Abstract
In this study we aimed to identify cancers where there is a consistent sex disparity, with the goal of identifying unexplained sex disparities that may offer promising opportunities for etiologic research. Age- and sex-specific cancer incidence data from Cancer Incidence in Five Continents, provided by the International Agency for Research on Cancer, were used to calculate incidence rate ratios for 35 cancer sites, comparing men to women, adjusting for attained age, gross domestic product (GDP), and geographical region. Genital cancers and breast cancer were excluded. The consistency of relative risks was examined by GDP and geographical region and, in a subset of longstanding cancer registers, by calendar year. For each cancer site, the sex disparity was broadly classified as plausibly explained by established environmental risk factors, partly explained, or unexplained. Cancer incidence was statistically significantly higher in men than women at 32 of 35 sites, with disparities >2-fold for 15 sites and >4-fold for 5 sites. For nearly all sites, the sex disparity was consistent across GDP groups and geographical regions. However, the incidence rate ratios varied considerably by age at diagnosis. The sex disparity for 13 cancer sites was considered to be entirely unexplained by known risk factors; these sites showed strikingly little variation in the incidence rate ratios over decades. Thus, the basis of many of the largest sex disparities in cancer incidence seems mostly unknown, highlighting the need for intensified research into its origins.



Similar content being viewed by others
References
Adami HO, Hunter D, Trichopoulos D, editors. Textbook of cancer epidemiology. 2nd ed. New York: Oxford University Press; 2008.
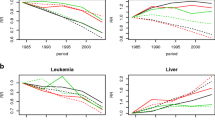
Cook MB, Dawsey SM, Freedman ND, et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1174–82.
Cook MB, McGlynn KA, Devesa SS, Freedman ND, Anderson WF. Sex disparities in cancer mortality and survival. Cancer Epidemiol Biomarkers Prev. 2011;20(8):1629–37.
Fuchs CS, Mayer RJ. Gastric carcinoma. N Engl J Med. 1995;333(1):32–41.
Czene K, Adami HO, Chang ET. Sex- and kindred-specific familial risk of non-Hodgkin’s lymphoma. Cancer Epidemiol Biomarkers Prev. 2007;16(11):2496–9.
Schwartz EE, Upton AC. Factors influencing the incidence of leukemia: special consideration of the role of ionizing radiation. Blood. 1958;13(9):845–64.
Yu MC, Yuan JM. Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol. 2002;12(6):421–9.
Haselkorn T, Stewart SL, Horn-Ross PL. Why are thyroid cancer rates so high in southeast asian women living in the United States? The bay area thyroid cancer study. Cancer Epidemiol Biomarkers Prev. 2003;12(2):144–50.
Gitschier J, Wood WI, Goralka TM, et al. Characterization of the human factor VIII gene. Nature. 1984;312(5992):326–30.
Camp PG, Goring SM. Gender and the diagnosis, management, and surveillance of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2007;4(8):686–91.
Curado MP, Edwards B, Shin HR, et al., editors. Cancer incidence in five continents, vol. IX. Lyon: IARC Scientific Publications; 2007.
World Development Indicators [database on the Internet]. The World Bank. 2009. Available from: http://data.worldbank.org/.
Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45(Suppl 2):S3–9.
MacKay J, Eriksen M. The tobacco atlas. Geneva: World Health Organization; 2002.
IARC monographs on the evaluation of carcinogenic risks to humans: tobacco smoke and involuntary smoking. Lyon: International Agency for Research on Cancer; 2002.
Bagnardi V, Blangiardo M, La Vecchia C, Corrao G. A meta-analysis of alcohol drinking and cancer risk. Br J Cancer. 2001;85(11):1700–5.
IARC monographs on the evaluation of carcinogenic risks to humans: alcohol drinking. Lyon: International Agency for Research on Cancer; 1988.
Driscoll T, Steenland K, Prüss-Üstun A, Imel Nelson D, Leigh J. Occupational carcinogens: assessing the environmental burden of disease at national and local levels. Prüss-Üstün A, Campbell-Lendrum D, Corvalán C, Woodward A, editors. Geneva: World Health Organization; 2004.
Black RJ, Bray F, Ferlay J, Parkin DM. Cancer incidence and mortality in the European Union: cancer registry data and estimates of national incidence for 1990. Eur J Cancer. 1997;33(7):1075–107.
Whitacre CC. Sex differences in autoimmune disease. Nat Immunol. 2001;2(9):777–80.
Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39(Suppl 1):5–41.
Albanes D, Winick M. Are cell number and cell proliferation risk factors for cancer? J Natl Cancer Inst. 1988;80(10):772–4.
Roberts DL, Dive C, Renehan AG. Biological mechanisms linking obesity and cancer risk: new perspectives. Annu Rev Med. 2010;61:301–16.
IARC monographs on the evaluation of carcinogenic risks to humans: combined estrogen-progestogen contraceptives and combined estrogen-progestogen menopausal therapy. Lyon: International Agency for Research on Cancer; 2005.
Liu J, Morgan M, Hutchison K, Calhoun VD. A study of the influence of sex on genome wide methylation. PLoS One. 2010;5(4):e10028.
Bjornsson HT, Sigurdsson MI, Fallin MD, et al. Intra-individual change over time in DNA methylation with familial clustering. JAMA. 2008;299(24):2877–83.
Kaminsky ZA, Tang T, Wang SC, et al. DNA methylation profiles in monozygotic and dizygotic twins. Nat Genet. 2009;41(2):240–5.
Christensen BC, Houseman EA, Marsit CJ, et al. Aging and environmental exposures alter tissue-specific DNA methylation dependent upon CpG island context. PLoS Genet. 2009;5(8):e1000602.
Fraga MF, Ballestar E, Paz MF, et al. Epigenetic differences arise during the lifetime of monozygotic twins. Proc Natl Acad Sci USA. 2005;102(30):10604–9.
Esteller M. Epigenetics in cancer. N Engl J Med. 2008;358(11):1148–59.
Alexander DD, Mink PJ, Adami HO, et al. The non-Hodgkin lymphomas: a review of the epidemiologic literature. Int J Cancer. 2007;120(Suppl 12):1–39.
Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2001;345(11):784–9.
Hjalgrim H, Askling J, Rostgaard K, et al. Characteristics of Hodgkin’s lymphoma after infectious mononucleosis. N Engl J Med. 2003;349(14):1324–32.
Gillison ML, Koch WM, Capone RB, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000;92(9):709–20.
Henle G, Henle W. Epstein-Barr virus-specific IgA serum antibodies as an outstanding feature of nasopharyngeal carcinoma. Int J Cancer. 1976;17(1):1–7.
Beasley RP, Hwang LY, Lin CC, Chien CS. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet. 1981;2(8256):1129–33.
Bruix J, Barrera JM, Calvet X, et al. Prevalence of antibodies to hepatitis C virus in Spanish patients with hepatocellular carcinoma and hepatic cirrhosis. Lancet. 1989;2(8670):1004–6.
Lleo A, Battezzati PM, Selmi C, Gershwin ME, Podda M. Is autoimmunity a matter of sex? Autoimmun Rev. 2008;7(8):626–30.
Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8(9):737–44.
Inman RD. Immunologic sex differences and the female predominance in systemic lupus erythematosus. Arthr Rheum. 1978;21(7):849–52.
Nelson RL, Davis FG, Sutter E, Sobin LH, Kikendall JW, Bowen P. Body iron stores and risk of colonic neoplasia. J Natl Cancer Inst. 1994;86(6):455–60.
Stevens RG, Jones DY, Micozzi MS, Taylor PR. Body iron stores and the risk of cancer. N Engl J Med. 1988;319(16):1047–52.
Hercberg S, Estaquio C, Czernichow S, et al. Iron status and risk of cancers in the SU.VI.MAX cohort. J Nutr. 2005;135(11):2664–8.
Edgren G, Nyren O, Melbye M. Cancer as a ferrotoxic disease: are we getting hard stainless evidence? J Natl Cancer Inst. 2008;100(14):976–7.
Edgren G, Reilly M, Hjalgrim H, et al. Donation frequency, iron loss, and risk of cancer among blood donors. J Natl Cancer Inst. 2008;100(8):572–9.
Beard JL, Dawson H, Pinero DJ. Iron metabolism: a comprehensive review. Nutr Rev. 1996;54(10):295–317.
Stevens RG. Iron and the risk of cancer. Med Oncol Tumor Pharmacother. 1990;7(2–3):177–81.
Zacharski LR, Chow BK, Howes PS, et al. Reduction of iron stores and cardiovascular outcomes in patients with peripheral arterial disease: a randomized controlled trial. JAMA. 2007;297(6):603–10.
Zacharski LR, Chow BK, Howes PS, et al. Decreased cancer risk after iron reduction in patients with peripheral arterial disease: results from a randomized trial. J Natl Cancer Inst. 2008;100(14):996–1002.
Frisch M, Glimelius B, van den Brule AJ, et al. Sexually transmitted infection as a cause of anal cancer. N Engl J Med. 1997;337(19):1350–8.
Edgren G, Sparen P. Risk of anogenital cancer after diagnosis of cervical intraepithelial neoplasia: a prospective population-based study. Lancet Oncol. 2007;8(4):311–6.
Fraumeni JF Jr. Cancers of the pancreas and biliary tract: epidemiological considerations. Cancer Res. 1975;35(11 Pt. 2):3437–46.
Tazuma S. Gallstone disease: epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol. 2006;20(6):1075–83.
Acknowledgments
We thank Prof. Georg Klein and Dr. Min-Han Tan for their critical review of an earlier draft of this manuscript. All four authors contributed to the study design and drafting of the manuscript. Dr Edgren had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The final approval of the manuscript was performed by Drs Edgren and Chang. Dr Edgren has received funding through a post-doctoral stipend from Svenska Sällskapet för Medicinsk Forskning (SSMF). No other funding was obtained for this study.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Edgren, G., Liang, L., Adami, HO. et al. Enigmatic sex disparities in cancer incidence. Eur J Epidemiol 27, 187–196 (2012). https://doi.org/10.1007/s10654-011-9647-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-011-9647-5