Abstract
Background
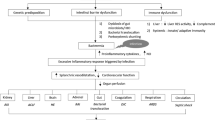
We evaluated the prevalence, risk factors, and impact of bacterial/fungal infections in acute liver failure (ALF) patients.
Methods
We analyzed clinical, biochemical, and microbiological data of ALF patients with and without bacterial/fungal infections admitted at an institute over the last 5 years.
Results
We enrolled 143 patients, 50% males, median age 25 years, with acute viral hepatitis (32.2%), drug-induced injury (18.2%), and tropical illness (14%) as aetiologies of ALF. 110 patients (76.9%) developed bacterial/fungal infections [Bacterial infection: MDR: 70%, PDR: 7%, ESBL: 40%, CRE: 30%, CRAB: 26.6%, MDR-EF: 13.3% and fungal infection: 19 (17.3%)].
On univariable analysis, SIRS (33.6% vs.3%), ICU admission (78.2% vs. 45.5%), mechanical ventilation (88.2% vs. 51.5%), inotropes (39.1% vs. 6.1%), invasive catheters (91.8% vs. 39.4%), and prolonged catheterization (6 days vs. 0 days) were significant risk factors for infections (p < 0.05, each). In contrast, SIRS and catheterization independently predicted infection on multivariable regression.
Organ failures [3 (2–4) vs. 1 (0–2)], grade-III–IV HE (67.3% vs. 33.3%), circulatory failure (39.1% vs. 6.1%), coagulopathy (INR > 2.5: 58.2% vs. 33.3%), renal injury (28.2% vs. 6.1%) (p < 0.05), MELD (32.9 ± 8.2 vs. 26.7 ± 8.3) and CPIS [3(2–4) vs. 2(0–2)] were higher in infected vs. non-infected patients (p < 0.001). 30-day survival was significantly lower in infected vs. non-infected patients (17.3% vs. 75.8%, p < 0.001), while no patient survived with fungal infections. Refractory septic shock was the commonest cause of mortality in patients.
Conclusions
Infections due to MDR organisms are high, fungal infections are fatal, and refractory septic shock is the dominant reason for mortality, implying bacterial and fungal infections as the major killer in ALF patients.



Similar content being viewed by others
Data Availability
Data are not publicly available but is available by contacting the corresponding author.
Abbreviations
- ALF:
-
Acute liver failure
- MDR:
-
Multidrug-resistant
- PDR:
-
Pandrug-resistant
- ESBLs:
-
Extended spectrum beta-lactamase producing organisms
- CRE:
-
Carbapenem-resistant Enterobacteriaceae
- CRAB:
-
Carbapenem-resistant Acinetobacter baumannii
- MDR-ef:
-
Multidrug-resistant Enterococcus faecium
- MELD:
-
Model for end-stage liver diseases
- CPI:
-
Score, clinical prognostic indicator score
- SIRS:
-
Systemic inflammatory response syndrome
- ICU:
-
Intensive care unit
- HE:
-
Hepatic encephalopathy
- INR:
-
International normalized ratio
- BDG:
-
Beta-D glucan
- GMI:
-
Galactomannan Index
- CDC/NHSN:
-
Centre for disease control and prevention-national heath safety network
- EORTC/MSG:
-
European organization for research and treatment of cancer mycoses study group criteria
- CSF:
-
Cerebrospinal fluid
- FNAC:
-
Fine needle aspiration cytology
- CLIF-SOFA:
-
Chronic liver failure-sequential organ failure assessment
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- MDRO:
-
Multidrug-resistant organisms
- KCC:
-
King's College criteria
- BSI:
-
Blood stream infections
- HEV:
-
Hepatitis E virus
References
Anand AC, Nandi B, Acharya SK et al. Indian National Association for the Study of the Liver Consensus Statement on Acute Liver Failure (Part 1): Epidemiology, Pathogenesis, Presentation and Prognosis. J Clin Exp Hepatol 2020;10:339–376.
Possamai LA, Thursz MR, Wendon JA et al. Modulation of monocyte/macrophage function: a therapeutic strategy in the treatment of acute liver failure. J Hepatol 2014;61:439–445.
Antoniades CG, Berry PA, Wendon JA et al. The importance of immune dysfunction in determining outcome in acute liver failure. J Hepatol 2008;49:845–861.
Antoniades CG, Quaglia A, Taams LS et al. Source and characterization of hepatic macrophages in acetaminophen-induced acute liver failure in humans. Hepatology 2012;56:735–746.
Antoniades CG, Berry PA, Davies ET et al. Reduced monocyte HLA-DR expression: a novel biomarker of disease severity and outcome in acetaminophen-induced acute liver failure. Hepatology 2006;44:34–43.
Vaquero J, Polson J, Chung C et al. Infection and the progression of hepatic encephalopathy in acute liver failure. Gastroenterology 2003;125:755–764.
Cuschieri S. The STROBE guidelines. Saudi J Anaesth 2019;13:S31–S34.
Wendon J, Cordoba J, Dhawan A et al. EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure. J Hepatol 2017;66:1047–1081.
Lee WM, Stravitz RT, Larson AM. Introduction to the revised American Association for the Study of Liver Diseases Position Paper on acute liver failure 2011. Hepatology 2012;55:965–967.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 2008;36:309–332.
Bajaj JS, O’Leary JG, Reddy KR et al. Second infections independently increase mortality in hospitalized patients with cirrhosis: the North American consortium for the study of end-stage liver disease (NACSELD) experience. Hepatology 2012;56:2328–2335.
Magiorakos AP, Srinivasan A, Carey RB et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 2012;18:268–281.
Verma N, Singh S, Taneja S et al. Invasive fungal infections amongst patients with acute-on-chronic liver failure at high risk for fungal infections. Liver Int 2019;39:503–513.
Verma N, Singh S, Singh M et al. Global epidemiological burden of fungal infections in cirrhosis patients: A systematic review with meta-analysis. Mycoses 2022;65:266–284.
Moreau R, Jalan R, Gines P et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426-37-37.e1-9.
Acharya SK, Panda SK, Saxena A et al. Acute hepatic failure in India: a perspective from the East. J Gastroenterol Hepatol 2000;15:473–479.
Rolando N, Harvey F, Brahm J et al. Fungal infection: a common, unrecognised complication of acute liver failure. J Hepatol 1991;12:1–9.
Karvellas CJ, Cavazos J, Battenhouse H et al. Effects of Antimicrobial Prophylaxis and Blood Stream Infections in Patients With Acute Liver Failure: A Retrospective Cohort Study. Clinical Gastroenterology and Hepatology. 2014;12:1942–9.e1.
Rolando N, Harvey F, Brahm J et al. Prospective study of bacterial infection in acute liver failure: an analysis of fifty patients. Hepatology 1990;11:49–53.
Rolando N, Wade J, Davalos M et al. The systemic inflammatory response syndrome in acute liver failure. Hepatology 2000;32:734–739.
Gupta T, Lochan D, Verma N et al. Prediction of 28-day mortality in acute decompensation of cirrhosis through the presence of multidrug-resistant infections at admission. J Gastroenterol Hepatol 2020;35:461–466.
Bhattacharya C, Das-Mondal M, Gupta D et al. Infection in cirrhosis: A prospective study. Ann Hepatol 2019;18:862–868.
Khuroo MS. Acute liver failure in India. Hepatology 1997;26:244–246.
Shalimar, Kedia S, Gunjan D et al. Acute Liver Failure Due to Hepatitis E Virus Infection Is Associated with Better Survival than Other Etiologies in Indian Patients. Dig Dis Sci 2017;62:1058–66.
Anand AC, Nandi B, Acharya SK et al. Erratum to “Indian National Association for the Study of Liver Consensus Statement on Acute Liver Failure (Part-2): Management of Acute Liver Failure” [J Clin Exp Hepatol 10 (2020) 477–517]. J Clin Exp Hepatol 2022;12:729–730.
Goel A, Lalruatsanga D, Himanshu D, Bharti V, Sharma D. Acute Liver Failure Prognostic Criteria: It’s Time to Revisit. Cureus 2023;15:e33810.
Kamath PS, Heimbach J, Wiesner RH. Acute Liver Failure Prognostic Scores: Is Good Enough Good Enough? Clin Gastroenterol Hepatol 2016;14:621–623.
Cholongitas E, Theocharidou E, Vasianopoulou P et al. Comparison of the sequential organ failure assessment score with the King’s College Hospital criteria and the model for end-stage liver disease score for the prognosis of acetaminophen-induced acute liver failure. Liver Transpl 2012;18:405–412.
Saluja V, Sharma A, Pasupuleti SS et al. Comparison of Prognostic Models in Acute Liver Failure: Decision is to be Dynamic. Indian J Crit Care Med 2019;23:574–581.
Dhiman RK, Jain S, Maheshwari U et al. Early indicators of prognosis in fulminant hepatic failure: an assessment of the Model for End-Stage Liver Disease (MELD) and King’s College Hospital criteria. Liver Transpl 2007;13:814–821.
Funding
None.
Author information
Authors and Affiliations
Contributions
NV designed the study, analysed the data, reviewed the manuscript. PK collected the data and drafted the manuscript. AV collected the data and revised the manuscript. PG, SR, AD, MP, ST, AD, VS, RKD revised and reviewed the manuscript. All the authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Ethical approval
This study was approved by ethics committee of Postgraduate Institute of Medical Education and Research, Chandigarh, India (NK/7445/Study/582).
Informed consent
N/A.
Research involving human and animal participants
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaur, P., Verma, N., Valsan, A. et al. Prevalence, Risk Factors, and Impact of Bacterial or Fungal Infections in Acute Liver Failure Patients from India. Dig Dis Sci 68, 4022–4038 (2023). https://doi.org/10.1007/s10620-023-07971-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07971-9