Abstract
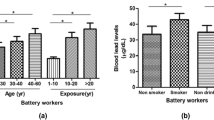
Occupational exposure to lead compounds can cause headache, nausea, encephalopathy, anemia, chronic muscle pain, and saturnism. Exposure to lead in women can affect fertility, and cause abortion or low IQ in the offspring. The aim of this study was to investigate occupational exposure to lead and its relation with blood lead levels in female electrical parts solderers. This cross-sectional (descriptive and analytical) study was carried out on 40 female solderers, working in two electrical parts manufacturing factories in Neyshabur city in 2017–2018. Occupational exposure to lead was determined by the OSHA 121 method, and the NIOSH 8003 method was used to determine the concentration of lead in blood. Lead in blood and air samples were determined by using a flame atomic absorption analyzer. Blood was measured using a Cell Dyn Hematology device. Data were analyzed using STATA 15. The mean age of the solderers was 35.42 ± 6.80 years, and their average work experience was 7.85 ± 5.60 years. Mean occupational exposure to lead was 0.09 ± 0.01 mg/m3, and the mean levels of lead in the blood of solderers were 10.59 ± 3.25 μg/dL. The mean of red blood cells (RBC) was 4.88 mil/uL, white blood cells (WBC) = 8.53 Tho/uL, hemoglobin = 14.02 g/dL, and hematocrit = 42.38%. There was a significant correlation between the concentrations of lead in air and the level of lead in workers’ blood (p = 0.012, r = 0.31). The level of lead in the workers’ respiratory region (β = 0.36, p = 0.033), body mass index (β = 0.25, p = 0.028), and the season of the year (β = 0.21, p = 0.019) were the strongest factors affecting blood lead levels. There was a significant relation between lead in workers’ air and their blood, although all blood indices were in normal range. Using lead-free alloys and local ventilation systems, and reducing exposure times are recommended to decrease exposure to lead among solderers.
Similar content being viewed by others
References
Agency for Toxic Substances and Disease Registry (ATSDR), Lead Toxicity. (2018). Agency for Toxic Substances and Disease Registry; Atlanta, GA. 2010. Retrieved fall, Available at: www. Atsdr.cdc.gov/toxicological profile for lead
Ahamed, M., Mehrotra, P. K., Kumar, P., & Siddiqui, M. K. J. (2009). Placental lead-induced oxidative stress and preterm delivery. Environmental Toxicology and Pharmacology, 27(1), 70–74.
American Conference of Governmental Industrial Hygienists(ACGIH). (2017). TLVs and BEIs. Retrieved fall, 2018, Available: https://www.acgih.org/forms/store/ProductFormPublic/2017-tlvs-and-beis
Arasaratnam, M., et al. (2004). Occupational lead exposure of soldering workers in an electronic factory. Journal of Occupational Safety and Health, 95, 49.
Baker, E. L., et al. (1977). Lead poisoning in children of lead workers: home contamination with industrial dust. New England Journal of Medicine, 296(5), 260–261.
Barkhordari, A., et al. (2014a). The toxic effects of silver nanoparticles on blood mononuclear cells. The international journal of occupational and environmental medicine, 5(3), 394-164-398.
Barkhordari, A., et al. (2014b). The glycoprofile patterns of endothelial cells in usual interstitial pneumonia. The international journal of occupational and environmental medicine, 5(4), 387-201-387.
Boseila, S. A., et al. (2004). Blood lead levels in Egyptian children: influence of social and environmental factors. American journal of public health, 94(1), 47–49.
Chen, P. C., et al. (2006). Parental exposure to lead and small for gestational age births. American journal of industrial medicine, 49(6), 417–422.
Dehghan-Nasiri, M. et al. (2012). "Biological and environmental monitoring of lead and exposure in the automobile industry." Iran Occupational Health 8(4)
Farooq, Y., et al. (2008). Lead intoxication: the extent of problem and its management. Pakistan Journal of Physiology, 4(2), 36–41.
Flora, G., et al. (2012). Toxicity of lead: a review with recent updates. Interdisciplinary toxicology, 5(2), 47–58.
Gardella, C. (2001). Lead exposure in pregnancy: a review of the literature and argument for routine prenatal screening. Obstetrical & gynecological survey, 56(4), 231–238.
Ghotbi, M. R., et al. (2013). Changes in urinary catecholamines in response to noise exposure in workers at Sarcheshmeh copper complex, Kerman, Iran. Environmental monitoring and assessment, 185(11), 8809–8814.
Golmohammadi, T. et al. (2007). "The effect of maternal and fetal lead concentration on birth weight: polluted versus non-polluted areas of Iran. Tehran University of Medical Sciences journal, 65(8), 74–78.
Golpayegani, A., & Khanjani, N. (2012). Occupational and environmental exposure to lead in Iran: a systematic review. Journal of Health and Development, 1(1), 74–89.
Hashemi Nejad, N., et al. (2013). Survey of relationship between mental health and job stress among midwives who were working in hospitals of Kerman, Iran, 2011. The Iranian journal of obstetrics, gynecology and infertility, 16(64), 1–9.
Ibeh, N., et al. (2016). The influence of occupational lead exposure on haematological indices among petrol station attendants and automobile mechanics in Nnewi, South-East Nigeria. J Environ Occup Sci, 5(1), 1.
Levin, S. M., & Goldberg, M. (2000). Clinical evaluation and management of lead-exposed construction workers. American journal of industrial medicine, 37(1), 23–43.
Lin, C.-M., et al. (2010). The role of essential metals in the placental transfer of lead from mother to child. Reproductive Toxicology, 29(4), 443–446.
International Agency for Research on Cancer (IARC). (2006). Group authors from the World Health Organization. IARC monographs on the evaluation of carcinogenic risks to humans. Lyon: 2006, Retrieved fall, 2018, fromavailable: https://www.who.int/en/news-room/fact-sheets/detail/lead-poisoning-and-health
Matczak, W. (2002). Assessment of exposure to toxic metals released during soldering and grazing processes. Medycyna pracy, 53(6), 473–480.
Ministry of Health and Medical Education (MHME), (2017). Occupational exposure limit (OEL). Tehran University of Medical Sciences
Rahimi-Moghadam, S., et al. (2017). Decline in lung function among cement production workers: a meta-analysis. Reviews on environmental health, 32(4), 333–341.
Mohammadyan, M., et al. (2019). Occupational exposure to styrene and its relation with urine mandelic acid, in plastic injection workers. Environmental Monitoring and Assessment, 191, 62.
Naicker, N., et al. (2010). Lead exposure is associated with a delay in the onset of puberty in South African adolescent females: findings from the Birth to Twenty cohort. Science of the total environment, 408(21), 4949–4954.
National Institute for Occupational Safety and Health (NIOSH). (2003). "Lead in blood and urine." Retrieved fall, 2018, from https://www.cdc.gov/niosh/docs/2003-154/pdfs/8003.pdf
Neyshabur of Ministry of Cooperatives Labour and Social Welfare (NMCLSW). (2018). Retrieved Winter 2018, https://khorasanrazavi.mcls.gov.ir/fa/vahedhayetabe/shahrha/nishaboor
Neyshabur University of Medical Sciences( NUMS), occupational health units. (2018). Retrieved Winter 2018, Available: https://nums.ac.ir
Occupational Safety and Health Administration (OSHA). (2006a). "Metal & metalloid particulates in workplace atmospheres(atomic absorption)." Retrieved Winter 2018, from https://www.osha.gov/dts/sltc/methods/toc_l.html
Occupational Safety and Health Administration (OSHA). (2006b). Blood lead laboratories program description and background. 2006. Retrieved winter 2018, from Available from: URL:http://www.oshagov/SLTC/bloodlead/ program. html
Phoon, W., et al. (1990). Biological monitoring of workers exposed to inorganic lead in Singapore. Singapore Med J, 31(2), 127–130.
Pinon-Lataillade, G., et al. (1995). Reproductive toxicity of chronic lead exposure in male and female mice. Human & experimental toxicology, 14(11), 872–878.
Rahman, S., et al. (2006). Non-occupational lead exposure and hypertension in Pakistani adults. Journal of Zhejiang University Science B, 7(9), 732–737.
Rice, C., et al. (1978). Lead contamination in the homes of employees of secondary lead smelters. Environmental research, 15(3), 375–380.
Richardson, D. B., Cardis, E., Daniels, R. D., et al. (2015). Risk of cancer from occupational exposure to ionising radiation: retrospective cohort study of workers in France, the United Kingdom, and the United States (INWORKS). bmj journal, 351, 5359.
Semczuk, M., & Semczuk-Sikora, A. (2001). New data on toxic metal intoxication (Cd, Pb, and Hg in particular) and Mg status during pregnancy. Medical Science Monitor, 7(2), 332–340.
Shah, F., et al. (2010). Environmental exposure of lead and iron deficit anemia in children age ranged 1–5 years: a cross sectional study. Science of the total environment, 408(22), 5325–5330.
Shahtaheri, S. M., & Afshari, D. (2007). Occupational Toxicology (pp. 237–243). Tehran: Baraye Farda Publication.
Solon, O., et al. (2008). Associations between cognitive function, blood lead concentration, and nutrition among children in the central Philippines. The Journal of Pediatrics, 152(2), 237–243 e231.
Srivastava, S., et al. (2001). Blood lead and zinc in pregnant women and their offspring in intrauterine growth retardation cases. Journal of analytical toxicology, 25(6), 461–465.
Tang, N., & Zhu, Z. Q. (2003). Adverse reproductive effects in female workers of lead battery plants. International journal of occupational medicine and environmental health, 16(4), 359–361.
Torres-Sánchez, L. E., et al. (1999). Intrauterine lead exposure and preterm birth. Environmental research, 81(4), 297–301.
Vigeh, M., et al. (2006). Lead and other trace metals in preeclampsia: a case–control study in Tehran, Iran. Environmental research, 100(2), 268–275.
Vigeh, M., et al. (2010). Early pregnancy blood lead levels and the risk of premature rupture of the membranes. Reproductive Toxicology, 30(3), 477–480.
Wang, N., et al. (2015). Blood lead level and its association with body mass index and obesity in China-results from SPECT-China study. Scientific reports, 5, 18299.
Winchester, H. A. (2007). Clinical management of poisoning and drug overdose (4th ed.). Philadelphia: Saunders Elsevier.
Wilhelm, M., et al. (2010). Reassessment of critical lead effects by the German human biomonitoring commission results in suspension of the human biomonitoring values (HBM I and HBM II) for lead in blood of children and adults. International journal of hygiene and environmental health, 213(4), 265–269.
World Health Organization. (1995). Biological indices of lead exposure and body burden. In IPCS, Inorganic lead, Environmental Health Criteria 118 (Vol. 165, pp. 114–118). Geneva: WHO.
Acknowledgements
The authors thank Dr. Abedi, Ph.D in Analytical Chemistry and the Simorgh Pharmaceutical Industry which helped in preparing and analyzing the samples.
Funding
This study was conducted with the financial support of both Mazandaran University of Medical Sciences and Neyshabur University of Medical Sciences, and by grant number 3036-96.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mohammadyan, M., Moosazadeh, M., Borji, A. et al. Investigation of occupational exposure to lead and its relation with blood lead levels in electrical solderers. Environ Monit Assess 191, 126 (2019). https://doi.org/10.1007/s10661-019-7258-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10661-019-7258-x