Summary
Purpose Galunisertib, a TGF-β inhibitor, has demonstrated antitumor effects in preclinical and radiographic responses in some patients with malignant glioma. This Phase 1b/2a trial investigated the clinical benefit of combining galunisertib with temozolomide-based radiochemotherapy (TMZ/RTX) in patients with newly diagnosed malignant glioma (NCT01220271). Methods This is an open-label, 2-arm Phase 1b/2a study (N = 56) of galunisertib (intermittent dosing: 14 days on/14 days off per cycle of 28 days) in combination with TMZ/RTX (n = 40), versus a control arm (TMZ/RTX, n = 16). The primary objective of Phase 1b was to determine the safe and tolerable Phase 2 dose of galunisertib. The primary objective of Phase 2a was to confirm the tolerability and pharmacodynamic profile of galunisertib with TMZ/RTX, and the secondary objectives included determining the efficacy and pharmacokinetic (PK) profile of galunisertib with TMZ/RTX in patients with glioblastoma. This study also characterized the changes in the major T-cell subsets during TMZ/RTX plus galunisertib treatment. Results In the Phase 2a study, efficacy results for patients treated with galunisertib plus TMZ/RTX or TMZ/RTX were: median overall survival (18.2 vs 17.9 months), median progression-free survival (7.6 vs 11.5 months), and disease control rate (80% [32/40] vs 56% [9/16] patients) respectively. PK profile of galunisertib plus TMZ/RTX regimen was consistent with previously published PK data of galunisertib. The overall safety profile across treatment arms was comparable. Conclusion No differences in efficacy, safety or pharmacokinetic variables were observed between the two treatment arms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GB) is the most common and aggressive brain cancer representing approximately 15% of all primary brain tumors, and about 55% of all gliomas [1]. The standard of care for patients with GB consists of maximal surgical resection followed by radiotherapy (RTX) with concomitant and maintenance temozolomide (TMZ). This therapy results in progression-free survival (PFS) at 6 months of 53.9% and median overall survival of 14.6 months [2]. Most of the therapy-responsive patients will die within a period of 2 years and the 2- and 5-year overall survival rates are 27% and 9.8%, respectively [3].
GB is characterized by persistent angiogenesis at the tumor site, and decreased peripheral immune responsiveness in patients [4]. GB microenvironment is enriched in immunosuppressive molecules such as transforming growth factor (TGF)-β that plays a specific role in cancer cell growth [5], in addition to affecting immune cell response, and endothelial cell and fibroblast differentiation [6, 7].
TGF-β is a multifunctional cytokine that is involved in a variety of cell functions including cell proliferation, migration, survival, and death that influence tumor growth in advanced forms of cancer [6, 7]. Upon binding to their ligands (TGF-β1, 2, and 3), the TGF-β kinase receptors are phosphorylated triggering phosphorylation of SMAD2 and SMAD3, and formation of SMAD complexes [8, 9].
Galunisertib is an oral small molecule inhibitor of TGF-β kinase receptor type I (TGF-β RI/ALK5) [10] and selectively inhibits the serine/threonine activity of the receptor, thereby preventing the phosphorylation of downstream proteins, SMAD2 and SMAD3 [10]. The antitumor activity of galunisertib has been demonstrated in three different in vivo tumor models; two breast cancer models, MX1 and 4 T1; and a non-small cell lung cancer model, Calu6 and fibrosis [11,12,13].
Based on the role of TGF-β in patients with malignant GB, evidence of antitumor effects of TGF-β inhibitors such as galunisertib (including in a monotherapy study in glioblastoma), and a favorable short- and long-term toxicity profile [14, 15], a multicenter Phase 1b/2a clinical trial was initiated to investigate the clinical benefit of combining galunisertib with standard TMZ-based radiochemotherapy (TMZ/RTX) in patients with newly diagnosed malignant glioma.
Methods
Patients
Eligible male and female patients were 18 years and older with histologically proven, World Health Organization Grade III (Phase 1b part only) and IV (Phase 1b/2a) malignant glioma. Patients with newly diagnosed and untreated intracranial GB including lower grade glioma, which evolved into GB were eligible. Patients with moderate or severe cardiac disease were not eligible. Adequate hematologic, hepatic, and renal function, and a performance status of ≤ 1 on the Eastern Cooperative Oncology Group (ECOG) scale were required. Concurrent use of stereotactic radiosurgery was not allowed. A biopsy or resection was required no more than 6 weeks prior to treatment and an MRI was required within 72 h after surgery; measurable or assessable disease was not required. Patients were required to begin study treatment within 2–6 weeks after surgery.
This study was conducted according to the principles of good clinical practice, applicable laws and regulations, and the Declaration of Helsinki. The protocol was approved by each institution’s review board. This study was conducted in 9 centers in 3 countries. Between April 2011 and August 2015, 101 patients entered the study but only 75 patients were enrolled and received at least one dose of galunisertib or TMZ (patients on therapy; Online Resource: Supplemental Fig. 1). All patients provided written informed consent. This trial is registered with ClinicalTrials.gov (NCT01220271).
Study design
In Phase 1b, two dose levels of galunisertib (2 cohorts: 160 mg/day or 300 mg/day) in combination with radiochemotherapy were studied to determine the dose for the Phase 2a portion of the study (Online Resource: Supplemental Fig. 2A). In Phase 2a, eligible patients were enrolled, and randomized (3:1) to either galunisertib at 300 mg/day plus radiochemotherapy, or to a control arm of radiochemotherapy (Online Resource: Supplemental Fig. 2A). Patients received galunisertib on an intermittent dose regimen of 14 days on/14 days off for a 28-day cycle (Online Resource: Supplemental Fig. 2B).
Study treatment
RTX consisted of 30 fractions at 1.8 to 2.0 Gy/dose (5 days a week for 6 weeks) for a total dose up to 60 Gy (Online Resource: Supplemental Fig. 2B). Galunisertib was given orally twice daily as 150 mg tablets for 14 days on/14 days off. TMZ was administered as recommended [2]. All patients received at least 6 cycles of therapy until disease progression, death, or discontinuation due to adverse events (AEs), or other reasons.
Safety assessments
Safety was evaluated on all patients (Phase 1b and 2a) who received at least one dose of galunisertib or TMZ. Safety analyses included AE rates, laboratory and non-laboratory changes, physical examination and other safety observations including cardiac safety, such as echocardiography/Doppler, chest CT scan, and cardiac plasma markers (brain natriuretic protein, Troponin I, Cystatin C and high sensitivity C-reactive protein).
Efficacy assessments
Primary objective of the Phase 1b study was to determine the safe and tolerable Phase 2a dose of galunisertib in patients treated concomitantly with radiochemotherapy, and the pharmacokinetics (PK) of galunisertib in combination with TMZ.
Primary objective of the Phase 2a study was to confirm the tolerability, and evaluate the pharmacodynamic (PD) effect on T-cells of galunisertib when combined with TMZ-based radiochemotherapy in patients with GB, as measured by changes in response biomarkers and their relationship to clinical benefit (overall survival [OS]). The secondary objectives were to evaluate time-to-event variables such as progression-free survival (PFS), time-to-treatment failure (TTF), time-to-tumor progression (TTP), duration-to-tumor response (DTR), overall response rate and clinical benefit rate. Galunisertib PK was also characterized (Online Resource: Supplemental Methods). Assessment of tumor response was based on Response Assessment in Neuro-Oncology (RANO) criteria [16] (Online Resource: Supplemental Methods).
Pharmacodynamics of biomarkers
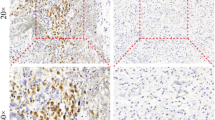
Tumor tissue and blood samples were collected at baseline and at specified times post-baseline. The baseline expression of tissue biomarkers including glial fibrillary acidic protein (GFAP), Ki67, CD3, phospho-SMAD2 (pSMAD2), and isocitrate dehydrogenase 1 (IDH1) R132H was evaluated by immunohistochemistry staining and scoring method as described previously [17] (Online Resource: Supplemental Methods).
Patients’ hematology, and expression of lactate dehydrogenase (LDH), YKL-40, and serum S100β were determined by clinical laboratory tests. Plasma TGF-β and MDC/CCL22 were measured by enzyme-linked immunosorbent assay (ELISA) (R&D systems), and multi-analyte immunoassay panel (MAIP) of 47 analytes (Myriad/RBM), respectively.
Blood samples from patients were collected and prepared for flow cytometry by Quintiles laboratories (Durham, NC) to determine the expression of CD3+ T cell subsets, such as CD4+ and CD8+, and T regulatory cells defined as CD4 + CD25 + CD127-FoxP3+. Cell staining strategy is described in Online Resource: Supplemental Methods.
Statistical methods
Patient disposition, demographic, safety, drug-related treatment-emergent adverse events (TEAEs), and response data were summarized using patient number, frequency counts, or percentages as appropriate. The safety analysis was based on summaries of AEs reported in Common Terminology Criteria for Adverse Events (CTCAE) version 4.0, and possibly drug related.
All time-to-event variables were analyzed using the Kaplan-Meier method with 90% confidence interval (CI). Univariate Cox models were used to evaluate results for potential prognostic markers by considering their impact on OS and PFS. Continuous markers were first converted to 2-level categorical variables by dichotomizing at the median and hazard ratios between treatment arms estimated for each level.
The absolute cell number of Treg cells, CD4+, and CD8+ T cells from each patient were presented in profile plots together with the geometric mean and 90% CI at baseline, Day 42 and Day 182 for each cell type. Pair-wise t-Tests were used to estimate the change from baseline to Day 42 for T cell subsets in each arm.
Results
Phase 1b
A Phase 1b study was performed to determine a safe and tolerable Phase 2a dose of galunisertib in combination with radiochemotherapy in patients with GB (Online Resource: Supplemental Fig. 1). PK analysis for galunisertib was also completed at two dose levels of galunisertib (160 mg/day [n = 10] or 300 mg/day [n = 9]) given to Phase 1b eligible patients (Online Resource: Supplemental Table 2). The dose escalation of galunisertib to 300 mg/day did not increase the toxicity profile, and overlapping toxicity was not observed when combined with radiochemotherapy (Online Resource: Supplemental Table 3). The Phase 1b PK data were consistent with previous PK analyses of galunisertib (Online Resource Supplemental Fig. 4A-C). Based on overall toxicity and PK information from Phase 1b, 300 mg/day of galunisertib was selected for the Phase 2a part of the study (Online Resource: Supplemental Results).
Patient dispositions, demographics, and baseline characteristics
A total of 59 patients from multiple centers were randomly assigned to the Phase 2a study, and 56 patients received at least one dose of galunisertib at 300 mg/day [14] concomitantly with TMZ-based radiochemotherapy (n = 40) or TMZ-based radiochemotherapy (n = 16; Fig. 1). Among the Phase 2a patients, 38/56 (67.9%) had received complete or partial surgery as the only prior treatment for their disease; 26/40 (65%) patients who had prior surgery were treated with galunisertib plus radiochemotherapy; and 12/16 (75%) patients were treated in the radiochemotherapy alone arm (Table 1).
Treatment discontinuation
The major reason for treatment discontinuation was progressive disease (37/56 [66.1%] (Fig. 1). By the end of the study, 42/56 (75%) patients from the two treatment arms had died (galunisertib plus radiochemotherapy, 31/40 [77.5%]; radiochemotherapy, 11/16 [68.8%]). Of those who died, 35/56 [62.5%] were due to disease progression, 3/56 [5.4%] were due to AEs that started 30 days after study treatment discontinuation and cause of death was not reported for 4/56 [7.1%]). Among the 56 patients enrolled in the Phase 2a clinical trial, 28 (50%) patients moved to other anti-cancer therapies (mainly bevacizumab and TMZ) after treatment discontinuation due to disease progression (Fig. 1).
Efficacy of treatment
Overall survival was 18.2 months (95% CI: 13.4, 20.6 months) in the galunisertib plus radiochemotherapy arm compared to 17.9 months (95% CI: 10.7, 24 months) in the radiochemotherapy arm (Fig. 2a-c). Galunisertib plus radiochemotherapy, and radiochemotherapy alone had a censoring rate of 22.5% and 31.3%, respectively.
Summary of treatment responses. Kaplan-Meier estimates of OS (a), and PFS (b). Summary of OS, PFS, TTF, TTP, and DTR (c). Abbreviations: m = months; OS = overall survival; PFS = progression-free survival; TFF = time-to-treatment failure; TTP = time-to-tumor progression; DTR = duration of tumor response; Gal = galunisertib; TMZ = temozolomide; RTX = radiation; NR = Not reported
The galunisertib plus radiochemotherapy arm showed a median PFS of 7.6 months (95% CI: 6.1, 10.4 months), and the probability that PFS at 12 and 24 months, was 25% (90% CI: 14, 37%) and 5% (90% CI: 1, 14%), respectively (Fig. 2b and c). In comparison, the radiochemotherapy arm had a median PFS of 11.5 months (95% CI: 5.4, 15.9 months) (Fig. 2b and c).
Assessment of tumor response showed that 3 out of 40 patients (7.5% [90% CI: 2.1, 18.3%]) from galunisertib plus radiochemotherapy arm had a complete response compared to none in radiochemotherapy arm (Online Resource: Supplemental Table 1). Therefore, the overall disease control rate in the galunisertib plus radiochemotherapy arm was higher than in the radiochemotherapy arm (80% [90% CI: 66.8, 89.6%] vs 56.3% [90% CI: 33.3, 77.3]).
Safety profile (AEs)
Possible all grade drug-related TEAEs (determined by CTCAE grade) occurring at a frequency of ≥ 10% of patients are described in Table 2. The most common (≥ 20%) all grade laboratory events in galunisertib plus radiochemotherapy arm were platelet count decreased (45%), lymphocyte count decreased (32.5%), and white blood cells decreased (30%). The percentage of grade 3–4 drug-related TEAEs was higher in patients treated with galunisertib plus radiochemotherapy compared to radiochemotherapy alone. Grade 3–4 most common drug-related TEAEs (≥ 10%) were decreases in platelet, lymphocyte, and white blood cell count. The most commonly reported (≥ 20%) all grade non-laboratory events in the galunisertib plus radiochemotherapy arm were fatigue (62.5%), nausea (52.5%), constipation (40%), alopecia (40%), vomiting (30%), and appetite decreased (20%).
Correlation between biomarkers and clinical benefit
Describing and comparing the effect of galunisertib in combination with TMZ-based radiochemotherapy on major subsets of circulating immune cells, particularly Tregs (CD4 + CD25 + CD127-FoxP3+ T cells), was one of the main translational objectives of this study (Online Resource: Supplemental Fig. 3). The analysis of OS/PFS across baseline biomarkers showed no association between baseline Tregs and OS/PFS (Online Resource: Supplemental Fig. 3A and 3B). The subgroup most favoring galunisertib plus radiochemotherapy treatment compared to control was a high ratio of CD4/CD8, however it was not statistically significant.
Next, we evaluated the T cell counts in both treatment arms every 2 weeks for 24 weeks (Fig. 3a). Variability within and between patients was observed, but when the geometric means were assessed at baseline, Day 42 (end of radiation therapy), and Day 182 (adjuvant phase), it was apparent that CD4 and CD8 lymphocytes in galunisertib plus radiochemotherapy arm were numerically decreased during radiochemotherapy (i.e., Day 42) as previously reported for CD4 T cells [18]. A pair-wise T-test analysis comparing the geometric mean of CD4, CD8, and Treg cells at baseline and Day 42 showed a significant decrease in these cell types in the galunisertib plus radiochemotherapy arm (Baseline vs Day 42: 545.0 vs 260.2 [CD4]; 227.2 vs 131.8 [CD8]; 19.8 vs 12.1 [Treg]; Fig. 3b). After radiation, the cell counts stayed steady or slightly recovered over time when galunisertib and TMZ were given as an adjuvant treatment. After 200 days of galunisertib plus radiochemotherapy treatment, approximately 22 weeks after radiation (≈ Cycle 8) and during adjuvant treatment with TMZ, we observed two clusters of patients, one with a high number of CD8 T cells (11/16 patients), the other with a low cell number (5/16 patients) by a cutoff of around 120 cells/μl (Fig. 3a). This may suggest that galunisertib treatment may provide some protective effect on CD8 T cell population in a subset of patients.
Characterization of the changes in the major T cell subsets in Phase 2a. a Absolute numbers of CD4 + CD25 + CD127-FoxP3+ T (Tregs), CD4+, and CD8+ T cells are reported over time from the first dose of treatment. Each gray line represents a patient. Solid and dashed lines connect the geometric mean (error bars, 90% CI) at baseline, Day 42 (end of radiation phase), and Day 182 (adjuvant phase). Vertical dotted line indicates the end of the chemoradiotherapy treatment and the beginning of the adjuvant phase. b Geometric mean, with 90% confidence interval, at baseline, Day 42, and Day 182. The p value from Pair-wise t-Test compares baseline and Day 42 within each arm. Note: Day42 = End of Radiation Phase, Cycle 2 Day 14; Day182 = Cycle 7 day 14; P value = Pair-wise t-Test for Comparing Baseline and Day42. Abbreviations: Gal = galunisertib; TMZ = temozolomide; RTX = radiation
Previous studies identified IDH1 R132H mutation as a positive prognostic marker of GB that occurs with a prevalence of almost 85% in secondary GB and approximately 5% in primary GB [19]. In the present study, the IDH1 R132H mutation was found on 6 of the 78 (8%) Phase 1b/2a-tested patients and all 6 were treated with galunisertib plus radiochemotherapy, 4 in the Phase 1b Cohort (data not shown) and 2 in the Phase 2a Cohort (Online Resource: Supplemental Table 4).
Prior to therapy, the expression of the following known tumor tissue biomarkers CD3, Ki67, GFAP, and pSMAD2 were assessed (Online Resource: Supplemental Table 4). No association between these factors and clinical outcome were identified (data not shown). In addition, the PD analysis conducted to determine the effect of galunisertib plus radiochemotherapy treatment on plasma markers (LDH, YKL-40, S100β, TGF-β and MDC/CCL22) did not find any association between the treatment and biomarkers (data not shown).
Discussion
We here report the efficacy, safety, and PD of galunisertib combined with radiochemotherapy in newly diagnosed malignant glioma. The overall toxicity and PK results from the Phase 1b study (Online Resource: Supplemental Results) were used to determine the recommended Phase 2a dose. Additionally, PK studies done during Phase 2a showed that the plasma levels of galunisertib were not altered when combined with TMZ and radiation (Online Resource: Supplemental Fig. 4) and achieved the targeted biologically effective dose level.
While both treatments showed comparable results for median OS (18.2 vs 17.9 months), the galunisertib plus radiochemotherapy group had a shorter estimated PFS than the radiochemotherapy group (7.6 vs 11.5 months). This difference might be explained by the small number of patients in both arms or the earlier withdrawal of patients from galunisertib plus radiochemotherapy arm. For example, 55% of patients from the experimental arm were moved to subsequent therapies, versus 37.5% of patients from control received other therapies (Fig. 1).
The overall safety data across treatment arms was similar; however, the frequency of grade 3–4 toxicities was higher in the galunisertib plus radiochemotherapy arm. There was a severe case of myeloablative marrow aplasia during the first cycle of treatment in a Phase 1a patient; this finding is more likely related to the known side effect of TMZ and radiation than to galunisertib treatment [20]. Galunisertib was not associated with bone marrow side effects in preclinical toxicology studies evaluating galunisertib in human bone marrow assays or in other combination studies with chemotherapeutic agents [14].
In addition, because cardiovascular toxicities are associated with small molecule inhibitors of TGF-β signaling in preclinical toxicology studies [21], cardiac toxicity was monitored in all patients. Galunisertib treatment did not show any clinically significant cardiac safety concerns, which are consistent with previous reports for a TGF-β small molecule inhibitor [22].
Biomarker studies did not find any correlation between baseline T cell subsets (including Tregs) and OS or PFS (Online Resource: Supplemental Fig. 3A and 3B). As reported by others, the CD4+, CD8+, and Treg cells count at 10 weeks post radiochemotherapy treatment were numerically decreased [23, 24]. The longitudinal analysis shows early decrease of CD4+ and CD8+ T cell counts during radiation, followed by a steady phase or a slight recovery in these cells over time within the galunisertib plus radiochemotherapy arm, while the pattern of CD4+, CD8+, and Treg cell counts were steady over time in the radiochemotherapy arm during both radiation and post-radiation phases. In other diseases, such as lung cancer, transient decreases in CD8+ T cells followed by an increase is associated with better OS [25]. Hence, the relevance of our observation needs further examination in order to decide whether such a response would be also expected in GB patients.
An exploratory analysis was performed to examine whether any two clusters of patients with respect to OS and PFS emerged after 200 days of galunisertib plus radiochemotherapy treatment (Fig. 3a). This limited analysis set showed that the 5 patients with a low number of CD8+ T cells had a mean OS of 25.5 months and mean PFS of 14.4 months, and the 11 patients with a higher number of CD8+ cells had a mean OS of 19.4 and mean PFS of 13.1 months. However, these observations need further confirmation in larger cohorts of patients.
Furthermore, we found no association between OS and MDC/CCL22 contrary to reports for second line treatment of GB patients [26]. It is possible that baseline levels of MDC/CCL22 are different between first and second line patients. Additionally, we found no association between pSMAD2 levels in tumor tissue and OS. The presence of CD3+ T cells in tumor tissue was not associated with OS changes. These findings are different from those reported for the second line patients treated with galunisertib [17].
TGF-β is a major driver of glioma progression, via its role in tumor cell proliferation and invasion, angiogenesis, and immune suppression within the tumor microenvironment [27]. Blocking TGF-β signaling by inhibition of its receptor TGF-β RI is one strategy for abrogating its pro-tumorigenic effects. Galunisertib is one of the only drugs in development designed to specifically target TGF-β RI; it is furthest along the clinical trial pipeline [28], not only in the setting of recurrent glioma/GB (in combination with TMZ/RTX in the current study and in combination with lomustine in [15, 26]), but also for other solid tumors. Galunisertib is currently being evaluated in Phase 1/2 or Phase 2 studies in combination with immune checkpoint inhibitors [29, 30], sorafenib [31], and gemcitabine [32]. In a Phase 2 study in patients with pancreatic cancer, the first line treatment of galunisertib in combination with gemcitabine resulted in an OS benefit of 8.9 months compared to 7.1 months for patients receiving gemcitabine alone (hazard ratio [HR], 0.79; 95% CI, 0.59–1.09) [32]. In HCC patients with elevated alpha-fetoprotein prior to treatment and who had previously progressed on sorafenib or were considered not eligible to receive sorafenib, galunisertib monotherapy achieved a median OS of 7.3 months (95% CI, 4.9–10.5). OS was longer for those patients who showed reduced alpha-fetoprotein (>20% from baseline) compared to non-responders (21.5 months vs 6.8 months) [33]. While these signals were encouraging, the sponsor discontinued future clinical development for galunisertib in mid-2017 [34]. Other TGF-β RI inhibitory drugs in early clinical development (Phase 1) include LY3200882 [35] and vactosertib [36], however there are no published reports of efficacy of these compounds as of yet. In contrast to these small molecule approaches, large molecule development has had advances, including M7824 (bintrafusp alfa), which is currently being evaluated in registration studies, including for NCSLC [37].
In conclusion, the combination of galunisertib with standard radiochemotherapy did not accentuate the toxicity profile of the radiochemotherapy. Even though survival probability was unchanged between the two treatments and PFS was reduced in the galunisertib plus radiochemotherapy arm, the disease control rate was higher in the galunisertib plus radiochemotherapy treatment when compared to radiochemotherapy treatment alone. Due to new R&D priorities, Eli Lilly discontinued the development of galunisertib in 2017 [34].
References
Glioblastoma Facts and Figures. National Brain Tumor Society. https://braintumor.org/take-action/about-gbm/. Accessed 17 Jan 2020
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. https://doi.org/10.1056/NEJMoa043330
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K, Hau P, Brandes AA, Gijtenbeek J, Marosi C, Vecht CJ, Mokhtari K, Wesseling P, Villa S, Eisenhauer E, Gorlia T, Weller M, Lacombe D, Cairncross JG, Mirimanoff RO (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10(5):459–466. https://doi.org/10.1016/S1470-2045(09)70025-7
Roszman T, Elliott L, Brooks W (1991) Modulation of T-cell function by gliomas. Immunol Today 12(10):370–374. https://doi.org/10.1016/0167-5699(91)90068-5
Wick W, Naumann U, Weller M (2006) Transforming growth factor-beta: a molecular target for the future therapy of glioblastoma. Curr Pharm Des 12(3):341–349
Gatza CE, Oh SY, Blobe GC (2010) Roles for the type III TGF-beta receptor in human cancer. Cell Signal 22(8):1163–1174. https://doi.org/10.1016/j.cellsig.2010.01.016
Derynck R, Akhurst RJ, Balmain A (2001) TGF-beta signaling in tumor suppression and cancer progression. Nat Genet 29(2):117–129. https://doi.org/10.1038/ng1001-117
Derynck R, Zhang Y, Feng XH (1998) Smads: transcriptional activators of TGF-beta responses. Cell 95(6):737–740
Shi Y, Massague J (2003) Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell 113(6):685–700
Sawyer JS, Anderson BD, Beight DW, Campbell RM, Jones ML, Herron DK, Lampe JW, McCowan JR, McMillen WT, Mort N, Parsons S, Smith EC, Vieth M, Weir LC, Yan L, Zhang F, Yingling JM (2003) Synthesis and activity of new aryl- and heteroaryl-substituted pyrazole inhibitors of the transforming growth factor-beta type I receptor kinase domain. J Med Chem 46(19):3953–3956. https://doi.org/10.1021/jm0205705
Maier A, Peille AL, Vuaroqueaux V, Lahn M (2015) Anti-tumor activity of the TGF-beta receptor kinase inhibitor galunisertib (LY2157299 monohydrate) in patient-derived tumor xenografts. Cell Oncol (Dordr) 38(2):131–144. https://doi.org/10.1007/s13402-014-0210-8
Herbertz S, Sawyer JS, Stauber AJ, Gueorguieva I, Driscoll KE, Estrem ST, Cleverly AL, Desaiah D, Guba SC, Benhadji KA, Slapak CA, Lahn MM (2015) Clinical development of galunisertib (LY2157299 monohydrate), a small molecule inhibitor of transforming growth factor-beta signaling pathway. Drug Des Dev Ther 9:4479–4499. https://doi.org/10.2147/DDDT.S86621
Zhang M, Kleber S, Rohrich M, Timke C, Han N, Tuettenberg J, Martin-Villalba A, Debus J, Peschke P, Wirkner U, Lahn M, Huber PE (2011) Blockade of TGF-beta signaling by the TGFbetaR-I kinase inhibitor LY2109761 enhances radiation response and prolongs survival in glioblastoma. Cancer Res 71(23):7155–7167. https://doi.org/10.1158/0008-5472.CAN-11-1212
Rodon J, Carducci M, Sepulveda-Sanchez JM, Azaro A, Calvo E, Seoane J, Brana I, Sicart E, Gueorguieva I, Cleverly A, Pillay NS, Desaiah D, Estrem ST, Paz-Ares L, Holdhoff M, Blakeley J, Lahn MM, Baselga J (2015) Pharmacokinetic, pharmacodynamic and biomarker evaluation of transforming growth factor-beta receptor I kinase inhibitor, galunisertib, in phase 1 study in patients with advanced cancer. Investig New Drugs 33(2):357–370. https://doi.org/10.1007/s10637-014-0192-4
Rodon J, Carducci MA, Sepulveda-Sanchez JM, Azaro A, Calvo E, Seoane J, Brana I, Sicart E, Gueorguieva I, Cleverly AL, Pillay NS, Desaiah D, Estrem ST, Paz-Ares L, Holdhoff M, Blakeley J, Lahn MM, Baselga J (2015) First-in-human dose study of the novel transforming growth factor-beta receptor I kinase inhibitor LY2157299 monohydrate in patients with advanced cancer and glioma. Clin Cancer Res 21(3):553–560. https://doi.org/10.1158/1078-0432.ccr-14-1380
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E, Degroot J, Wick W, Gilbert MR, Lassman AB, Tsien C, Mikkelsen T, Wong ET, Chamberlain MC, Stupp R, Lamborn KR, Vogelbaum MA, van den Bent MJ, Chang SM (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28(11):1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Capper D, von Deimling A, Brandes AA, Carpentier AF, Kesari S, Sepulveda-Sanchez JM, Wheeler HR, Chinot O, Cher L, Steinbach JP, Specenier P, Rodon J, Cleverly A, Smith C, Gueorguieva I, Miles C, Guba SC, Desaiah D, Estrem ST, Lahn MM, Wick W (2017) Biomarker and histopathology evaluation of patients with recurrent Glioblastoma treated with Galunisertib, Lomustine, or the combination of Galunisertib and Lomustine. Int J Mol Sci 18(5). https://doi.org/10.3390/ijms18050995
Grossman SA, Ye X, Lesser G, Sloan A, Carraway H, Desideri S, Piantadosi S, Consortium NC (2011) Immunosuppression in patients with high-grade gliomas treated with radiation and temozolomide. Clin Cancer Res 17(16):5473–5480. https://doi.org/10.1158/1078-0432.CCR-11-0774
Gessler F, Zappi J, Konczalla J, Bernstock JD, Forster MT, Wagner M, Mittelbronn M, Seifert V, Senft C (2017) Secondary Glioblastoma: molecular and clinical factors that affect outcome after malignant progression of a lower grade tumor. World Neurosurg 102:49–55. https://doi.org/10.1016/j.wneu.2017.02.104
Kourelis TV, Buckner JC, Gangat N, Patnaik MM (2015) Temozolomide induced bone marrow suppression--a single institution outcome analysis and review of the literature. Am J Hematol 90(9):E183–E184. https://doi.org/10.1002/ajh.24066
Stauber AJ, Credille KM, Truex LL, Ehlhardt WJ, Young JK (2014) Nonclinical safety evaluation of a transforming growth factor ß receptor I kinase inhibitor in Fischer 344 rats and beagle dogs. J Clin Toxicol 4(3):1–10. https://doi.org/10.4172/2161-0495.196
Kovacs RJ, Maldonado G, Azaro A, Fernandez MS, Romero FL, Sepulveda-Sanchez JM, Corretti M, Carducci M, Dolan M, Gueorguieva I, Cleverly AL, Pillay NS, Baselga J, Lahn MM (2015) Cardiac safety of TGF-beta receptor I kinase inhibitor LY2157299 monohydrate in Cancer patients in a first-in-human dose study. Cardiovasc Toxicol 15(4):309–323. https://doi.org/10.1007/s12012-014-9297-4
Ellsworth S, Balmanoukian A, Kos F, Nirschl CJ, Nirschl TR, Grossman SA, Luznik L, Drake CG (2014) Sustained CD4+ T cell-driven lymphopenia without a compensatory IL-7/IL-15 response among high-grade glioma patients treated with radiation and temozolomide. Oncoimmunology 3(1):e27357. https://doi.org/10.4161/onci.27357
Fadul CE, Fisher JL, Gui J, Hampton TH, Cote AL, Ernstoff MS (2011) Immune modulation effects of concomitant temozolomide and radiation therapy on peripheral blood mononuclear cells in patients with glioblastoma multiforme. Neuro-Oncology 13(4):393–400. https://doi.org/10.1093/neuonc/noq204
McCoy MJ, Lake RA, van der Most RG, Dick IM, Nowak AK (2012) Post-chemotherapy T-cell recovery is a marker of improved survival in patients with advanced thoracic malignancies. Br J Cancer 107(7):1107–1115. https://doi.org/10.1038/bjc.2012.362
Brandes AA, Carpentier AF, Kesari S, Sepulveda-Sanchez JM, Wheeler HR, Chinot O, Cher L, Steinbach JP, Capper D, Specenier P, Rodon J, Cleverly A, Smith C, Gueorguieva I, Miles C, Guba SC, Desaiah D, Lahn MM, Wick W (2016) A phase II randomized study of galunisertib monotherapy or galunisertib plus lomustine compared with lomustine monotherapy in patients with recurrent glioblastoma. Neuro-Oncology 18(8):1146–1156. https://doi.org/10.1093/neuonc/now009
Han J, Alvarez-Breckenridge CA, Wang QE, Yu J (2015) TGF-beta signaling and its targeting for glioma treatment. Am J Cancer Res 5(3):945–955
de Gramont A, Faivre S, Raymond E (2017) Novel TGF-beta inhibitors ready for prime time in onco-immunology. Oncoimmunology 6(1):e1257453. https://doi.org/10.1080/2162402x.2016.1257453
Melisi D, Hollebecque A, Oh D-Y, Calvo E, Varghese AM, Borazanci EH, Mercade TM, Simionato F, Park JO, Bendell JC, Faivre SJ, Zhao Y, Gueorguieva I, Man M, Estrem S, Benhadji KA, Lanasa M, Guba SC, Garcia-Carbonero R (2019) A phase Ib dose-escalation and cohort-expansion study of safety and activity of the transforming growth factor (TGF) β receptor I kinase inhibitor galunisertib plus the anti-PD-L1 antibody durvalumab in metastatic pancreatic cancer [abstract]. J Clin Oncol 37(15_suppl):4124–4124. https://doi.org/10.1200/JCO.2019.37.15_suppl.4124
Nadal E, Saleh MN, Aix SP, Olza MOd, Patel SP, Antonia SJ, Zhao Y, Gueorguieva I, Man M, Estrem ST, Avsar E, Lin WH, Benhadji K, Guba S, Diaz IA A Phase 1b/2 study of galunisertib in combination with nivolumab in solid tumors and NSCLC [abstract]. In: SITC 2019, National Harbor, Maryland, Nov 6–10 2019. p P413
Kelley RK, Gane E, Assenat E, Siebler J, Galle PR, Merle P, Hourmand IO, Cleverly A, Zhao Y, Gueorguieva I, Lahn M, Faivre S, Benhadji KA, Giannelli G (2019) A phase 2 study of Galunisertib (TGF-beta1 receptor type I inhibitor) and Sorafenib in patients with advanced hepatocellular carcinoma. Clin Transl Gastroenterol 10(7):e00056. https://doi.org/10.14309/ctg.0000000000000056
Melisi D, Garcia-Carbonero R, Macarulla T, Pezet D, Deplanque G, Fuchs M, Trojan J, Oettle H, Kozloff M, Cleverly A, Smith C, Estrem ST, Gueorguieva I, Lahn MMF, Blunt A, Benhadji KA, Tabernero J (2018) Galunisertib plus gemcitabine vs. gemcitabine for first-line treatment of patients with unresectable pancreatic cancer. Br J Cancer 119(10):1208–1214. https://doi.org/10.1038/s41416-018-0246-z
Faivre S, Santoro A, Kelley RK, Gane E, Costentin CE, Gueorguieva I, Smith C, Cleverly A, Lahn MM, Raymond E, Benhadji KA, Giannelli G (2019) Novel transforming growth factor beta receptor I kinase inhibitor galunisertib (LY2157299) in advanced hepatocellular carcinoma. Liver Int 39(8):1468–1477. https://doi.org/10.1111/liv.14113
Lilly puts two-thirds of midphase cancer pipeline up for sale in major shake-up of R&D priorities [news release]. FierceBiotech; https://www.fiercebiotech.com/biotech/lilly-puts-two-thirds-mid-phase-cancer-pipeline-up-for-sale-major-shake-up-r-d-priorities. Accessed 17 Jan 2020
Yap T, Baldini C, Massard C, Gueorguieva I, Zhao Y, Schmidt S, Man M, Estrem S, Benhadji K, Vieito M (2018) First-in-human phase 1 dose-escalation trial of the potent and selective next generation transforming growth factor-β receptor type 1 (TGF-βR1) inhibitor LY3200882 in patients with advanced cancers [abstract]. J Immunother Cancer 6(Suppl1):O30
Keedy VL, Bauer TM, Clarke JM, Hurwitz H, Baek I, Ha I, Ock C-Y, Nam SY, Kim M, Park N, Kim JY, Kim S-J (2018) Association of TGF-β responsive signature with anti-tumor effect of vactosertib, a potent, oral TGF-β receptor type I (TGFBRI) inhibitor in patients with advanced solid tumors. J Clin Oncol 36(15_suppl):3031–3031. https://doi.org/10.1200/JCO.2018.36.15_suppl.3031
ClinicalTrials.gov. M7824 versus pembrolizumab as a first-line (1L) treatment in participants with programmed death ligand 1 (PD-L1) expressing advanced non-small cell lung cancer (NSCLC). https://clinicaltrials.gov/ct2/show/NCT03631706
Acknowledgements
The authors thank Loretta Wilcox for contributions to this manuscript, and Annie-Carole Trampont, PhD, Eli Lilly and Company, for her assistance in writing this manuscript. We thank patients and their families who participated in this trial, and all site staff and investigators at the institutions, and the trial personnel at Eli Lilly and Company.
Authorship
All authors have contributed to the conception and the design of the work, the data acquisition, the analysis and/or the interpretation of the data, in addition to drafting and/or the critical revision of the manuscript.
Funding
Open Access funding provided by Projekt DEAL. This trial was funded by Eli Lilly and Company.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AD serves on Advisory Board for Orbus Therapeutics, and Celgene, holds stock options from ISTARI Oncology, and letters of patent for Oncolytic Poliovirus for human tumors. AD’s institution receives research funding from Genentech/Roche, Celldex, Triphase Accelerator Corp., Eli Lilly and Company, Symphogen A/S, Pfizer, and Orbus Therapeutics. CS serves on Advisory Board for Pfizer, IPSEN, BMS, Astellas, Sanofi, Bayer, and MSD; is a speaker for BMS, Pfizer, IPSEN, and Astellas; received travel reimbursement from BMS, Pfizer, and Roche; reports receiving research/clinical funding from Roche. PF is consultant for AbbVie Inc., Ziopharm, Tocagen Inc., BMS and L.E.K. JR reports non-financial support and reasonable reimbursement for travel from European Journal of Cancer, Vall d’Hebron Institut of Oncology, Chinese University of Hong Kong, SOLTI, Elsevier, GLAXOSMITHKLINE; receiving consulting and travel fees from Novartis, Eli Lilly and Company, Orion Pharmaceuticals, Servier Pharmaceuticals, Peptomyc, Merck Sharp & Dohme, Kelun Pharmaceutical/Klus Pharma, Spectrum Pharmaceuticals Inc., Pfizer, Roche Pharmaceuticals, Ellipses Pharma (including serving on the scientific advisory board from 2015-present), receiving research funding from Bayer and Novartis, and serving as investigator in clinical trials with Spectrum Pharmaceuticals, Tocagen, Symphogen, BioAtla, Pfizer, GenMab, CytomX, KELUN-BIOTECH, Takeda-Millenium, GLAXOSMITHKLINE, IPSEN and travel fees from ESMO, US Department of Defense, Louisiana State University, Hunstman Cancer Institute, Cancer Core Europe, Karolinska Cancer Institute and King Abdullah International Medical Research Center (KAIMRC). SE, IG, and TB are employees of Eli Lilly and Company and may hold company stocks. ML, SG, and ALC are former employees of Eli Lilly and Company and hold company stocks. The other authors report no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was registered at ClinicalTrials.gov as NCT01220271.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 661 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wick, A., Desjardins, A., Suarez, C. et al. Phase 1b/2a study of galunisertib, a small molecule inhibitor of transforming growth factor-beta receptor I, in combination with standard temozolomide-based radiochemotherapy in patients with newly diagnosed malignant glioma. Invest New Drugs 38, 1570–1579 (2020). https://doi.org/10.1007/s10637-020-00910-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-020-00910-9