Abstract
Background/Aim
Patients with cirrhosis have poor outcomes once decompensation occurs; however, we lack adequate predictors of decompensation. To use a national claim database to compare the predictive accuracy of seven models for decompensation and hospitalization in patients with compensated cirrhosis.
Methods
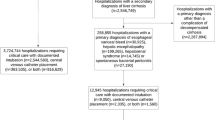
We defined decompensation as ascites, hepatic encephalopathy, hepato-renal syndrome, and variceal bleeding. Patients without decompensation at the time of cirrhosis diagnosis were enrolled from 2001 to 2015. Patients with hepatitis B and/or C were grouped as viral cirrhosis. We compared the predictive accuracy of models with the AUC (area under the curve) and c-statistic. The cumulative incidence of decompensation and incidence risk ratios of hospitalization were calculated with the Fine–Gray competing risk and negative binomial models, respectively.
Results
A total of 3722 unique patients were enrolled with a mean follow-up time of 524 days. The mean age was 59 (standard deviation 12), and the majority were male (55%) and white (65%). Fifty-three percent of patients had non-viral cirrhosis. Sixteen and 20 percent of patients with non-viral and viral cirrhosis, respectively, developed decompensation (P = 0.589). The FIB-4 model had the highest 3-year AUC (0.73) and overall c-statistic (0.692) in patients with non-viral cirrhosis. The ALBI-FIB-4 model had the best 1-year (AUC = 0.741), 3-year (AUC = 0.754), and overall predictive accuracy (c-statistic = 0.681) in patients with viral cirrhosis. The MELD score had the best predictive power for hospitalization in both non-viral and viral patients.
Conclusions
FIB-4-based models provide more accurate prediction for decompensation, and the MELD model has the best predictive ability of hospitalization.


Similar content being viewed by others
Abbreviations
- ALBI:
-
Albumin–bilirubin
- APRI:
-
Aspartate aminotransferase-to-platelet ratio index
- CI:
-
Confidence interval
- CTP:
-
Child–Turcotte–Pugh
- FIB-4:
-
Fibrosis-4
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- MELD:
-
Model for end-stage liver disease
References
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217–231.
D’Amico G, Morabito A, D’Amico M, et al. New concepts on the clinical course and stratification of compensated and decompensated cirrhosis. Hepatol Int.. 2018;12:34–43.
Tapper EB, Zhang P, Garg R, et al. Body composition predicts mortality and decompensation in compensated cirrhosis patients: A prospective cohort study. JHEP Rep.. 2020;2:100061.
Guha IN, Harris R, Berhane S, et al. Validation of a model for identification of patients with compensated cirrhosis at high risk of decompensation. Clin Gastroenterol Hepatol.. 2019;17:e1.
Hung TH, Hsieh MH, Lay CJ, et al. Increased occurrence of native septic arthritis in adult cirrhotic patients: a population-based three-year follow-up study in Taiwan. Prz Gastroenterol.. 2014;9:342–347.
Hung TH, Hsieh YH, Tseng KC, et al. The risk for bacterial endocarditis in cirrhotic patients: a population-based 3-year follow-up study. Int J Infect Dis.. 2013;17:e391.
Parikh NS, Kamel H, Navi BB, et al. Liver fibrosis indices and outcomes after primary intracerebral hemorrhage. Stroke. 2020:STROKEAHA119028161.
Mittal VS, Wu B, Song J, et al. Healthcare resource utilization and costs among nonvalvular atrial fibrillation patients initiating rivaroxaban or warfarin in skilled nursing facilities: a retrospective cohort study. Curr Med Res Opin.. 2019;20:1.
Allen AM, Therneau TM, Larson JJ, et al. Nonalcoholic fatty liver disease incidence and impact on metabotlic burden and death: a 20 year-community study. Hepatology.. 2018;67:1726–1736.
Austin PC, Fine JP. Practical recommendations for reporting Fine-Gray model analyses for competing risk data. Stat Med.. 2017;36:4391–4400.
Uno H, Cai T, Pencina MJ, et al. On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med.. 2011;30:1105–1117.
Planas R, Montoliu S, Ballesté B, et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin Gastroenterol Hepatol.. 2006;4:1385–1394.
D’Amico G, Pasta L, Morabito A, et al. Competing risks and prognostic stages of cirrhosis: a 25-year inception cohort study of 494 patients. Aliment Pharmacol Ther.. 2014;39:1180–1193.
Chen RC, Cai YJ, Wu JM, et al. Usefulness of albumin-bilirubin grade for evaluation of long-term prognosis for hepatitis B-related cirrhosis. J Viral Hepat.. 2017;24:238–245.
Angulo P, Bugianesi E, Bjornsson ES, et al. Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology.. 2013;145:e4.
Chen B, Lin S. Albumin-bilirubin (ALBI) score at admission predicts possible outcomes in patients with acute-on-chronic liver failure. Medicine (Baltimore).. 2017;96:e7142.
Wang J, Zhang Z, Yan X, et al. Albumin-Bilirubin (ALBI) as an accurate and simple prognostic score for chronic hepatitis B-related liver cirrhosis. Dig Liver Dis.. 2019;51:1172–1178.
Hsieh YC, Lee KC, Wang YW, et al. Correlation and prognostic accuracy between noninvasive liver fibrosis markers and portal pressure in cirrhosis: role of ALBI score. PLoS One.. 2018;13:e0208903.
Piano S, Romano A, Di Pascoli M, et al. Why and how to measure renal function in patients with liver disease. Liver Int.. 2017;37:116–122.
Piano S, Brocca A, Angeli P. Renal function in cirrhosis: a critical review of available tools. Semin Liver Dis.. 2018;38:230–241.
Fede G, D’Amico G, Arvaniti V, et al. Renal failure and cirrhosis: a systematic review of mortality and prognosis. J Hepatol.. 2012;56:810–818.
Smith BD, Morgan RL, Beckett GA, et al. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR Recomm Rep.. 2012;61:1–32.
Alberts M, Chen YW, Lin JH, et al. Risks of Stroke and Mortality in Atrial Fibrillation Patients Treated With Rivaroxaban and Warfarin. Stroke. 2019:STROKEAHA119025554.
Tapper EB, Hao S, Lin M, et al. The quality and outcomes of care provided to patients with cirrhosis by advanced practice providers. Hepatology.. 2019;71:225–234.
Funding
Elliot Tapper receives funding from the National Institutes of Health through the NIDDK (1K23DK117055-01A1).
Author information
Authors and Affiliations
Contributions
C-YH, NDP, and EBT performed the study design, biostatistics analysis, and manuscript preparation. T-IH participated in the biostatistics analysis. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Neehar Parikh serves as a consultant for Bristol Myers-Squibb, Exact Sciences, Eli Lilly, Freenome, has served on advisory boards of Genentech, Easai, Bayer, Exelexis, Wako/Fujifilm, and has received research funding from Bayer, Target Pharmasolutions, Exact Sciences, and Glycotest. Elliot Tapper has served as a consultant to Novartis, Kaleido, Axcella, and Allergan, has served on advisory boards for Mallinckrodt, Rebiotix, and Bausch Health, and has received unrestricted research grants from Gilead and Valeant. The remaining authors indicate no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hsu, CY., Parikh, N.D., Huo, TI. et al. Comparison of Seven Noninvasive Models for Predicting Decompensation and Hospitalization in Patients with Cirrhosis. Dig Dis Sci 66, 4508–4517 (2021). https://doi.org/10.1007/s10620-020-06763-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06763-9