Abstract
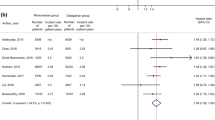
Emerging observational studies using propensity score (PS) methods assessed real-world comparative effectiveness of non-vitamin K antagonist oral anticoagulants (NOACs) versus warfarin in patients with non-valvular atrial fibrillation (AF). We aimed to compare treatment effect estimates of NOACs between PS studies and randomized controlled trials (RCTs). Electronic databases and conference proceedings were searched systematically. Primary outcomes included stroke or systemic embolism (SE) and major bleeding. A random-effects meta-analysis was performed to synthesize the data by pooling the PS- and RCT-derived hazard ratios (HRs) separately. The ratio of HRs (RHR) from the ratio of PS-derived HRs relative to RCT-derived HRs was used to determine whether there was a difference between estimates from PS studies and RCTs. There were 10 PS studies and 5 RCTs included for analysis. No significant difference of treatment effect estimates between the PS studies and RCTs was observed: RHR 1.11, 95 % CI 0.98–1.23 for stroke or SE; RHR 1.07, 95 % CI 0.87–1.34 for major bleeding. A significant association between NOACs and risk of stroke or SE was observed: HR 0.88, 95 % CI 0.83–0.94 for the PS studies; HR 0.79, 95 % CI 0.72–0.87 for the RCTs. However, no relationship between NOACs and risk of major bleeding was found: HR 0.91, 95 % CI 0.79–1.05 for the PS studies; HR 0.85, 95 % CI 0.73–1.00 for the RCTs. In this study, treatment effect estimates of NOACs versus warfarin in patients with non-valvular AF from PS studies are found to be in agreement with those from RCTs.





Similar content being viewed by others
References
Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129(8):837–47.
Rockson SG, Albers GW. Comparing the guidelines: anticoagulation therapy to optimize stroke prevention in patients with atrial fibrillation. J Am Coll Cardiol. 2004;43(6):929–35.
Cairns JA, Connolly S, McMurtry S, Stephenson M, Talajic M. Canadian Cardiovascular Society atrial fibrillation guidelines 2010: prevention of stroke and systemic thromboembolism in atrial fibrillation and flutter. Can J Cardiol. 2011;27(1):74–90.
Camm AJ, Kirchhof P, Lip GY, Schotten U, Savelieva I, Ernst S, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Eur Heart J. 2010;31(19):2369–429.
Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G. Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e44S–88S.
Verheugt FW, Granger CB. Oral anticoagulants for stroke prevention in atrial fibrillation: current status, special situations, and unmet needs. Lancet. 2015;386(9990):303–10.
Dentali F, Riva N, Crowther M, Turpie AG, Lip GY, Ageno W. Efficacy and safety of the novel oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of the literature. Circulation. 2012;126(20):2381–91.
Adam SS, McDuffie JR, Ortel TL, Williams JW Jr. Comparative effectiveness of warfarin and new oral anticoagulants for the management of atrial fibrillation and venous thromboembolism: a systematic review. Ann Intern Med. 2012;157(11):796–807.
Miller CS, Grandi SM, Shimony A, Filion KB, Eisenberg MJ. Meta-analysis of efficacy and safety of new oral anticoagulants (dabigatran, rivaroxaban, apixaban) versus warfarin in patients with atrial fibrillation. Am J Cardiol. 2012;110(3):453–60.
Cameron C, Coyle D, Richter T, Kelly S, Gauthier K, Steiner S, et al. Systematic review and network meta-analysis comparing antithrombotic agents for the prevention of stroke and major bleeding in patients with atrial fibrillation. BMJ Open. 2014;4(6):e004301.
Fox BD, Kahn SR, Langleben D, Eisenberg MJ, Shimony A. Efficacy and safety of novel oral anticoagulants for treatment of acute venous thromboembolism: direct and adjusted indirect meta-analysis of randomised controlled trials. BMJ (Clinical research ed). 2012;345:e7498.
Jia B, Lynn HS, Rong F, Zhang W. Meta-analysis of efficacy and safety of the new anticoagulants versus warfarin in patients with atrial fibrillation. J Cardiovasc Pharmacol. 2014;64(4):368–74.
Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62.
Gomez-Outes A, Terleira-Fernandez AI, Calvo-Rojas G, Suarez-Gea ML, Vargas-Castrillon E. Dabigatran, rivaroxaban, or apixaban versus warfarin in patients with nonvalvular atrial fibrillation: a systematic review and meta-analysis of subgroups. Thrombosis. 2013;2013:640723.
Liu GJ, Wang YF, Chen PY, Chang W, Tu ML, Chang LY, et al. The efficacy and safety of novel oral anticoagulants for the preventive treatment in atrial fibrillation patients: a systematic review and meta-analysis. Drug Deliv. 2014;21(6):436–52.
Sibbald B, Roland M. Understanding controlled trials. Why are randomised controlled trials important? BMJ (Clinical research ed). 1998;316(7126):201.
Rothwell PM. External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet. 2005;365(9453):82–93.
Byar DP. Why data bases should not replace randomized clinical trials. Biometrics. 1980;36(2):337–42.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424.
Heinze G, Juni P. An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J. 2011;32(14):1704–8.
Guo S, Fraser MW. Propensity score analysis: statistical methods and applications: statistical methods and applications. Thousand Oaks: Sage Publications; 2014.
Rubin DB. The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med. 2007;26(1):20–36.
Heinze G, Jüni P. An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J. 2011;32(14):1704–8.
Dahabreh IJ, Sheldrick RC, Paulus JK, Chung M, Varvarigou V, Jafri H, et al. Do observational studies using propensity score methods agree with randomized trials? A systematic comparison of studies on acute coronary syndromes. Eur Heart J. 2012;33(15):1893–901.
Lonjon G, Boutron I, Trinquart L, Ahmad N, Aim F, Nizard R, et al. Comparison of treatment effect estimates from prospective nonrandomized studies with propensity score analysis and randomized controlled trials of surgical procedures. Ann Surg. 2014;259(1):18–25.
Zhang Z, Ni H, Xu X. Do the observational studies using propensity score analysis agree with randomized controlled trials in the area of sepsis? J Crit Care. 2014;29(5):886.e9–15. doi:10.1016/j.jcrc.2014.05.023.
Zhang Z, Ni H, Xu X. Observational studies using propensity score analysis underestimated the effect sizes in critical care medicine. J Clin Epidemiol. 2014;67(8):932–9.
Kuss O, Legler T, Borgermann J. Treatments effects from randomized trials and propensity score analyses were similar in similar populations in an example from cardiac surgery. J Clin Epidemiol. 2011;64(10):1076–84.
Kitsios GD, Dahabreh IJ, Callahan S, Paulus JK, Campagna AC, Dargin JM. Can we trust observational studies using propensity scores in the critical care literature? A systematic comparison with randomized clinical trials. Crit Care Med. 2015;43(9):1870–9.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions 5.1.0. [updated March 2011] http://handbook.cochrane.org. Accessed October, 2015.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed). 2009;339:b2535.
Providencia R, Albenque JP, Combes S, Bouzeman A, Casteigt B, Combes N, et al. Safety and efficacy of dabigatran versus warfarin in patients undergoing catheter ablation of atrial fibrillation: a systematic review and meta-analysis. Heart (British Cardiac Society). 2014;100(4):324–35.
Lip GY, Merino J, Ezekowitz M, Ellenbogen K, Zamoryakhin D, Lanz H, et al. A prospective evaluation of edoxaban compared to warfarin in subjects undergoing cardioversion of atrial fibrillation: the EdoxabaN vs. warfarin in subjectS UndeRgoing cardiovErsion of Atrial Fibrillation (ENSURE-AF) study. Am Heart J. 2015;169(5):597–604.e5. doi:10.1016/j.ahj.2015.02.009.
Nairooz R, Sardar P, Pino M, Aronow WS, Sewani A, Mukherjee D, et al. Meta-analysis of risk of stroke and thrombo-embolism with rivaroxaban versus vitamin K antagonists in ablation and cardioversion of atrial fibrillation. Int J Cardiol. 2015;6(187):345–53.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37(5):360–3.
The ROBINS-I tool (Risk Of Bias In Non-randomized Studies—of Interventions). https://sites.google.com/site/riskofbiastool/. Accessed June, 2016.
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ (Clinical research ed). 2003;326(7382):219.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Hori M, Matsumoto M, Tanahashi N, Momomura S, Uchiyama S, Goto S, et al. Rivaroxaban vs. Warfarin in Japanese patients with atrial fibrillation—the J-ROCKET AF study. Circ J. 2012;76(9):2104–11.
Abraham NS, Singh S, Alexander GC, Heien H, Haas LR, Crown W, et al. Comparative risk of gastrointestinal bleeding with dabigatran, rivaroxaban, and warfarin: population based cohort study. BMJ (Clinical research ed). 2015;350:h1857.
Hernandez I, Baik SH, Pinera A, Zhang Y. Risk of bleeding with dabigatran in atrial fibrillation. JAMA Intern Med. 2015;175(1):18–24.
Laliberte F, Cloutier M, Nelson WW, Coleman CI, Pilon D, Olson WH, et al. Real-world comparative effectiveness and safety of rivaroxaban and warfarin in nonvalvular atrial fibrillation patients. Curr Med Res Opin. 2014;30(7):1317–25.
Larsen TB, Rasmussen LH, Skjoth F, Due KM, Callreus T, Rosenzweig M, et al. Efficacy and safety of dabigatran etexilate and warfarin in “real-world” patients with atrial fibrillation: a prospective nationwide cohort study. J Am Coll Cardiol. 2013;61(22):2264–73.
Lauffenburger JC, Farley JF, Gehi AK, Rhoney DH, Brookhart MA, Fang G. Effectiveness and safety of dabigatran and warfarin in real-world US patients with non-valvular atrial fibrillation: a retrospective cohort study. J Am Heart Assoc. 2015;4(4):e001798.
Graham DJ, Reichman ME, Wernecke M, Zhang R, Southworth MR, Levenson M, et al. Cardiovascular, bleeding, and mortality risks in elderly medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2014;131(2):157–64.
Leef G, Qin D, Althouse A, Alam MB, Rattan R, Munir MB, et al. Risk of stroke and death in atrial fibrillation by type of anticoagulation: a propensity-matched analysis. Pacing Clin Electrophysiol. 2015;38(11):1310–6.
Bengtson L, Chen L, MacLehose R, Lutsey P, Alonso A. Comparative effectiveness of dabigatran and rivaroxaban versus warfarin in patients with non-valvular atrial fibrillation. Circulation. 2014;130(Suppl 2):A20218.
Seeger JD, Bartels DB, Huybrechts K, Bykov K, Shash D, Zint K, et al. Safety and effectiveness of dabigatran relative to warfarin in routine care. Circulation. 2014;130(Suppl 2):A16227.
Tsadok MA, Jackevicius CA, Essebag V, Eisenberg MJ, Rahme E, Humphries KH, et al. Comparative effectiveness and safety of dabigatran vs. Warfarin in patients with atrial fibrillation-evidence from real world practice. Circulation. 2013;128(Suppl 22):A13884.
Connolly SJ, Ezekowitz MD, Yusuf S, Reilly PA, Wallentin L. Newly identified events in the RE-LY trial. N Engl J Med. 2010;363(19):1875–6.
Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Sturmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163(12):1149–56.
Chai-Adisaksopha C, Crowther M, Isayama T, Lim W. The impact of bleeding complications in patients receiving target-specific oral anticoagulants: a systematic review and meta-analysis. Blood. 2014;124(15):2450–8.
Robins JM. Correction for non-compliance in equivalence trials. Stat Med. 1998;17(3):269–302 (discussion 387–269).
Swanson SA, Robins JM, Miller M, Hernan MA. Selecting on treatment: a pervasive form of bias in instrumental variable analyses. Am J Epidemiol. 2015;181(3):191–7.
Acknowledgments
GL. receives a Father Sean O’Sullivan Research Award, the Research Institute of St. Joseph’s Healthcare Hamilton, and a doctoral award from the CSC. M.C. sat on advisory boards for Janssen, Leo Pharma, Portola, and AKP America; his institution has received funding for research projects from Leo Pharma; and he received funding for presentations from Leo Pharma, Bayer, Celgene, Shire, and CSL Behring. S.C. received consulting fees, lecture fees, and grant support from Boehringer Ingelheim.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, G., Holbrook, A., Jin, Y. et al. Comparison of treatment effect estimates of non-vitamin K antagonist oral anticoagulants versus warfarin between observational studies using propensity score methods and randomized controlled trials. Eur J Epidemiol 31, 541–561 (2016). https://doi.org/10.1007/s10654-016-0178-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-016-0178-y