Abstract
Background
Therapeutic drug monitoring (TDM) is important in optimizing use of biologics in inflammatory bowel diseases (IBD). However, the role of proactive TDM during remission remains uncertain.
Methods
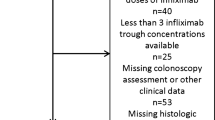
This retrospective study included patients receiving infliximab (IFX) therapy at Massachusetts General Hospital or Erasmus University Medical Center. All eligible patients had completed induction phase of IFX and were in clinical and endoscopic remission. Our primary outcome was clinical relapse within 2 years after baseline. Multivariable regression models examined the association between infliximab trough levels during remission and relapse, need for IBD-related surgery or hospitalization.
Results
Our study cohort included 110 patients with IBD (72 CD, 38 UC) on IFX maintenance therapy. In total, 12 patients (10.9%) experienced relapse of disease over 2 years. The mean IFX trough level at baseline was 8.0 µg/mL (± 8.6) and did not differ between the institutions. 49.1% of patients had levels < 5 µg/mL and 2.7% had antibodies to infliximab at baseline. There was no difference in the mean IFX trough levels between patients who relapsed (7.5 µg/mL ± 3.7 µg/mL) over 24 months compared to those who did not (8.1 µg/mL ± 7.9 µg/mL, p = 0.815). On multivariable logistic regression analysis, IFX trough levels at baseline were not associated with relapse of disease over 24 months (OR 1.01, 95% CI 0.93–1.09, p = 0.856).
Conclusion
This retrospective multicenter study provides evidence that IFX trough levels during quiescent disease do not predict relapse over 2 years, suggestive that proactive TDM in this setting is not warranted.


Similar content being viewed by others
References
Holko P, Kawalec P, Pilc A. Impact of biologic treatment of Crohn’s disease on the rate of surgeries and other healthcare resources: an analysis of a Nationwide Database From Poland. Front Pharmacol. 2018;9:621.
Kuenzig ME, Benchimol EI, Lee L, et al. The impact of inflammatory bowel disease in Canada 2018: direct costs and health services utilization. J Can Assoc Gastroenterol. 2019;2:S17–S33.
Feuerstein JD, Nguyen GC, Kupfer SS, et al. American gastroenterological association institute guideline on therapeutic drug monitoring in inflammatory bowel disease. Gastroenterology. 2017;153:827–834.
Steenholdt C, Brynskov J, Thomsen OO, et al. Individualised therapy is more cost-effective than dose intensification in patients with Crohn’s disease who lose response to anti-TNF treatment: a randomised, controlled trial. Gut. 2014;63:919–927.
Roblin X, Marotte H, Rinaudo M, et al. Association between pharmacokinetics of adalimumab and mucosal healing in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2014;12:80–84e2.
Yanai H, Lichtenstein L, Assa A, et al. Levels of drug and antidrug antibodies are associated with outcome of interventions after loss of response to infliximab or adalimumab. Clin Gastroenterol Hepatol. 2015;13:522–530e2.
Papamichael K, Chachu KA, Vajravelu RK, et al. Improved long-term outcomes of patients with inflammatory bowel disease receiving proactive compared with reactive monitoring of serum concentrations of infliximab. Clin Gastroenterol Hepatol. 2017;15:1580–1588e3.
Vande Casteele N, Ferrante M, Van Assche G, et al. Trough concentrations of infliximab guide dosing for patients with inflammatory bowel disease. Gastroenterology. 2015;148:1320–1329e3.
D’Haens G, Vermeire S, Lambrecht G, et al. Increasing infliximab dose based on symptoms, biomarkers, and serum drug concentrations does not increase clinical, endoscopic, and corticosteroid-free remission in patients with active luminal Crohn’s disease. Gastroenterology. 2018;154:1343–1351e1.
Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1:514.
Walmsley RS, Ayres RC, Pounder RE, et al. A simple clinical colitis activity index. Gut. 1998;43:29–32.
Willrich MA, Murray DL, Barnidge DR, et al. Quantitation of infliximab using clonotypic peptides and selective reaction monitoring by LC–MS/MS. Int Immunopharmacol. 2015;28:513–520.
Ungar B, Levy I, Yavne Y, et al. Optimizing anti-TNF-alpha therapy: serum levels of infliximab and adalimumab are associated with mucosal healing in patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2016;14:550–557e2.
Papamichael K, Rakowsky S, Rivera C, et al. Association between serum infliximab trough concentrations during maintenance therapy and biochemical, endoscopic, and histologic remission in Crohn’s disease. Inflamm Bowel Dis. 2018;24:2266–2271.
Papamichael K, Rakowsky S, Rivera C, et al. Infliximab trough concentrations during maintenance therapy are associated with endoscopic and histologic healing in ulcerative colitis. Aliment Pharmacol Ther. 2018;47:478–484.
Cornillie F, Hanauer SB, Diamond RH, et al. Postinduction serum infliximab trough level and decrease of C-reactive protein level are associated with durable sustained response to infliximab: a retrospective analysis of the ACCENT I trial. Gut. 2014;63:1721–1727.
Bortlik M, Duricova D, Malickova K, et al. Infliximab trough levels may predict sustained response to infliximab in patients with Crohn’s disease. J Crohns Colitis. 2013;7:736–743.
Adedokun OJ, Sandborn WJ, Feagan BG, et al. Association between serum concentration of infliximab and efficacy in adult patients with ulcerative colitis. Gastroenterology. 2014;147:1296–1307e5.
Assa A, Matar M, Turner D, et al. Proactive monitoring of adalimumab trough concentration associated with increased clinical remission in children with Crohn’s disease compared with reactive monitoring. Gastroenterology. 2019;157:985–996e2.
Gisbert JP, Panes J. Loss of response and requirement of infliximab dose intensification in Crohn’s disease: a review. Am J Gastroenterol. 2009;104:760–767.
Ben-Horin S, Chowers Y. Review article: loss of response to anti-TNF treatments in Crohn’s disease. Aliment Pharmacol Ther. 2011;33:987–995.
Hanauer SB, Feagan BG, Lichtenstein GR, et al. Maintenance infliximab for Crohn’s disease: the ACCENT I randomised trial. Lancet. 2002;359:1541–1549.
Acknowledgment
Dr. Ananthakrishnan has served on advisory boards for Abbvie, Takeda, and Merck. He is supported by research funding from the Crohn’s and Colitis Foundation, National Institutes of Health, Chleck Family Foundation, and Pfizer. Professor CJ van der Woude has served on advisory boards for Abbvie, Takeda, Pfizer, and Celltrion. She is supported by research funding from ZonMW, Tramedico, and Pfizer. Dr. Willrich reports intellectual property on the laboratory method to measure infliximab concentration (US patent #42580).
Funding
None.
Author information
Authors and Affiliations
Contributions
NZB and EP were involved in the study design, data acquisition, drafting of manuscript, and critical revision; JLF, RNO, MAW, and CJW contributed to the data acquisition and critical revision of manuscript; ANA was involved in the study design, data acquisition, critical revision of manuscript, and study supervision.
Corresponding author
Ethics declarations
Conflict of interest
There is no potential conflict of interest for this work for all authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Borren, N.Z., Paulides, E., Frinack, J.L. et al. Infliximab Trough Levels Are Not Predictive of Relapse in Patients with IBD in Endoscopic Remission: A Multicenter Cohort Study. Dig Dis Sci 66, 3548–3554 (2021). https://doi.org/10.1007/s10620-020-06645-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06645-0