Abstract
Background
Alcohol-related liver disease is one of the most prevalent chronic liver diseases worldwide. Mechanisms involved in the pathogenesis of alcohol-related liver disease are not well understood. Oxylipins play a crucial role in numerous biological processes and pathological conditions. Nevertheless, oxylipins are not well studied in alcohol-related liver disease.
Aims
(1) To characterize the patterns of bioactive ω-3 and ω-6 polyunsaturated fatty acid metabolites in alcohol use disorder and alcoholic hepatitis patients and (2) to identify associations of serum oxylipins with clinical parameters in patients with alcohol-related liver disease.
Methods
We performed a comprehensive liquid chromatography with tandem mass spectrometry (LC–MS/MS) analysis of serum and fecal oxylipins derived from ω-6 arachidonic acid, ω-3 eicosapentaenoic acid, and docosahexaenoic acid in a patient cohort with alcohol-related liver disease.
Results
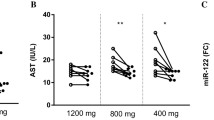
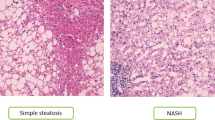
Our results show profound alterations in the serum oxylipin profile of patients with alcohol use disorder and alcoholic hepatitis compared to nonalcoholic controls. Spearman correlation of the oxylipins with clinical parameters shows a link between different serum oxylipins and intestinal permeability, aspartate aminotransferase, bilirubin, albumin, international normalized ratio, platelet count, steatosis, fibrosis and model for end-stage liver disease score. Especially, higher level of serum 20-HETE was significantly associated with decreased albumin, increased hepatic steatosis, polymorphonuclear infiltration, and 90-day mortality.
Conclusions
Patients with alcohol-related liver disease have different oxylipin profiles. Future studies are required to confirm oxylipins as disease biomarker or to connect oxylipins to disease pathogenesis.







Similar content being viewed by others
Abbreviations
- AP:
-
Alkaline phosphatase
- AST:
-
Aspartate aminotransferase
- ALT:
-
Alanine aminotransferase
- BMI:
-
Body mass index
- CAP:
-
Controlled attenuation parameter
- INR:
-
International normalized ratio
- MELD:
-
Model for end-stage liver disease
- MELDNa:
-
Sodium model for end-stage liver disease
- PMN:
-
Polymorphonuclear infiltration
- AA:
-
Arachidonic acid
- EPA:
-
Eicosapentaenoic acid
- DHA:
-
Docosahexaenoic acid
- HpETE:
-
Hydroperoxyeicosatetraenoic acid
- HETE:
-
Hydroxyeicosatetraenoic acid
- DiHETE:
-
Dihydroxyeicosatetraenoic acid
- PG:
-
Prostaglandin
- TX:
-
Thromboxane X
- EpETrE:
-
Epoxyeicosatrienoic acid
- DiHETrE:
-
Dihydroxyeicosatrienoic acid
- HpEPE:
-
Hydroperoxy-eicosapentaenoic acid
- HEPE:
-
Hydroxyeicosapentaenoic acid
- DiHEPE:
-
Dihydroxyeicosapentaenoic acid
- EpETE:
-
Epoxyeicosatetraenoic acid
- HpDoHE:
-
Hydroperoxydocosahexaenoic acid
- HDoHE:
-
Hydroxydocosahexaenoic acid
- DiHDoHE:
-
Dihydroxydocosahexaenoic acid
- DiHDPE:
-
Dihydroxydocosapentaenoic acid
- PLS-DA:
-
Partial least squares discriminant analysis
- VIP:
-
Variable importance in projection
- MRM:
-
Multiple reaction monitoring
References
Kwo PY, Cohen SM, Lim JK. ACG clinical guideline: evaluation of abnormal liver chemistries. Am J Gastroenterol. 2017;112:18.
Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology. 2011;141:1572–1585.
Gabbs M, Leng S, Devassy JG, Monirujjaman M, Aukema HM. Advances in our understanding of oxylipins derived from dietary PUFAs. Adv Nutr (Bethesda, Md.). 2015;6:513–540.
Buczynski MW, Dumlao DS, Dennis EA. Thematic review series: proteomics. An integrated omics analysis of eicosanoid biology. J Lipid Res. 2009;50:1015–1038.
Arnold C, Konkel A, Fischer R, Schunck W-H. Cytochrome P450–dependent metabolism of ω-6 and ω-3 long-chain polyunsaturated fatty acids. Pharmacol Rep. 2010;62:536–547.
Barquissau V, Ghandour RA, Ailhaud G, et al. Control of adipogenesis by oxylipins, GPCRs and PPARs. Biochimie. 2017;136:3–11.
Caligiuri SPB, Parikh M, Stamenkovic A, Pierce GN, Aukema HM. Dietary modulation of oxylipins in cardiovascular disease and aging. Am J Physiol Heart Circ Physiol. 2017;313:H903–H918.
Tourdot BE, Ahmed I, Holinstat M. The emerging role of oxylipins in thrombosis and diabetes. Front Pharmacol. 2014;4:176.
Funk CD. Prostaglandins and leukotrienes: advances in eicosanoid biology. Science. 2001;294:1871.
Yeung J, Hawley M, Holinstat M. The expansive role of oxylipins on platelet biology. J Mol Med (Berlin, Germany). 2017;95:575–588.
Wagner D, Westover K, Simmons DL. Nonsteroidal anti-inflammatory drugs, acetaminophen, cyclooxygenase 2, and fever. Clin Infect Dis. 2000;31:S211–S218.
Liu MC, Dubé LM, Lancaster J. Acute and chronic effects of a 5-lipoxygenase inhibitor in asthma: A 6-month randomized multicenter trial. J Allergy Clin Immunol. 1996;98:859–871.
Zhang W, Zhong W, Sun Q, Sun X, Zhou Z. Hepatic overproduction of 13-HODE due to ALOX15 upregulation contributes to alcohol-induced liver injury in mice. Sci Rep. 2017;7:8976.
Feldstein AE, Lopez R, Tamimi TA-R, et al. Mass spectrometric profiling of oxidized lipid products in human nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. J Lipid Res. 2010;51:3046–3054.
Ball SA, Tennen H, Poling JC, Kranzler HR, Rounsaville BJ. Personality, temperament, and character dimensions and the DSM-IV personality disorders in substance abusers. J Abnorm Psychol. 1997;106:545–553.
Brandl K, Hartmann P, Jih LJ, et al. Dysregulation of serum bile acids and FGF19 in alcoholic hepatitis. J Hepatol. 2018;69:396–405.
Nguyen-Khac E, Thiele M, Voican C, et al. Non-invasive diagnosis of liver fibrosis in patients with alcohol-related liver disease by transient elastography: an individual patient data meta-analysis. Lancet Gastroenterol Hepatol. 2018;3:614–625.
Salavrakos M, Piessevaux H, Komuta M, Lanthier N, Starkel P. Fibroscan reliably rules out advanced liver fibrosis and significant portal hypertension in alcoholic patients. J Clin Gastroenterol. 2018. https://doi.org/10.1097/MCG.0000000000001119.
Buzzetti E, Lombardi R, De Luca L, Tsochatzis EA. Noninvasive assessment of fibrosis in patients with nonalcoholic fatty liver disease. Int J Endocrinol. 2015;2015:343828.
Eddowes PJ, Sasso M, Allison M, et al. Accuracy of FibroScan controlled attenuation parameter and liver stiffness measurement in assessing steatosis and fibrosis in patients with non-alcoholic fatty liver disease. Gastroenterology. 2019;156:1717–1730.
Caussy C, Alquiraish MH, Nguyen P, et al. Optimal threshold of controlled attenuation parameter with MRI-PDFF as the gold standard for the detection of hepatic steatosis. Hepatology. 2018;67:1348–1359.
Karlas T, Petroff D, Sasso M, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022–1030.
Leclercq S, Matamoros S, Cani PD, et al. Intestinal permeability, gut-bacterial dysbiosis, and behavioral markers of alcohol-dependence severity. Proc Natl Acad Sci USA. 2014;111:E4485–E4493.
Shearer GC, Harris WS, Pedersen TL, Newman JW. Detection of omega-3 oxylipins in human plasma and response to treatment with omega-3 acid ethyl esters. J Lipid Res. 2010;51:2074–2081.
Luria A, Weldon SM, Kabcenell AK, et al. Compensatory mechanism for homeostatic blood pressure regulation in Ephx2 gene-disrupted mice. J Biol Chem. 2007;282:2891–2898.
Barupal DK, Fiehn O. Chemical similarity enrichment analysis (ChemRICH) as alternative to biochemical pathway mapping for metabolomic datasets. Sci Rep. 2017;7:14567.
Warner DR, Liu H, Ghosh Dastidar S, et al. Ethanol and unsaturated dietary fat induce unique patterns of hepatic ω-6 and ω-3 PUFA oxylipins in a mouse model of alcoholic liver disease. PloS One. 2018;13:e0204119.
Lazic M, Inzaugarat ME, Povero D, et al. Reduced dietary omega-6 to omega-3 fatty acid ratio and 12/15-lipoxygenase deficiency are protective against chronic high fat diet-induced steatohepatitis. PloS one. 2014;9:e107658.
Puri P, Xu J, Vihervaara T, et al. Alcohol produces distinct hepatic lipidome and eicosanoid signature in lean and obese. J Lipid Res. 2016;57:1017–1028.
Puri P, Wiest MM, Cheung O, et al. The plasma lipidomic signature of nonalcoholic steatohepatitis. Hepatology (Baltimore, Md.). 2009;50:1827–1838.
Zein CO, Lopez R, Fu X, et al. Pentoxifylline decreases oxidized lipid products in nonalcoholic steatohepatitis: new evidence on the potential therapeutic mechanism. Hepatology (Baltimore, Md.). 2012;56:1291–1299.
Kirpich IA, Feng W, Wang Y, et al. The type of dietary fat modulates intestinal tight junction integrity, gut permeability, and hepatic toll-like receptor expression in a mouse model of alcoholic liver disease. Alcohol Clin Exp Res. 2012;36:835–846.
Noverr MC, Erb-Downward JR, Huffnagle GB. Production of eicosanoids and other oxylipins by pathogenic eukaryotic microbes. Clin Microbiol Rev. 2003;16:517–533.
Tsitsigiannis DI, Keller NP. Oxylipins as developmental and host–fungal communication signals. Trends Microbiol. 2007;15:109–118.
Acknowledgments
This study was supported in part by NIH Grants R01 AA020703, R01 AA24726, U01 AA021856, U01 AA026939 and by Award Number BX004594 from the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development (to B.S.), and by Fond National de Recherche Scientifique (FNRS) Belgium grants CDR J.0146.17 and PDR T.0217.18 (to P.S.).
Author information
Authors and Affiliations
Contributions
B.G. was responsible for data acquisition, analysis, interpretation, and writing of the manuscript; S.L. was responsible for data analysis; Y.D. and Y.W. were responsible for preparation of human samples; D.L.S., A.L., P.M., S.B.H., and P.S. enrolled subjects for bio-specimen collection; and B.S. was responsible for the study concept and design, editing the manuscript, and study supervision.
Corresponding author
Ethics declarations
Conflict of interest
B.S. is consulting for Ferring Research Institute.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10620_2019_5638_MOESM1_ESM.jpg
Supplemental Figure S1 Venn diagram of significantly altered oxylipins found in both serum and fecal samples (adjusted p value < 0.05). Ctrl: controls; AUD: alcoholic use disorder; AH: alcoholic hepatitis (JPEG 165 kb)
10620_2019_5638_MOESM2_ESM.jpg
Supplemental Figure S2 Spearman correlation of fecal oxylipins with laboratory parameters in alcoholic hepatitis and alcohol use disorder patients. Color intensity represents the correlation coefficient (R). Red: positive correlation. Blue: negative correlation. * p < 0.05, ** p < 0.01, *** p < 0.001. INR, international normalized ratio; ALT, alanine aminotransferase; AST, aspartate aminotransferase; GGT, gamma-glutamyltransferase; AP, alkaline phosphatase (JPEG 267 kb)
10620_2019_5638_MOESM3_ESM.jpg
Supplemental Figure S3 Spearman correlation of fecal oxylipins with parameters of liver disease stage in alcohol use disorder patients (A). CAP: controlled attenuation parameter. Color intensity represents the correlation coefficient (R). Red: positive correlation. Blue: negative correlation. * p < 0.05. Number of alcohol use disorder patients N = 30. Spearman correlation of fecal oxylipins with liver histology and clinical scores in alcoholic hepatitis patients (B). Color intensity represents the correlation coefficient (R). Red: positive correlation. Blue: negative correlation. * p < 0.05, ** p < 0.01, *** p < 0.001. MELD, model for end-stage liver disease; MELDNa, sodium model for end-stage liver disease. Number of alcoholic hepatitis patients N = 7 (JPEG 486 kb)
Rights and permissions
About this article
Cite this article
Gao, B., Lang, S., Duan, Y. et al. Serum and Fecal Oxylipins in Patients with Alcohol-Related Liver Disease. Dig Dis Sci 64, 1878–1892 (2019). https://doi.org/10.1007/s10620-019-05638-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05638-y