expressions of lectin-reactive sialylated and fucosylated glycotopes at the turn of the 2nd and the 3rd trimesters also overlap with immunological phases of pregnancy (Fig. 3).
In our opinion, the pregnancy-associated unique expressions of sialylated and fucosylated glycoforms of amniotic IgA illustrate a general importance of carbohydrate-lectin and/or carbohydrate-carbohydrate interactions in the control and modulation of pro- and anti-inflammatory events to ensuring the fetus well-being. Glycovariants of amniotic IgA associated with pregnancy progression overlap and/or are influenced by a gestational-depended pro- and anti-inflammatory condition. They seem to be molecular indicators reflecting the pregnancy age and can also be used as a window into the physiological events that lead up to both normal and post-date pregnancy. However, a future aim for these studies is the structural analysis of the IgA oligosaccharides that should confirm or verify relative levels of sialic acid and fucose of the lectin based proposals, and helps to understand their role and impact on the course of pregnancy.
Abbreviations
- IgA:
-
Immunoglobulin A
- LCA:
-
Lens culinaris lectin
- LTA:
-
Tetragonolobus purpureus lectin
- MAA:
-
Maackia amurensis lectin
- SNA:
-
Sambucus nigra lectin
- UEA:
-
Ulex europaeus lectin
- Fuc:
-
Fucose
- SA:
-
Sialic acid
References
Haltiwanger, R.S., Lowe, J.B.: Role of glycosylation in development. Annu. Rev. Biochem. 73, 491–573 (2004)
Becker, D.J., Lowe, J.B.: Fucose: biosynthesis and biological function in mammals. Glycobiology 13, 41–53 (2003)
Schauer, R.: Sialic acids as regulators of molecular and cellular interactions. Curr. Opin. Struct. Biol. 19, 507–514 (2009)
Orczyk-Pawiłowicz, M., Kątnik-Prastowska, I.: Terminal monosaccharide expression on amniotic glycoproteins as biomarkers of fetus maturity. Biochem. Soc. Trans. 39, 344–348 (2011)
Jeschke, U., Toth, B., Scholz, C., Friese, K., Makrigiannakis, A.: Glycoprotein and carbohydrate binding protein expression in the placenta in early pregnancy loss. J. Reprod. Immunol. 85, 99–105 (2010)
Uszyński, W., Uszyński, M., Zekanowska, E., Kuczyński, J., Szymański, M.: Selectins in human amniotic fluid and cord blood plasma. A preliminary report. Thromb. Res. 127, 60–61 (2011)
Carson, D.D., Farrar, J.D., Laidlaw, J., Wright, D.A.: Selective activation of the N-glycosylation apparatus in uteri by estrogen. J. Biol. Chem. 265, 2947–2955 (1990)
Kobata, A.: The N-linked sugar chain of human immunoglobulin G: their unique pattern, and their functional roles. Biochim. Biophys. Acta 1780, 472–478 (2008)
Brinkman-Van der Linden, E.C.M., Havenaar, E.C., Van Ommen, E.C.R., Van Kamp, G.J., Gooren, L.J.G., Van Dijk, W.: Oral estrogen treatment induces a decrease in expression of sialyl Lewis x on alpha1-acid glycoprotein in females and male-to-female transsexuals. Glycobiology 6, 407–412 (1996)
Jeschke, U., Xiaoyu, W., Volker, B., Friese, K., Stahn, R.: Glycodelin and amniotic fluid transferrin as inhibitors of E-selectin-mediated cell adhesion. Histochem. Cell Biol. 119, 345–354 (2003)
Jeschke, U., Stahn, R., Goletz, C., Wang, X.Y., Briese, V., Friese, K.: HCG in trophoblast tumour cells of the cell line Jeg3 and hCG isolated from amniotic fluid and serum of pregnant women carry oligosaccharides of the sialyl Lewis x and sialyl Lewis a type. Anticancer. Res. 23, 1087–1092 (2003)
Orczyk-Pawiłowicz, M., Hirnle, L., Kątnik-Prastowska, I.: The expression of fucose isoforms of amniotic and plasma alpha-1-acid glycoprotein derived from 2nd and 3rd trimester normal pregnancies. Clin. Biochem. 42, 1517–1523 (2009)
Hirnle, L., Kątnik-Prastowska, I.: Amniotic fibronectin fragmentation and expression of its domains, sialyl and fucosyl glycotopes associated with pregnancy complicated by intrauterine infection. Clin. Chem. Lab. Med. 45, 208–214 (2007)
Orczyk-Pawiłowicz, M., Augustyniak, D., Hirnle, L., Kątnik-Prastowska, I.: Degree of sialylation and fucosylation of plasma and amniotic immunoglobulin G changes progressively during normal pregnancy. Prenat. Diagn. 35, 432–439 (2012)
Briese, V., Kunkel, S., Plath, C., Wutzke, K.D., Plesse, R.: Sialic acid, steroids and proteohormones in maternal, cord and retroplacental blood. Z. Geburtshilfe Neonatol. 203, 63–68 (1999)
Bowen, J.M., Chamley, L., Keelan, J.A., Mitchell, M.D.: Cytokines of the placenta and extra-placental membranes: roles and regulation during human pregnancy and parturition. Placenta 23, 257–273 (2002)
Goldblum, R.M., Hilton, S.: Amniotic fluid and the fetal mucosal immune system. In: Ogra, P.L., Mestecky, J., Lamm, M.E., Strober, W., Bienenstock, J., McGhee, J.R. (eds.) Mucosal immunology, 2nd edn, pp. 1555–1564. Academic, London (1999)
Quan, C.P., Forestier, F., Bouvet, J.-P.: Immunoglobulins of the human amniotic fluid. Am. J. Reprod. Immunol. 42, 219–225 (1999)
Jauniaux, E., Jurkovic, D., Gulbis, B., Liesnard, C., Lees, C., Campbell, S.: Materno-fetal immunoglobulin transfer and passive immunity during the first trimester of human pregnancy. Hum. Reprod. 10, 3297–3300 (1995)
Quan, C.P., Berneman, A., Pirts, R., Avrameas, S., Bouvet, J.P.: Natural polyreactive secretory immunoglobulin A autoantibodies as a possible barrier to infection in humans. Infect. Immun. 65, 3997–4004 (1997)
Quan, C.P., Watanabe, S., Forestier, F., Bouvet, J.P.: Human amniotic IgA inhibits natural IgG autoantibodies of maternal or unrelated origin. Eur. J. Immunol. 28, 4001–4009 (1998)
Arnold, J.N., Dwek, R.A., Rudd, P.M., Sim, R.B.: Mannan binding lectin and its interaction with immunoglobulins in health and in disease. Immunol. Lett. 106, 103–110 (2006)
Kerr, M.A.: The structure and function of human IgA. Biochem. J. 271, 285–296 (1990)
Monteiro, R.C.: Role of IgA and IgA Fc receptors in inflammation. J. Clin. Immunol. 30, 1–9 (2010)
Royle, L., Roos, A., Harvey, D.J., Wormald, M.R., van Gijlswijk-Janssen, D., Redwan, el-R.M., Wilson, I.A., Daha, M.R., Dwek, R.A., Rudd, P.M.: Secretory IgA N- and O-glycans provide a link between the innate and adaptive immune systems. J. Biol. Chem. 278, 20140–20153 (2003)
Arnold, J.N., Royle, L., Dwek, R.A., Rudd, P.M., Sim, R.B.: Human immunoglobulin glycosylation and the lectin pathway of complement activation. John S. Axford (ed), Glycobiology and Medicine, pp 27–43. Springer, Printed in the Netherlands (2005)
Mattu, T.S., Pleass, R.J., Willis, A.C., Kilian, M., Wormald, M.R., Lellouch, A.C., Rudd, P.M., Woof, J.M., Dwek, R.A.: The glycosylation and structure of human serum IgA1, Fab, and Fc regions and the role of N-glycosylation on Fc alpha receptor interactions. J. Biol. Chem. 273, 2260–2272 (1998)
Knibbs, R., Goldstein, I.J., Ratcliff, R.M., Shibuya, N.: Characterization of the carbohydrate binding specificity of the leukoagglutinating lectin from Maackia amurensis. Comparison with other sialic acid-specific lectins. J. Biol. Chem. 266, 83–88 (1991)
Shibuya, N., Goldstein, I.J., Broekaert, W.F., Nsimba-Lubaki, M., Peeters, B., Peumans, W.J.: The elderberry (Sambucus nigra L.) bark lectin recognizes the Neu5Ac(α2,6)Gal/GalNAc sequence. J. Biol. Chem. 262, 1596–1601 (1987)
Kornfeld, K., Reitman, M.L., Kornfeld, R.: The carbohydrate-binding specificity of pea and lentil lectins. Fucose is an important determinant. J. Biol. Chem. 256, 6633–6640 (1981)
Yan, L., Wilkins, P.P., Alvarez-Manilla, G., Do, S.I., Smith, D.F., Cummings, R.D.: Immobilized Lotus tetragonolobus agglutinin binds oligosaccharides containing the Le x determinant. Glycoconj. J. 14, 45–55 (1997)
Audette, G.F., Vandonselaar, M., Delbaere, L.T.J.: The 2.2 Å resolution structure of the O(H) blood-group-specific Lectin I from Ulex europaeus. J. Mol. Biol. 304, 423–433 (2000)
Orczyk-Pawiłowicz, M., Hirnle, L., Kątnik-Prastowska, I.: High expression of α1,2- and α1,6-linked fucoses on amniotic AGP as a biomarker of fetal postmaturity risk. J. Immunoassay Immunochem. 32, 103–113 (2011)
Wu, A.M., Lisowska, E., Duk, M., Yang, Z.: Lectins as tools in glycoconjugate research. Glycoconj. J. 26, 899–913 (2009)
Kątnik, I., Jadach, J., Krotkiewski, H., Gerber, J.: Investigating the glycosylation of normal and ovarian cancer haptoglobins using digoxigenin-labeled lectins. Glycosyl. Dis. 1, 97–104 (1994)
Cederquist, L.L., Ewool, L.C., Bonsnes, R.W., Litwin, S.D.: Detectability and pattern of immunoglobulins in normal amniotic-fluid throughout gestation. Am. J. Obstet. Gynecol. 130, 220–224 (1978)
Hampel, D.J., Köttgen, B., Dudenhausen, J.W., Köttgen, E.: Fetal fibronectin as a marker for an imminent preterm delivery. A new technique using the glycoprotein lectin immunosorbent assay. J. Immunol. Methods 224, 31–42 (1999)
Maenuma, K., Yim, M., Komatsu, K., Hoshino, M., Takahashi, Y., Bovin, N., Irimura, T.: Use of a library of mutated Maackia amurensis hemagglutinin for profiling the cell lineage and differentiation. Proteomics 8, 3274–3283 (2008)
Novak, J., Julian, B.A., Mestecky, J., Renfrow, M.B.: Glycosylation of IgA1 and pathogenesis of IgA nephropathy. Semin. Immunopathol. 34, 365–382 (2012)
Mor, G., Cardenas, I., Abrahams, V., Guller, S.: Inflammation and pregnancy: the role of the immune system at the implantation site. Ann. N. Y. Acad. Sci. 1221, 80–87 (2011)
Denison, F.C., Roberts, K.A., Barr, S.M., Norman, J.E.: Obesity, pregnancy, inflammation, and vascular function. Reproduction 140, 373–385 (2010)
Orczyk-Pawiłowicz, M., Florjański, J., Zalewski, J., Kątnik-Prastowska, I.: Relative amounts of sialic acid and fucose of amniotic fluid glycoconjugates in relation to pregnancy age. Glycoconj. J. 22, 433–442 (2005)
Hirnle, L.: Analysis of fibronectin molecular forms in amniotic fluid and plasma of pregnant women during normal and complicated by intrauterine infection pregnancies. Habilitation Thesis, Wrocław Medical University, Wrocław, Poland (2006)
Van Dijk, W., Poland, D.C.: Anti-inflammatory properties of specific glycoforms of human alpha1-acid glycoprotein. Adv. Exp. Med. Biol. 535, 251–256 (2003)
Kreisman, L.S., Cobb, B.A.: Infection, inflammation and host carbohydrates: a glyco-evasion hypothesis. Glycobiology 22, 1019–1030 (2012)
Chaturvedi, P., Warren, C.D., Altaye, M., Morrow, A.L., Ruiz-Palacios, G., Pickering, L.K., Newburg, D.S.: Fucosylated human milk oligosaccharides vary between individuals and over the course of lactation. Glycobiology 11, 365–372 (2001)
Romero, R., Espinoza, J., Goncalves, L.F., Kusanovic, J.P., Friel, L.A., Nien, J.K.: Inflammation in preterm and term labour and delivery. Semin. Fetal Neonatal. Med. 11, 317–326 (2006)
Hilder, L., Costeloe, K., Thilaganathan, B.: Prolonged pregnancy: evaluating gestation-specific risks of fetal and infant mortality. Br. J. Obstet. Gynaecol. 105, 169–173 (1998)
Mor, G., Cardenas, I.: The immune system in pregnancy: a unique complexity. Am. J. Reprod. Immunol. 63, 425–433 (2010)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Orczyk-Pawiłowicz, M., Augustyniak, D., Hirnle, L. et al. Lectin-based analysis of fucose and sialic acid expressions on human amniotic IgA during normal pregnancy. Glycoconj J 30, 599–608 (2013). https://doi.org/10.1007/s10719-012-9460-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10719-012-9460-8