Abstract
In addition to classic germline APC gene variants, APC mosaicism and deep intronic germline APC variants have also been reported to be causes of adenomatous polyposis. In this study, we investigated 80 unexplained colorectal polyposis patients without germline pathogenic variants in known polyposis predisposing genes to detect mosaic and deep intronic APC variants. All patients developed more than 50 colorectal polyps, with adenomas being predominantly observed. To detect APC mosaicism, we performed next-generation sequencing (NGS) in leukocyte DNA. Furthermore, using Sanger sequencing, the cohort was screened for the following previously reported deep intronic pathogenic germline APC variants: c.1408 + 731C > T, p.(Gly471Serfs*55), c.1408 + 735A > T, p.(Gly471Serfs*55), c.1408 + 729A > G, p.(Gly471Serfs*55) and c.532-941G > A, p.(Phe178Argfs*22). We did not detect mosaic or intronic APC variants in the screened unexplained colorectal polyposis patients. The results of this study indicate that the deep intronic APC variants investigated in this study are not a cause of colorectal polyposis in this Dutch population. In addition, NGS did not detect any further mosaic variants in our cohort.
Similar content being viewed by others
Introduction
Pathogenic germline variants in APC (MIM# 611,731) cause familial adenomatous polyposis syndrome (FAP; MIM# 175,100), a rare autosomal dominant-inherited syndrome characterized by the development of multiple colorectal adenomas and a very high risk of colorectal cancer [1,2,3,4]. In classic FAP, patients develop hundreds to thousands of colorectal adenomatous polyps, while in attenuated FAP (AFAP), patients develop fewer adenomas (< 100) at a later age than those with classical FAP [5,6,7,8]. A subset of patients with multiple colorectal adenomas and no APC germline variants have been found to carry biallelic variants in the base excision repair gene MUTYH (MIM# 604,933), causing MUTYH-associated polyposis (MAP; MIM# 608,456) [9]. In addition, a number of other genes associated with adenomatous polyposis, such as POLE, POLD1, NTHL1, MSH3 and MLH3, have recently been reported [10,11,12,13]. The detection rate of APC variants in FAP patients depends on phenotype and methods. In classic FAP, APC germline variants can be detected in up to 85% of patients [14, 15]; however, the detection rates of APC germline variants in patients with fewer colorectal adenomatous polyps (AFAP patients) are lower, ranging from 10 to 30% of patients [14, 16], suggesting that a proportion of pathogenic variants remain undetected by routine methods [17,18,19]. Mosaic APC variants and deep intronic variants localized in regions not covered by PCR-based diagnostics were previously identified as additional causal factors. Using RNA-based assays and next-generation sequencing (NGS), it has been shown that a proportion of variant-negative FAP patients harbor molecular changes in deep intronic regions of APC [19, 20]. These studies identified deep intronic APC variants that result in pseudoexon formation [19, 20]. Through the use of sensitive techniques, somatic APC mosaicism has been demonstrated in a minority of adenomatous polyposis patients [21,22,23,24,25,26]. In addition, using deep sequence analysis of APC in DNA isolated from multiple adenomas, mosaic variants were identified in 9 of 18 patients with 21 to 100 adenomas; in some of these cases, NGS also detected the variants in leukocyte DNA at low frequency [27]. In this study, we investigate the role of deep intronic germline APC variants and mosaic APC variants in leukocyte DNA as possible genetic causes of colorectal polyposis in a Dutch cohort of unexplained patients with more than 50 polyps.
Materials and methods
Patients
A total of 80 index patients with more than 50 colorectal polyps (Table 1) were selected from a previously described cohort [28,29,30,31]. The cohort included patients previously screened for germline mosaic APC variants by denaturing gradient gel electrophoresis (DGGE) [17], the protein truncation test (PTT) [17] and high resolution melting analysis (HRMA) [21]. All cases tested negative for pathogenic germline variants in APC, MUTYH, POLE, and POLD1 and for NTHL1 hotspot variants. Clinicopathological data included date of birth, gender, age at diagnosis of colorectal polyps/adenomas, cumulative number of polyps, location and histology of polyps/adenomas, information on CRC and presence of polyps/CRC in first-degree family members. Since the term serrated adenomas is currently preferred over hyperplastic polyps, we lumped together polyps described as such under the term sessile serrated lesions with or without dysplasia. Three controls were included in this study. Leukocyte DNA from this cohort was available for the study. The study was approved by the medical ethics committee of Leiden University Medical Center, protocol P01-019.
APC intronic variant screening
Leukocyte DNA of the patients was screened for the intronic APC variants in Table 2 using Sanger sequencing. Primers were designed using Primer3 software http://primer3.ut.ee/ and were obtained from Eurofins Genomics (Ebersberg, Germany). The following primers with universal M13 tails were used: c.1408 + 731C > T, c.1408 + 735A > T and c.1408 + 729A > G; forward: 5′-TGTAAAACGACGGCCAGTATCATGCTGAACCATCTCAT-3′ and reverse: 5′ CAGGAAACAGCTATGACCAAATGACGAATGAAACGATG-3′. For c.532-941G > A; forward: 5′ TGTAAAACGACGGCCAGTAGAGGGTTTGGGAAGTGGAG-3′ and reverse: 5′ CAGGAAACAGCTATGACCTCTGTGTGCCCTTAGAAAACTG-3′. Sanger sequencing of the PCR amplified fragments was performed by Macrogen (Amsterdam, Netherlands). The sequencing results were analyzed using Mutation Surveyor software (Sofgenetics, State College PA, USA).
Next-generation sequencing and data analysis
Deep APC sequencing was performed using a previously described custom APC panel [27]. The complete sequencing panel consisted of 115 amplicons (11,216 bp), covering 99.3% of the coding regions of APC. Libraries were prepared with Ion Ampliseq™ 2.0 Kit (Thermo Fisher Scientific, Bleiswijk, The Netherlands) according to the manufacturer’s instructions and were sequenced on the Ion Torrent Proton Platform (Thermo Fisher Scientific, Bleiswijk, The Netherlands). Sequence data were analyzed as described previously [27]. Variants were annotated to the GenBank reference sequence NM_000038.4. The Integrative Genomics Viewer (IGV) (https://www.broadinstitute.org/igv/) was used to visualize the read alignment and the presence of variants against the reference genome.
Results and discussion
In this study, we attempt to identify the genetic causes of colorectal polyposis in unexplained patients with colorectal polyposis. Deep NGS of APC was performed to identify possible undetected pathogenic mosaic variants. Furthermore, APC intronic germline variants described previously [19, 20] were studied to evaluate their role. A high-risk cohort was selected for this study, consisting of 80 index patients with ≥ 50 colorectal polyps (Table 1), of whom many had a relatively early onset, which increases the probability of finding undiscovered mosaic or intronic variants. The mean age at diagnosis of colorectal polyps was 49 years (range 12–80). The majority of patients (n = 51, 63.8% with a mean age of 51 years at diagnosis) had a cumulative polyp count between 50 and 100, while 29 patients (36.2% with a mean age of 46 years at diagnosis) showed more than 100 polyps. Forty-five percent of the patients displayed only adenomatous polyps, while 47.5% of the patients displayed a mixed phenotype with adenomas and sessile serrated lesions with or without dysplasia. CRC was found in 27 patients (33.8%, with a mean age of 56 years, range 37–80). The clinical characteristics of the patients are summarized in Table 1.
First, we screened the leukocyte DNA of 80 patients for the following deep intronic heterozygous germline variants in APC: c.1408 + 731C > T, p.(Gly471Serfs*55), c.1408 + 735A > T, p.(Gly471Serfs*55), c.1408 + 729A > G, p.(Gly471Serfs*55) and c.532-941G > A, p.(Phe178Argfs*22). We did not detect any of these variants in our cohort. The study by Spier et al. [19] was the first to describe APC-related pseudoexons in FAP patients from Germany. These pseudoexons were caused by three heterozygous germline variants with a combined frequency of 6.4% (8/125); APC c.532-941G > A was identified in five patients, APC c.1408 + 731C > T was identified in two patients, and APC c.1408 + 735A > T was identified in one patient [19]. In a second study by Nieminen et al. [20], two additional intronic variants were identified in a cohort of 54 patients from Finland: APC c.1408 + 729A > G and APC c.646-1806 T > G and the variant identified previously by Spier et al., APC c.1408 + 731C > T. The overall reported frequency of these variants from the study by Nieminen et al. was 5.5% (3/54). The reported frequency of these intronic variants from both studies is approximately 6%. Nevertheless, we could not detect these variants in our cohort, possibly because either the frequency of intronic variants is lower in the Dutch population and the sample size of our cohort is not large enough or because these variants are local founder variants.
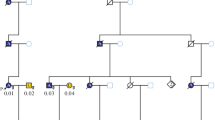
Subsequently, we performed deep APC sequencing of leukocyte DNA from 80 colorectal polyposis patients. Our positive controls were two previously described cases with mosaic APC variants [27]; APC c.4110_4111delAA was reported to be present in leukocyte DNA with 4% variant allele frequency (VAF), and APC c.2493dupA was reported with a VAF of 3% in leukocyte DNA. The APC mosaic variant c.4057G > T served as a negative control, as the variant was detected previously [27] in normal colonic mucosa and was absent in leukocyte DNA. Both positive controls, APC c.4110_4111delAA (Fig. 1) and APC c.2493dupA, were clearly present, while APC c.4057G > T was absent in the negative control. No additional APC mosaic variants were detected in our cohort. A limitation of this study is that we used only leukocyte DNA for mosaicism screening due to the scarcity of available DNA from patient adenomas. Mosaicism might remain undetectable or be overlooked if the molecular analysis is limited to blood, even when sensitive techniques are applied, due to very low or even absent presentation of the mutated allele [23, 27]. Peripheral blood cells arise from the mesoderm, and when the variant occurs after mesoderm and endoderm specification (early postzygotic mutation), the mosaicism is likely restricted to the colon and is difficult to detect the variant in leukocyte DNA [23, 27, 32, 33]. In a previous study, it was recommended to test at least two or more adenomas to detect mosaic variants [27].
A recent systematic review of current APC mosaicism studies recommends testing adenomas from the polyposis patients without APC germline variant to allow the detection of low allele frequency mosaicism as well as mosaicism confined to colon [33]. Consequently, in our study, APC mosaic variants confined to the colon could have been missed because we could not screen the DNA from the adenomas of the patients.
In conclusion, we did not detect any of the four previously reported APC intronic variants in our cohort. We also did not detect mosaic APC variants in our cohort using deep sequencing analysis in blood. This finding suggests that the benefit of using targeted amplicon-based NGS to further scrutinize the APC gene in unexplained cases of polyposis is limited. Analyzing DNA from adenomas in addition to leukocyte DNA is recommended to detect a possible underlying mosaicism. Also, other approaches, such as whole genome sequencing or transcriptome sequencing, could be employed to detect undiscovered intronic or promoter variants or other regulatory variants.
Abbreviations
- FAP:
-
Familial adenomatous polyposis syndrome
- AFAP:
-
Attenuated FAP
- NGS:
-
Next-generation sequencing
- DGGE:
-
Denaturing gradient gel electrophoresis
- PTT:
-
Protein truncation test
- HRMA:
-
High resolution melting analysis
- IGV:
-
Integrative genomics viewer
- VAF:
-
Variant allele frequency
References
Bodmer WF, Bailey CJ, Bodmer J et al (1987) Localization of the gene for familial adenomatous polyposis on chromosome 5. Nature 328(6131):614–616. https://doi.org/10.1038/328614a0
Bisgaard ML, Fenger K, Bulow S, Niebuhr E, Mohr J (1994) Familial adenomatous polyposis (FAP): frequency, penetrance, and mutation rate. Hum Mutat 3(2):121–125. https://doi.org/10.1002/humu.1380030206
Fearnhead NS, Britton MP, Bodmer WF (2001) The ABC of APC. Hum Mol Genet 10(7):721–733. https://doi.org/10.1093/hmg/10.7.721
Yurgelun MB, Kulke MH, Fuchs CS et al (2017) Cancer susceptibility gene mutations in individuals with colorectal cancer. J Clin Oncol: Off J Am Soc Clin Oncol 35(10):1086–1095. https://doi.org/10.1200/jco.2016.71.0012
Knudsen AL, Bisgaard ML, Bulow S (2003) Attenuated familial adenomatous polyposis (AFAP) A review of the literature. Familial Cancer 2(1):43–55. https://doi.org/10.1023/a:1023286520725
Jasperson KW, Tuohy TM, Neklason DW, Burt RW (2010) Hereditary and familial colon cancer. Gastroenterology 138(6):2044–2058. https://doi.org/10.1053/j.gastro.2010.01.054
Nielsen M, Hes FJ, Nagengast FM et al (2007) Germline mutations in APC and MUTYH are responsible for the majority of families with attenuated familial adenomatous polyposis. Clin Genet 71(5):427–433. https://doi.org/10.1111/j.1399-0004.2007.00766.x
Nieuwenhuis MH, Vasen HF (2007) Correlations between mutation site in APC and phenotype of familial adenomatous polyposis (FAP): a review of the literature. Crit Rev Oncol Hematol 61(2):153–161. https://doi.org/10.1016/j.critrevonc.2006.07.004
Al-Tassan N, Chmiel NH, Maynard J et al (2002) Inherited variants of MYH associated with somatic G:C–>T: a mutations in colorectal tumors. Nat Genet 30(2):227–232. https://doi.org/10.1038/ng828
Palles C, Cazier JB, Howarth KM et al (2013) Germline mutations affecting the proofreading domains of POLE and POLD1 predispose to colorectal adenomas and carcinomas. Nat Genet 45(2):136–144. https://doi.org/10.1038/ng.2503
Weren RD, Ligtenberg MJ, Kets CM et al (2015) A germline homozygous mutation in the base-excision repair gene NTHL1 causes adenomatous polyposis and colorectal cancer. Nat Genet 47(6):668–671. https://doi.org/10.1038/ng.3287
Adam R, Spier I, Zhao B et al (2016) Exome sequencing identifies biallelic MSH3 germline mutations as a recessive subtype of colorectal adenomatous polyposis. Am J Hum Genet 99(2):337–351. https://doi.org/10.1016/j.ajhg.2016.06.015
Olkinuora A, Nieminen TT, Mårtensson E et al (2019) Biallelic germline nonsense variant of MLH3 underlies polyposis predisposition. Genet Med: Off J Am College Med Genet 21(8):1868–1873. https://doi.org/10.1038/s41436-018-0405-x
Friedl W, Aretz S (2005) Familial adenomatous polyposis: experience from a study of 1164 unrelated german polyposis patients. Hereditary Cancer Clin Pract 3(3):95–114. https://doi.org/10.1186/1897-4287-3-3-95
Aretz S, Stienen D, Uhlhaas S et al (2005) Large submicroscopic genomic APC deletions are a common cause of typical familial adenomatous polyposis. J Med Genet 42(2):185–192. https://doi.org/10.1136/jmg.2004.022822
Terlouw D, Suerink M, Singh SS et al (2020) Declining detection rates for APC and biallelic MUTYH variants in polyposis patients, implications for DNA testing policy. Eur J Human Genet: EJHG 28(2):222–230. https://doi.org/10.1038/s41431-019-0509-z
Hes FJ, Nielsen M, Bik EC et al (2008) Somatic APC mosaicism: an underestimated cause of polyposis coli. Gut 57(1):71–76. https://doi.org/10.1136/gut.2006.117796
Rohlin A, Wernersson J, Engwall Y, Wiklund L, Bjork J, Nordling M (2009) Parallel sequencing used in detection of mosaic mutations: comparison with four diagnostic DNA screening techniques. Hum Mutat 30(6):1012–1020. https://doi.org/10.1002/humu.20980
Spier I, Horpaopan S, Vogt S et al (2012) Deep intronic APC mutations explain a substantial proportion of patients with familial or early-onset adenomatous polyposis. Hum Mutat 33(7):1045–1050. https://doi.org/10.1002/humu.22082
Nieminen TT, Pavicic W, Porkka N et al (2016) Pseudoexons provide a mechanism for allele-specific expression of APC in familial adenomatous polyposis. Oncotarget 7(43):70685–70698. https://doi.org/10.18632/oncotarget.12206
Out AA, van Minderhout IJ, van der Stoep N et al (2015) High-resolution melting (HRM) re-analysis of a polyposis patients cohort reveals previously undetected heterozygous and mosaic APC gene mutations. Fam Cancer 14(2):247–257. https://doi.org/10.1007/s10689-015-9780-5
Yamaguchi K, Komura M, Yamaguchi R et al (2015) Detection of APC mosaicism by next-generation sequencing in an FAP patient. J Hum Genet 60(5):227–231. https://doi.org/10.1038/jhg.2015.14
Spier I, Drichel D, Kerick M et al (2016) Low-level APC mutational mosaicism is the underlying cause in a substantial fraction of unexplained colorectal adenomatous polyposis cases. J Med Genet 53(3):172–179. https://doi.org/10.1136/jmedgenet-2015-103468
Ciavarella M, Miccoli S, Prossomariti A et al (2018) Somatic APC mosaicism and oligogenic inheritance in genetically unsolved colorectal adenomatous polyposis patients. Eur J Human Genet: EJHG 26(3):387–395. https://doi.org/10.1038/s41431-017-0086-y
Kim B, Won D, Jang M et al (2019) Next-generation sequencing with comprehensive bioinformatics analysis facilitates somatic mosaic APC gene mutation detection in patients with familial adenomatous polyposis. BMC Med Genom 12(1):103. https://doi.org/10.1186/s12920-019-0553-0
Urbanova M, Hirschfeldova K, Obeidova L et al (2019) Two Czech patients with familial adenomatous polyposis presenting mosaicism in APC gene. Neoplasma 66(2):294–300. https://doi.org/10.4149/neo_2018_180731N559
Jansen AM, Crobach S, Geurts-Giele WR et al (2017) Distinct patterns of somatic mosaicism in the APC gene in neoplasms from patients with unexplained adenomatous polyposis. Gastroenterology 152(3):546–9.e3. https://doi.org/10.1053/j.gastro.2016.10.040
Hes FJ, Ruano D, Nieuwenhuis M et al (2014) Colorectal cancer risk variants on 11q23 and 15q13 are associated with unexplained adenomatous polyposis. J Med Genet 51(1):55–60. https://doi.org/10.1136/jmedgenet-2013-102000
Elsayed FA, Kets CM, Ruano D et al (2015) Germline variants in POLE are associated with early onset mismatch repair deficient colorectal cancer. Eur J Human Genet: EJHG 23(8):1080–1084. https://doi.org/10.1038/ejhg.2014.242
Elsayed FA, Tops CMJ, Nielsen M, et al. (2019) Low frequency of POLD1 and POLE exonuclease domain variants in patients with multiple colorectal polyps. Molecular genetics & genomic medicine: e603 https://doi.org/https://doi.org/10.1002/mgg3.603
Grolleman JE, de Voer RM, Elsayed FA et al (2019) Mutational Signature Analysis Reveals NTHL1 Deficiency to Cause a Multi-tumor Phenotype. Cancer Cell 35(2):256–66.e5. https://doi.org/10.1016/j.ccell.2018.12.011
Tuohy TM, Burt RW (2008) Somatic mosaicism: a cause for unexplained cases of FAP? Gut 57(1):10–12. https://doi.org/10.1136/gut.2007.133108
Jansen AML, Goel A (2020) Mosaicism in patients with colorectal cancer or polyposis syndromes: a systematic review. Clin Gastroenterol Hepatol: Off Clin Pract J Am Gastroenterol Assoc 18(9):1949–1960. https://doi.org/10.1016/j.cgh.2020.02.049
Acknowledgements
The authors would like to thank Demi van Egmond for technical support and Diantha Terlouw for support with clinical data.
Funding
Grant support: This study was supported in part by the Dutch Digestive Foundation (MLDS FP13-13 to TVW).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elsayed, F.A., Tops, C.M.J., Nielsen, M. et al. Use of sanger and next-generation sequencing to screen for mosaic and intronic APC variants in unexplained colorectal polyposis patients. Familial Cancer 21, 79–83 (2022). https://doi.org/10.1007/s10689-021-00236-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-021-00236-2