Abstract
Background
Limited data are available to support current guidelines recommendations on obtaining gastric and duodenal biopsies of patients with clinical and histologic manifestations consistent with eosinophilic esophagitis (EoE) to rule out eosinophilic gastritis (EG) or duodenitis (EoD). Our study examined the prevalence of concomitant extraesophageal, gastrointestinal pathology to better characterize the diagnostic yield of additional biopsies.
Methods
This was a single-center, retrospective study which utilized ICD 9 codes (530.13) and search queries of pathology reports (“Eosinophilic esophagitis,” “EoE”) to identify EoE patients. Patient endoscopy reports, pathology reports, and office notes were manually reviewed to characterize cases.
Results
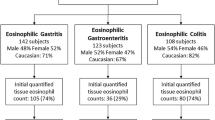
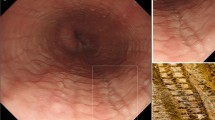
The electronic health record search yielded 1,688 EoE adults. In those who had extra-esophageal biopsies obtained, EG was identified in 34 (3.4%), H. pylori in 45 (4.6%), EoD in 27 (3.3%), and histology consistent with celiac disease in 20 (2.5%). Endoscopic abnormalities were found in the stomach of 92% of patients with EoE and EG and in the duodenum of 50% of patients with EoE and EoD. Symptoms of dyspepsia and/or abdominal pain occurred in a significantly greater proportion of patients with extraesophageal disease (64% vs. 19% in EoE group, p < 0.001). Overall, extraesophageal pathology would have been missed in 1.4% of patients lacking either symptoms or endoscopic signs suggestive of extraesophageal disease.
Conclusions
The yield of gastric and duodenal biopsies in adults with EoE is low, with 6.5% of patients demonstrating histologic features of celiac disease, Helicobacter pylori, EG, and/or EoD. Biopsies of extraesophageal, gastrointestinal sites in patients with suspected or previously diagnosed EoE should consider symptom and endoscopy manifestations as well as the potential impact of histopathologic findings on clinical management.




Similar content being viewed by others
Abbreviations
- EoE:
-
Esophagitis
- EG:
-
Eosinophilic gastritis
- EoD:
-
Eosinophilic duodenitis
- EGID:
-
Eosinophilic gastrointestinal disease
- eos/hpf:
-
Eosinophils per high-power field
- GERD:
-
Gastroesophageal reflux disease
- PPI:
-
Proton pump inhibitor
- PPIREE:
-
Proton pump inhibitor responsive esophageal eosinophilia
- EREFS:
-
Esophagitis endoscopic reference score
References
Dellon ES, Liacouras CA, Molina-Infante J, et al (2018) Updated international consensus diagnostic criteria for eosinophilic esophagitis: proceedings of the AGREE conference. Gastroenterology. 155:1022–1033 e1010.
Dellon ES, Gonsalves N, Hirano I, et al (2013) ACG clinical guideline: Evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE). Am J Gastroenterol. ;108:679–692; quiz 693.
Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3–20 e26; quiz 21–22.
Lucendo AJ, Molina-Infante J, Arias A et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United Eur Gastroenterol J. 2017;5:335–358.
Furuta GT, Liacouras CA, Collins MH et al. Eosinophilic esophagitis in children and adults: a systematic review and consensus recommendations for diagnosis and treatment. Gastroenterology. 2007;133:1342–1363.
Dellon ES, Collins MH, Bonis PA et al. Substantial variability in biopsy practice patterns among gastroenterologists for suspected eosinophilic gastrointestinal disorders. Clin Gastroenterol Hepatol. 2016;14:1842–1844.
Kaur S, Rosen JM, Kriegermeier AA, Wechsler JB, Kagalwalla AF, Brown JB. Utility of gastric and duodenal biopsies during follow-up endoscopy in children with eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2017;65:399–403.
Mukkada V, Falk GW, Eichinger CS, King D, Todorova L, Shaheen NJ. Health-related quality of life and costs associated with eosinophilic esophagitis: a systematic review. Clin Gastroenterol Hepatol. 2018;16(4):495–503 e498.
Jensen ET, Kappelman MD, Martin CF, Dellon ES. Health-care utilization, costs, and the burden of disease related to eosinophilic esophagitis in the United States. Am J Gastroenterol. 2015;110:626–632.
Shah SC, Tepler A, Peek RM, Jr., Colombel JF, Hirano I, Hirano N. Association between helicobacter pylori exposure and decreased odds of eosinophilic esophagitis-a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2019;17:2185–2198 e3.
Lucendo AJ, Arias A, Tenias JM. Systematic review: the association between eosinophilic oesophagitis and coeliac disease. Aliment Pharmacol Ther. 2014;40:422–434.
Lucendo AJ. Disease associations in eosinophilic oesophagitis and oesophageal eosinophilia. Best Pract Res Clin Gastroenterol. 2015;29:759–769.
Dellon ES, Peery AF, Shaheen NJ et al. Inverse association of esophageal eosinophilia with Helicobacter pylori based on analysis of a US pathology database. Gastroenterology. 2011;141:1586–1592.
Molina-Infante J, Gutierrez-Junquera C, Savarino E et al. Helicobacter pylori infection does not protect against eosinophilic esophagitis: results from a large multicenter case-control study. Am J Gastroenterol. 2018;113:972–979.
Mansoor E, Saleh MA, Cooper GS. Prevalence of eosinophilic gastroenteritis and colitis in a population-based study, from 2012 to 2017. Clin Gastroenterol Hepatol. 2017;15:1733–1741.
Pesek RD, Reed CC, Collins MH et al. Association between endoscopic and histologic findings in a multicenter retrospective cohort of patients with non-esophageal eosinophilic gastrointestinal disorders. Dig Dis Sci. 2020;65:2024–2035.
Pesek RD, Reed CC, Muir AB et al. Increasing rates of diagnosis, substantial co-occurrence, and variable treatment patterns of eosinophilic gastritis, gastroenteritis, and colitis based on 10-year data across a multicenter consortium. Am J Gastroenterol. 2019;114:984–994.
Lwin T, Melton SD, Genta RM. Eosinophilic gastritis: histopathological characterization and quantification of the normal gastric eosinophil content. Mod Pathol. 2011;24:556–563.
Collins MH. Histopathology of eosinophilic esophagitis. Dig Dis. 2014;32:68–73.
Genta RM, Sonnenberg A, Turner K. Quantification of the duodenal eosinophil content in adults: a necessary step for an evidence-based diagnosis of duodenal eosinophilia. Aliment Pharmacol Ther. 2018;47:1143–1150.
Collins MH. Histopathologic features of eosinophilic esophagitis and eosinophilic gastrointestinal diseases. Gastroenterol Clin North Am. 2014;43:257–268.
Kagalwalla AF, Shah A, Ritz S, Melin-Aldana H, Li BU. Cow’s milk protein-induced eosinophilic esophagitis in a child with gluten-sensitive enteropathy. J Pediatr Gastroenterol Nutr. 2007;44:386–388.
Quaglietta L, Coccorullo P, Miele E, Pascarella F, Troncone R, Staiano A. Eosinophilic oesophagitis and coeliac disease: Is there an association? Aliment Pharmacol Ther. 2007;26:487–493.
Ahmed OI, Qasem SA, Abdulsattar JA, Snow AN, Hill ID. Esophageal eosinophilia in pediatric patients with celiac disease: Is it a causal or an incidental association? J Pediatr Gastroenterol Nutr. 2015;60:493–497.
Leslie C, Mews C, Charles A, Ravikumara M. Celiac disease and eosinophilic esophagitis: a true association. J Pediatr Gastroenterol Nutr. 2010;50:397–399.
Jensen ET, Eluri S, Lebwohl B, Genta RM, Dellon ES. Increased risk of esophageal eosinophilia and eosinophilic esophagitis in patients with active celiac disease on biopsy. Clin Gastroenterol Hepatol. 2015;13:1426–1431.
Elitsur Y, Alrazzak BA, Preston D, Demetieva Y. Does Helicobacter pylori protect against eosinophilic esophagitis in children? Helicobacter. 2014;19:367–371.
Furuta K, Adachi K, Aimi M et al. Case-control study of association of eosinophilic gastrointestinal disorders with Helicobacter pylori infection in Japan. J Clin Biochem Nutr. 2013;53:60–62.
Sonnenberg A, Dellon ES, Dellon KO, Genta RM. The influence of Helicobacter pylori on the ethnic distribution of esophageal eosinophilia. Helicobacter. 2017;22:e12370.
Jensen ET, Martin CF, Kappelman MD, Dellon ES. Prevalence of eosinophilic gastritis, gastroenteritis, and colitis: estimates from a national administrative database. J Pediatr Gastroenterol Nutr. 2016;62:36–42.
Kia L, Hirano I. Distinguishing GERD from eosinophilic oesophagitis: concepts and controversies. Nat Rev Gastroenterol Hepatol. 2015;12:379–386.
Molina-Infante J, Bredenoord AJ, Cheng E et al. Proton pump inhibitor-responsive oesophageal eosinophilia: an entity challenging current diagnostic criteria for eosinophilic oesophagitis. Gut. 2016;65:524–531.
Molina-Infante J, Lucendo AJ. Proton pump inhibitor therapy for eosinophilic esophagitis: a paradigm shift. Am J Gastroenterol. 2017;112:1770–1773.
Dellon ES, Peterson KA, Murray JA et al. Anti-siglec-8 antibody for eosinophilic gastritis and duodenitis. N Engl J Med. 2020;383:1624–1634.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest in the publication of this article.
Disclosures
Ikuo Hirano has served as a consultant for Adare, Allakos, Arena, AstraZeneca, EsoCap, Gossamer, Receptos, Regeneron, and Shire Pharmaceuticals. He has received research funding from Adare, Allakos, Receptos, Regeneron, and Shire. Nirmala Gonsalves has served on the advisory board and as a co-investigator for Allakos Inc. She has received royalties from Up to Date.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10620_2021_7087_MOESM1_ESM.tif
Supplemental figure 1. Consort diagram of electronic medical record and pathology database search protocol used for patients included in the study (TIF 1850 KB)
Rights and permissions
About this article
Cite this article
Hiramoto, B., Zalewski, A., Gregory, D. et al. Low Prevalence of Extraesophageal Gastrointestinal Pathology in Patients with Eosinophilic Esophagitis. Dig Dis Sci 67, 3080–3088 (2022). https://doi.org/10.1007/s10620-021-07087-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07087-y