Abstract
Introduction
Pancreatic cancer is one of the most fatal malignancies and primary prevention strategies are limited. Epidemiological studies focusing on the association between folate intake and pancreatic cancer risk have reported inconsistent findings.
Methods
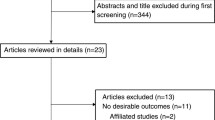
A systematic search of the literature was conducted using the PubMed and EMBASE databases. A systematic review and meta-analysis of eligible studies was performed to assess the association between folate intake and risk of pancreatic cancer.
Results
A total of 16 studies involving 5654 cases and 1,009,374 individuals were included. The result showed a significant association of folate intake with a decreased risk of pancreatic cancer, with a pooled OR of 0.82 (95% CI: 0.69–0.97, P = 0.019) for the highest category of intake vs. the lowest. The data suggested that high intake of folate may contribute to the prevention of pancreatic cancer. However, the association was observed only in case–control studies (OR = 0.78, 95% CI: 0.65–0.93, P = 0.006), but not in cohort studies (RR = 0.85, 95% CI: 0.66–1.09, P = 0.244). Dose–response meta-analysis showed that an increment of folate intake (100 μg/day) was marginally associated with the risk of pancreatic cancer, with a pooled OR of 0.97 (95% CI: 0.93–1.00, P = 0.053).
Conclusion
High folate intake might be inversely associated with pancreatic cancer risk, which needs to be confirmed.




Similar content being viewed by others
References
Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol. 2019;10:10–27.
Ilic M, Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol. 2016;22:9694–9705.
Afzal A, Suhong L, Gage BF, et al. Splanchnic vein thrombosis predicts worse survival in patients with advanced pancreatic cancer. Thromb Res. 2019;185:125–131.
Kirkegård J, Gaber C, Lund JL, et al. Acute pancreatitis as an early marker of pancreatic cancer and cancer stage, treatment, and prognosis. Cancer Epidemiol. 2019;64:101647.
Ikubo A, Matsufuji S, Morifuji Y, et al. Clinical features, prognosis, diagnostic approaches and treatment of multiple primary malignancies in the digestive system. Anticancer Res. 2019;39:6863–6870.
Ma Y, Pu Y, Peng L, et al. Identification of potential hub genes associated with the pathogenesis and prognosis of pancreatic duct adenocarcinoma using bioinformatics meta-analysis of multi-platform datasets. Oncol Lett. 2019;18:6741–6751.
Liu S, Qin Z, Xu J, et al. Irreversible electroporation combined with chemotherapy for unresectable pancreatic carcinoma: a prospective cohort study. Onco Targets Ther. 2019;12:1341–1350.
Mackay TM, van Erning FN, van der Geest LGM, et al. Association between primary origin (head, body and tail) of metastasised pancreatic ductal adenocarcinoma and oncologic outcome: a population-based analysis. Eur J Cancer. 2019;106:99–105.
Ben QW, Liu J, Sun YW, et al. Cigarette smoking and mortality in patients with pancreatic cancer: a systematic review and meta-analysis. Pancreas. 2019;48:985–995.
Koyanagi YN, Ito H, Matsuo K, et al. Smoking and pancreatic cancer incidence: a pooled analysis of 10 population-based cohort studies in Japan. Cancer Epidemiol Biomark Prev. 2019;28:1370–1378.
Pei-Ying Lu, Shu Long, Shen Shan-Shan, Chen Xu-Jiao, Zhang Xiao-Yan. Dietary patterns and pancreatic cancer risk: a meta-analysis. Nutrients. 2017;9:38.
Zheng Z, Zheng R, He Y, et al. Risk factors for pancreatic cancer in China: a multicenter case-control study. J Epidemiol. 2016;26:64–70.
Paternoster S, Falasca M. The intricate relationship between diabetes, obesity and pancreatic cancer. Biochim Biophys Acta Rev Cancer. 2019;1873:188326.
Zhou B, Wu D, Liu H, et al. Obesity and pancreatic cancer: an update of epidemiological evidence and molecular mechanisms. Pancreatology. 2019;19:941–950.
Tirkes T, Jeon CY, Li L, et al. Association of pancreatic steatosis with chronic pancreatitis, obesity, and type 2 diabetes mellitus. Pancreas. 2019;48:420–426.
Saluja A, Maitra A. Pancreatitis and pancreatic cancer. Gastroenterology. 2019;156:1937–1940.
Hart PA, Conwell DL. Chronic pancreatitis: managing a difficult disease. Am J Gastroenterol. 2019;00:1–7.
Wang YT, Gou YW, Jin WW, Xiao M, Fang HY. Association between alcohol intake and the risk of pancreatic cancer: a dose-response meta-analysis of cohort studies. BMC Cancer. 2016;16:212.
Underhill-Blazey M, Blonquist T, Lawrence J, Hong F, Yurgelun MB, Syngal S. Health behaviours and beliefs in individuals with familial pancreatic cancer. Fam Cancer. 2019;18:457–464.
Tsai HJ, Chang JS. Environmental risk factors of pancreatic cancer. J Clin Med. 2019;8:1427.
Risch HA, Lu L, Streicher SA, et al. Aspirin use and reduced risk of pancreatic cancer. Cancer Epidemiol Biomark Prev. 2017;26:68–74.
Karpiński TM. The microbiota and pancreatic cancer. Gastroenterol Clin North Am. 2019;48:447–464.
Maisonneuve P, Lowenfels AB. Risk factors for pancreatic cancer: a summary review of meta-analytical studies. Int J Epidemiol. 2015;44:186–198.
Zheng J, Wirth MD, Merchant AT, et al. Inflammatory potential of diet, inflammation-related lifestyle factors and risk of pancreatic cancer: results from the NIH-AARP Diet and Health Study. Cancer Epidemiol Biomark Prev. 2019;28:1266–1270.
Moukayed M, Grant WB. The roles of UVB and vitamin D in reducing risk of cancer incidence and mortality: a review of the epidemiology, clinical trials, and mechanisms. Rev Endocr Metab Disord. 2017;18:167–182.
Li D, Tang H, Wei P, Zheng J, Daniel CR, Hassan MM. Vitamin C andvitamin E mitigate the risk of pancreatic ductal adenocarcinoma from meat-derived mutagen exposure in adults in a case-control study. J Nutr. 2019;149:1443–1450.
Obón-Santacana M, Luján-Barroso L, Freisling H, et al. Consumption of nuts and seeds and pancreatic ductal adenocarcinoma risk in the European prospective investigation into cancer and nutrition. Int J Cancer. 2020;146:76–84.
Poirier AE, Ruan Y, Hebert LA, et al. Estimates of the current and future burden of cancer attributable to low fruit and vegetable consumption in Canada. Prev Med. 2019;122:20–30.
Koulouris AI, Luben R, Banim P, Hart AR. Dietary fiber and the risk of pancreatic cancer. Pancreas. 2019;48:121–125.
Asante I, Chui D, Pei H, et al. Alterations in folate-dependent one-carbon metabolism as colon cell transition from normal to cancerous. J Nutr Biochem. 2019;69:1–9.
Wu S, Zhang J, Li F, et al. One-carbon metabolism links nutrition intake to embryonic development via epigenetic mechanisms. Stem Cells Int. 2019;2019:3894101.
Gurwara S, Ajami NJ, Jang A, et al. Dietary nutrients involved in one-carbon metabolism and colonic mucosa-associated gut microbiome in individuals with an endoscopically normal colon. Nutrients. 2019;11:613.
Ducker GS, Rabinowitz JD. One-carbon metabolism in health and disease. Cell Metab. 2017;25:27–42.
Perrier F, Viallon V, Ambatipudi S, et al. Association of leukocyte DNA methylation changes with dietary folate and alcohol intake in the EPIC study. Clin Epigenetics. 2019;11:57.
Ben Fradj MK, Mrad Dali K, Kallel A, et al. Interaction effects of plasma vitamins A, E, D, B9, and B12 and tobacco exposure in urothelial bladder cancer: a multifactor dimensionality reduction analysis. Nutr Cancer. 2019;6:1–8.
Newman AC, Maddocks ODK. One-carbon metabolism in cancer. Br J Cancer. 2017;116:1499–1504.
Essén A, Santaolalla A, Garmo H, et al. Baseline serum folate, vitamin B12 and the risk of prostate and breast cancer using data from the Swedish AMORIS cohort. Cancer Causes Control. 2019;30:603–615.
Arthur RS, Kirsh VA, Rohan TE. Dietary B-vitamin intake and risk of breast, endometrial, ovarian and colorectal cancer among canadians. Nutr Cancer. 2019;7:1–11.
Liu W, Zhou H, Zhu Y, Tie C. Associations between dietary folate intake and risks of esophageal, gastric and pancreatic cancers: an overall and dose-response meta-analysis. Oncotarget. 2017;8:86828–86842.
Park JY, Bueno-de-Mesquita HB, Ferrari P, et al. Dietary folate intake and pancreatic cancer risk: results from the European prospective investigation into cancer and nutrition. Int J Cancer. 2019;144:1511–1521.
Marley AR, Fan H, Hoyt ML, Anderson KE, Zhang J. Intake of methyl-related nutrients and risk of pancreatic cancer in a population-based case-control study in Minnesota. Eur J Clin Nutr. 2018;72:1128–1135.
Yallew W, Bamlet WR, Oberg AL, et al. Association between alcohol consumption, folate intake, and risk of pancreatic cancer: a case-control study. Nutrients. 2017;9:48.
Huang JY, Butler LM, Wang R, Jin A, Koh WP, Yuan JM. Dietary intake of one-carbon metabolism-related nutrients and pancreatic cancer risk: the Singapore Chinese health study. Cancer Epidemiol Biomark Prev. 2016;25:417–424.
Tavani A, Malerba S, Pelucchi C, et al. Dietary folates and cancer risk in a network of case-control studies. Ann Oncol. 2012;23:2737–2742.
Chuang SC, Stolzenberg-Solomon R, Ueland PM, et al. A U-shaped relationship between plasma folate and pancreatic cancer risk in the European Prospective Investigation into Cancer and Nutrition. Eur J Cancer. 2011;47:1808–1816.
Bravi F, Polesel J, Bosetti C, et al. Dietary intake of selected micronutrients and the risk of pancreatic cancer: an Italian case-control study. Ann Oncol. 2011;22:202–206.
Oaks BM, Dodd KW, Meinhold CL, Jiao L, Church TR, Stolzenberg-Solomon RZ. Folate intake, post-folic acid grain fortification, and pancreatic cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Am J Clin Nutr. 2010;91:449–455.
Keszei AP, Verhage BA, Heinen MM, Goldbohm RA, van den Brandt PA. Dietary folate and folatevitamers and the risk of pancreatic cancer in the Netherlands cohort study. Cancer Epidemiol Biomark Prev. 2009;18:1785–1791.
Gong Z, Holly EA, Bracci PM. Intake of folate, vitamins B6, B12 and methionine and risk of pancreatic cancer in a large population-based case-control study. Cancer Causes Control. 2009;20:1317–1325.
Anderson LN, Cotterchio M, Gallinger S. Lifestyle, dietary, and medical history factors associated with pancreatic cancer risk in Ontario, Canada. Cancer Causes Control. 2009;20:825–834.
Schernhammer E, Wolpin B, Rifai N, et al. Plasma folate, vitamin B6, vitamin B12, and homocysteine and pancreatic cancer risk in four large cohorts. Cancer Res. 2007;67:5553–5560.
Larsson SC, Håkansson N, Giovannucci E, Wolk A. Folate intake and pancreatic cancer incidence: a prospective study of Swedish women and men. J Natl Cancer Inst. 2006;98:407–413.
Skinner HG, Michaud DS, Giovannucci EL, et al. A prospective study of folate intake and the risk of pancreatic cancer in men and women. Am J Epidemiol. 2004;160:248–258.
Stolzenberg-Solomon RZ, Pietinen P, Barrett MJ, Taylor PR, Virtamo J, Albanes D. Dietary and other methyl-group availability factors and pancreatic cancer risk in a cohort of male smokers. Am J Epidemiol. 2001;153:680–687.
Stolzenberg-Solomon RZ, Albanes D, Nieto FJ, et al. Pancreatic cancer risk and nutrition-related methyl-group availability indicators in male smokers. J Natl Cancer Inst. 1999;91:535–541.
Bao Y, Michaud DS, Spiegelman D, et al. Folate intake and risk of pancreatic cancer: pooled analysis of prospective cohort studies. J Natl Cancer Inst. 2011;103:1840–1850.
Lin HL, An QZ, Wang QZ, Liu CX. Folate intake and pancreatic cancer risk: an overall and dose-response meta-analysis. Public Health. 2013;127:607–613.
Ebara S. Nutritional role of folate. Congenit Anom (Kyoto). 2017;57:138–141.
Hogervorst E, Kassam S, Kridawati A, et al. Nutrition research in cognitive impairment/dementia, with a focus on soya and folate. Proc Nutr Soc. 2017;76:437–442.
Pieroth R, Paver S, Day S, Lammersfeld C. Folate and its impact on cancer risk. Curr Nutr Rep. 2018;7:70–84.
Fan C, Yu S, Zhang S, Ding X, Su J, Cheng Z. Association between folate intake and risk of head and neck squamous cell carcinoma: an overall and dose-response PRISMA meta-analysis. Med (Baltimore). 2017;96:e8182.
Selhub J, Rosenberg IH. Excessive folic acid intake and relation to adverse health outcome. Biochimie. 2016;126:71–78.
Liew SC. Folic acid and diseases—supplement it or not? Rev Assoc Med Bras. 1992;2016:90–100.
Joob B, Wiwanitkit V. Folate intake and risk of esophageal cancer. Eur J Cancer Prev. 2019;28:382.
Arthur RS, Kirsh VA, Rohan TE. Dietary B-vitamin intake and risk of breast, endometrial, ovarian and colorectal cancer among canadians. Nutr Cancer. 2019;71:1067–1077.
Du L, Wang Y, Zhang H, Zhang H, Gao Y. Folate intake and the risk of endometrial cancer: a meta-analysis. Oncotarget. 2016;7:85176–85184.
Dugué PA, Bassett JK, Brinkman MT, et al. Dietary intake of nutrients involved in one-carbon metabolism and risk of gastric cancer: a prospective study. Nutr Cancer. 2019;71:605–614.
Takata Y, Shu XO, Buchowski MS, et al. Food intake of folate, folic acid and other B vitamins with lung cancer risk in a low-income population in the Southeastern United States. Eur J Nutr. 2019;59:671–683.
Catala GN, Bestwick CS, Russell WR, et al. Folate, genomic stability and colon cancer: the use of single cell gel electrophoresis in assessing the impact of folate in vitro, in vivo and in human biomonitoring. Mutat Res. 2019;843:73–80.
Zgheib R, Battaglia-Hsu SF, Hergalant S, et al. Folate can promote the methionine-dependent reprogramming of glioblastoma cells towards pluripotency. Cell Death Dis. 2019;10:596.
Wang P, Chen Y, Wang L, et al. The intervention mechanism of folic acid for benzo(a)pyrene toxic effects in vitro and in vivo. Eur J Cancer Prev. 2019;28:355–364.
Rizzo A, Napoli A, Roggiani F, Tomassetti A, Bagnoli M, Mezzanzanica D. One-carbon metabolism: biological players in epithelial ovarian cancer. Int J Mol Sci. 2018;19:2092.
Min DJ, Vural S, Krushkal J. Association of transcriptional levels of folate-mediated one-carbon metabolism-related genes in cancer cell lines with drug treatment response. Cancer Genet. 2019;237:19–38.
Fenech M. Nutrition and genome health. Forum Nutr. 2007;60:49–65.
Wang HC, Huo YN, Lee WS. Folic acid prevents the progesterone-promoted proliferation and migration in breast cancer cell lines. Eur J Nutr. 2019.
Fernández M, Javaid F, Chudasama V. Advances in targeting the folate receptor in the treatment/imaging of cancers. Chem Sci. 2017;9:790–810.
Ting PC, Lee WR, Huo YN, Hsu SP, Lee WS. Folic acid inhibits colorectal cancer cell migration. J Nutr Biochem. 2019;63:157–164.
Zeng J, Wang K, Ye F, et al. Folate intake and the risk of breast cancer: an up-to-date meta-analysis of prospective studies. Eur J Clin Nutr. 2019;73:1657–1660.
Kim SJ, Zhang CXW, Demsky R, et al. Folic acid supplement use and breast cancer risk in BRCA1 and BRCA2 mutation carriers: a case-control study. Breast Cancer Res Treat. 2019;174:741–748.
Dhana A, Yen H, Li T, Holmes MD, Qureshi AA, Cho E. Intake of folate and other nutrients related to one-carbon metabolism and risk of cutaneous melanoma among US women and men. Cancer Epidemiol. 2018;55:176–183.
Kim HJ, Jung S, Eliassen AH, Chen WY, Willett WC, Cho E. Alcohol consumption and breast cancer risk in younger women according to family history of breast cancer and folate intake. Am J Epidemiol. 2017;186:524–531.
Seitz HK, Pelucchi C, Bagnardi V, La Vecchia C. Epidemiology and pathophysiology of alcohol and breast cancer: update 2012. Alcohol Alcohol. 2012;47:204–212.
Frydenberg H, Flote VG, Larsson IM, Barrett ES, Furberg AS, Ursin G. Alcohol consumption, endogenous estrogen and mammographic density among premenopausal women. Breast Cancer Res. 2015;17:103.
Stanisławska-Sachadyn A, Borzyszkowska J, Krzemiński M, et al. Folate/homocysteine metabolism and lung cancer risk among smokers. PLoS One. 2019;14:e0214462.
Sobczyńska-Malefora A, Harrington DJ. Laboratory assessment of folate (vitamin B9) status. J Clin Pathol. 2018;71:949–956.
Dixit R, Nettem S, Madan SS, et al. Folate supplementation in people with sickle cell disease. Cochrane Database Syst Rev. 2018;3:CD011130.
Zara-Lopes T, Galbiatti-Dias ALS, Castanhole-Nunes MMU, et al. Polymorphisms in MTHFR, MTR, RFC1 and CßS genes involved in folate metabolism and thyroid cancer: a case-control study. Arch Med Sci. 2019;15:522–530.
Gong JM, Shen Y, Shan WW, He YX. The association between MTHFR polymorphism and cervical cancer. Sci Rep. 2018;8:7244.
Román GC, Mancera-Páez O, Bernal C. Epigenetic factors in late-onset alzheimer’s disease: MTHFR and CTH gene polymorphisms, metabolic transsulfuration and methylation pathways, and B Vitamins. Int J Mol Sci. 2019;20:E319.
Acknowledgment
We thank Editage of Cactus Communications for the English language editing of the article.
Funding
This work was funded by Fundamental Research Funds for the Central Universities (XDJK2020D030).
Author information
Authors and Affiliations
Contributions
HC, HJF and JZ developed the study concept, designed the study, conducted the electronic searches and wrote the draft of the manuscript. HJF, CL, YG and YXZ conducted validity assessment, data extraction and provided critical review of the manuscript. HJF, JZ and CL tabulated data and conducted meta-analyses. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fu, H., Zeng, J., Liu, C. et al. Folate Intake and Risk of Pancreatic Cancer: A Systematic Review and Updated Meta-Analysis of Epidemiological Studies. Dig Dis Sci 66, 2368–2379 (2021). https://doi.org/10.1007/s10620-020-06525-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06525-7