Abstract
Background
Patients with chronic hepatitis C and risky/harmful alcohol use experience poor outcomes. Granular data evaluating whether alcohol counseling during hepatitis C treatment impacts longitudinal alcohol consumption are lacking.
Aims
To evaluate whether provider-delivered counseling in the context of direct-acting antiviral hepatitis C treatment associates with decreased longitudinal alcohol consumption.
Methods
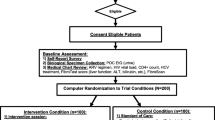
We performed secondary data analysis from the Hep ART study including adults with hepatitis C who underwent provider-delivered counseling during direct-acting antiviral treatment between October 2014 and September 2017. Demographics and disease characteristics were summarized. Alcohol consumption, abstinence, and heavy drinking were evaluated in periods before, during, and after direct-acting antiviral treatment. Multivariate regression analyses were performed to evaluate the association of alcohol consumption with each 12-week time period for all patients and a subsample with cirrhosis.
Results
One hundred twenty-three patients were included; 41 had cirrhosis. Most patients were male (74.0%) and Black (58.5%). Alcohol consumption improved during direct-acting antiviral treatment and was notably sustained (< 12 weeks before treatment 32.5 g/day; during treatment 20.0 g/day; and 12–24 weeks after treatment 23.7 g/day). Multivariable analyses showed significantly improved alcohol consumption metrics during and after antiviral treatment compared to < 12 weeks before treatment (during treatment 13.04 g/day less, p = 0.0001; > 24 weeks after treatment 15.29 g/day less, p = 0.0001). The subsample with cirrhosis showed similar results (during treatment 13.21 g/day less, p = 0.0001; > 24 weeks after treatment 7.69 g/day less, p = 0.0001).
Conclusions
Patients with chronic HCV and risky/harmful alcohol use given provider-delivered alcohol-related counseling during HCV treatment sustain decreased alcohol consumption patterns during and after treatment.




Similar content being viewed by others
References
Yang JD, Larson JJ, Watt KD, Allen AM, Wiesner RH, Gores GJ et al. Hepatocellular carcinoma is the most common indication for liver transplantation and placement on the waitlist in the United States. Clin Gastroenterol Hepatol. 2017;15:767–775.e3. https://doi.org/10.1016/j.cgh.2016.11.034.
Younossi ZM, Zheng L, Stepanova M, Venkatesan C, Mir HM. Moderate, excessive or heavy alcohol consumption: each is significantly associated with increased mortality in patients with chronic hepatitis C. Aliment Pharmacol Ther. 2013;37:703–709. https://doi.org/10.1111/apt.12265.
EASL Recommendations on Treatment of Hepatitis C 2018. J Hepatol. 2018;69:461–511. https://doi.org/10.1016/j.jhep.2018.03.026.
American Association for the Study of Liver Diseases. Recommendations for testing, managing, and treating hepatitis C [available at HCVguidelines.org]. 2019.
Taylor AL, Denniston MM, Klevens RM, McKnight-Eily LR, Jiles RB. Association of hepatitis C virus with alcohol use among US adults: NHANES 2003–2010. Am J Prevent Med. 2016;51:206–215. https://doi.org/10.1016/j.amepre.2016.02.033.
Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71:843–861. https://doi.org/10.1037/0022-006x.71.5.843.
Beich A, Thorsen T, Rollnick S. Screening in brief intervention trials targeting excessive drinkers in general practice: systematic review and meta-analysis. BMJ (Clin Res Ed). 2003;327:536–542. https://doi.org/10.1136/bmj.327.7414.536.
Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction (Abingdon). 1993;88:315–335. https://doi.org/10.1111/j.1360-0443.1993.tb00820.x.
Bernstein E, Topp D, Shaw E, Girard C, Pressman K, Woolcock E et al. A preliminary report of knowledge translation: lessons from taking screening and brief intervention techniques from the research setting into regional systems of care. Acad Emerg Med. 2009;16:1225–1233. https://doi.org/10.1111/j.1553-2712.2009.00516.x.
Owens MD, Ioannou GN, Tsui JL, Edelman EJ, Greene PA, Williams EC. Receipt of alcohol-related care among patients with HCV and unhealthy alcohol use. Drug Alcohol Depend. 2018;188:79–85. https://doi.org/10.1016/j.drugalcdep.2018.03.047.
Proeschold-Bell RJ, Evon DM, Yao J, Niedzwiecki D, Makarushka C, Keefe KA et al. A randomized controlled trial of an integrated alcohol reduction intervention in patients with hepatitis C infection. Hepatology (Baltimore) 2019. https://doi.org/10.1002/hep.31058.
Proeschold-Bell RJ, Patkar AA, Naggie S, Coward L, Mannelli P, Yao J et al. An integrated alcohol abuse and medical treatment model for patients with hepatitis C. Dig Dis Sci. 2012;57:1083–1091. https://doi.org/10.1007/s10620-011-1976-4.
Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165:986–995. https://doi.org/10.1001/archinte.165.9.986.
Sobell LC SM. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten RZ AJ, editor. Measuring alcohol consumption. The Humana Press; 1992. p. 41–72.
Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–706. https://doi.org/10.1093/aje/kwh090.
Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 2006;144:705–714. https://doi.org/10.7326/0003-4819-144-10-200605160-00004.
Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med. 2004;140:554–546. https://doi.org/10.7326/0003-4819-140-7-200404060-00016.
Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: measuring drinking outcomes in clinical trials. J Stud Alcohol. 2000;61:55–63. https://doi.org/10.15288/jsa.2000.61.55.
Acknowledgments
We are thankful to the study’s site PIs, Michael Fried and Susanna Naggie. We are also grateful to our study manager, Christina Makarushka, and interviewers, including Kelly Keefe, Becca Heine, Carla Mena, Courtenay Pierce, and Lavanya Vasudevan; our data managers including Ceci Chamorro and Donna Safley; our data entry team including Michael West, Blen Biru, Andy Elkins, Lauren Hunt, Caesar Lubangakene, and Nneka Molokwu; and Cathryn Mainville and Hayden Dawes who served as our Hep ART alcohol therapists.
Funding
This work was funded by the National Institutes of Health (Grant No. R01AA021133-01A1) and supported by the Duke University Center for AIDS Research (CFAR), an NIH-funded program (SP30 AI064518).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
Yuval A. Patel serves as a consultant for Intercept. Jia Yao has no conflicts of interest to report. Rae Jean Proeschold-Bell has no conflicts of interest to report. Donna Niedzwiecki has no conflicts of interest to report. Elizabeth Goacher has served as a speaker, a consultant, and an advisory board member for Gilead, AbbVie, Intercept, and Dova. Andrew J. Muir serves on advisory boards for AbbVie and Gilead.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patel, Y.A., Yao, J., Proeschold-Bell, R.J. et al. Reduced Alcohol Use Is Sustained in Patients Provided Alcohol-Related Counseling During Direct-Acting Antiviral Therapy for Hepatitis C. Dig Dis Sci 66, 2956–2963 (2021). https://doi.org/10.1007/s10620-020-06616-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06616-5