Abstract
Background
The incidence of, risk factors for, and outcomes after the development of ascites are poorly described for contemporary patients with cirrhosis.
Methods
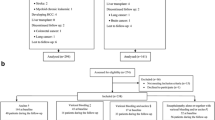
We examined data for a 20% random sample of US Medicare enrollees with cirrhosis and Part D prescription coverage from 2008 to 2019, excluding patients with heart failure and diuretic use prior to cirrhosis. Among 63,364 persons with cirrhosis, we evaluated the incidence of ascites using an Aalen–Johansen estimator. We evaluated risk factors for ascites, mortality, and mortality after ascites using multistate modeling. We determined the associations with each outcome for an array of medication exposures including nonselective beta-blockers, antiviral therapy, statins, rifaximin, anticoagulants, and metformin.
Results
The cumulative incidence of ascites was 5.1%, 9.5%, and 10.7% and 1, 3, and 5 years overall. The corresponding data for ascites requiring paracentesis were 1%, 2.1%, and 2.4%. Persons aged < 65 years, with alcohol-related cirrhosis, varices, or HE, are most likely to develop ascites. The risk of ascites was higher for persons taking any NSBB (including carvedilol) but lower for those taking atorvastatin (but not other statins) and antiviral therapy for Hepatitis C. Incident ascites was associated with increased risk of death, HR 27.6 95%CI(21.7–35.1). Survival following ascites was 1.08 years (interquartile range, IQR, 0.26–2.75), 0.38 years (IQR0.1–1.3) for those requiring paracentesis. Lipophilic statins were the only medications associated with lower mortality after ascites requiring paracentesis.
Conclusions
Ascites is associated with a high risk of death. Very few candidate therapies are associated with the reduction in the risk of ascites and mortality after ascites development.



Similar content being viewed by others
References
Tapper E, Kanwal F, Asrani S, et al. Patient reported outcomes in cirrhosis: a scoping review of the literature. Hepatology (Baltimore, Md.) 2017.
D’Amico G, Pasta L, Morabito A et al. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther 2014;39:1180–1193.
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol 2006;44:217–231.
D’Amico G, Morabito A, D’Amico M et al. Clinical states of cirrhosis and competing risks. J Hepatol 2018;68:563–576.
Jepsen P, Lash TL, Vilstrup H. The clinical course of alcoholic cirrhosis: development of comorbid diseases. A Danish nationwide cohort study. Liver Int 2016;36:1696–1703.
Jepsen P, Ott P, Andersen PK et al. Clinical course of alcoholic liver cirrhosis: A Danish population-based cohort study. Hepatology 2010;51:1675–1682.
Parikh ND, Marrero WJ, Wang J, et al. Projected increase in obesity and non‐alcoholic‐steatohepatitis–related liver transplantation waitlist additions in the United States. Hepatology 2017; doi:10.1007/s10620-021-07367-7.
Tapper EB, Henderson JB, Parikh ND, et al. Incidence of and risk factors for hepatic encephalopathy in a population‐based cohort of Americans with cirrhosis. Hepatol Commun 2019.
Tapper EB, Parikh ND, Sengupta N et al. A risk score to predict the development of hepatic encephalopathy in a population-based cohort of patients with cirrhosis. Hepatology 2018;68:1498–1507.
Scaglione S, Kliethermes S, Cao G et al. The epidemiology of cirrhosis in the United States. J Clin Gastroenterol 2015;49:690–696.
Sharpton SR, Feng S, Hameed B et al. Combined effects of recipient age and model for end-stage liver disease score on liver transplantation outcomes. Transplantation 2014;98:557.
Villanueva C, Albillos A, Genescà J et al. β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomised, double-blind, placebo-controlled, multicentre trial. The Lancet 2019;393:1597–1608.
Salehi S, Tranah TH, Lim S et al. Rifaximin reduces the incidence of spontaneous bacterial peritonitis, variceal bleeding and all-cause admissions in patients on the liver transplant waiting list. Aliment Pharmacol Ther 2019;50:435–441.
Villa E, Cammà C, Marietta M et al. Enoxaparin prevents portal vein thrombosis and liver decompensation in patients with advanced cirrhosis. Gastroenterology 2012;143:1253-1260.e4.
Rakoski MO, McCammon RJ, Piette JD et al. Burden of cirrhosis on older Americans and their families: analysis of the health and retirement study. Hepatology 2012;55:184–191.
Mapakshi S, Kramer JR, Richardson P et al. Positive predictive value of international classification of diseases, 10th revision, codes for cirrhosis and its related complications. Clin Gastroenterol Hepatol 2018;16:1677–1678.
Gonzalez JJ, Dziwis J, Patel YA, et al. Identifying ascites in patients with cirrhosis using administrative codes and diuretic use: a multicenter study. Dig Dis Sci 2022.https://doi.org/10.1007/s10620-021-07367-7
Kaplan DE, Serper M, John BV, et al. Effects of metformin exposure on survival in a large national cohort of patients with diabetes and cirrhosis. Clin Gastroenterol Hepatol 2020.
Mohanty A, Tate JP, Garcia-Tsao G. Statins are associated with a decreased risk of decompensation and death in veterans with hepatitis C–related compensated cirrhosis. Gastroenterology 2016;150:430-440.e1.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613–619.
Mellinger JL, Shedden K, Winder GS, et al. The high burden of alcoholic cirrhosis in privately insured persons in the United States. Hepatology 2018.
Allen AM, Therneau TM, Larson JJ et al. Nonalcoholic fatty liver disease incidence and impact on metabolic burden and death: A 20 year-community study. Hepatology 2018;67:1726–1736.
Lévesque LE, Hanley JA, Kezouh A et al. Problem of immortal time bias in cohort studies: example using statins for preventing progression of diabetes. Bmj 2010;340:b5087.
Jepsen P, Vilstrup H, Andersen PK. The clinical course of cirrhosis: the importance of multistate models and competing risks analysis. Hepatology 2015;62:292–302.
Sanyal AJ, Van Natta ML, Clark J et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N Eng J Med 2021;385:1559–1569.
Kimer N, Grønbæk H, Fred RG, et al. Atorvastatin for prevention of disease progression and hospitalisation in liver cirrhosis: protocol for a randomised, double-blind, placebo-controlled trial. BMJ open 2020;10.
Serper M, Weinberg EM, Cohen JB et al. Mortality and hepatic decompensation in patients with cirrhosis and atrial fibrillation treated with anticoagulation. Hepatology 2021;73:219–232.
Lai JC, Tandon P, Bernal W, et al. Malnutrition, frailty, and sarcopenia in patients with cirrhosis: 2021 practice guidance by the American association for the study of liver diseases. Hepatology 2021.
Montoliu S, Balleste B, Planas R et al. Incidence and prognosis of different types of functional renal failure in cirrhotic patients with ascites. Clin Gastroenterol Hepatol 2010;8:616–622.
Rodríguez-Vilarrupla A, Laviña B, García-Calderó H et al. PPARα activation improves endothelial dysfunction and reduces fibrosis and portal pressure in cirrhotic rats. J Hepatol 2012;56:1033–1039.
Tapper EB, Aberasturi D, Zhao Z, et al. Outcomes after hepatic encephalopathy in population‐based cohorts of patients with cirrhosis. Alimentary Pharmacol Ther 2020.
Funding
Elliot Tapper receives funding from the National Institutes of Health through NIDDK K23-DK117055. This work was supported in part by an unrestricted research grant from Valeant Pharmaceuticals (makers of Rifaximin). Valeant had no access to the data and played no role in the analysis.
Author information
Authors and Affiliations
Contributions
Elliot Tapper is the guarantor of this article. Roles: Concept: Tapper, Analysis: Tapper, Zhe, Mazumder, Parikh, Data acquisition: Tapper, Zhe, Writing: Tapper, Revision: Zhe, Mazumder, Parikh.
Corresponding author
Ethics declarations
Conflict of interest
Author declares that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tapper, E.B., Zhao, Z., Mazumder, N. et al. Incidence of, Risk Factors for, and Outcomes After Ascites in a Population-Based Cohort of Older Americans. Dig Dis Sci 67, 5327–5335 (2022). https://doi.org/10.1007/s10620-022-07454-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07454-3