Abstract
Background
There is currently an inadequate supply of allografts to meet the number of transplant candidates worldwide. A number of controversial policies, including implementation of a presumed consent organ donation system, have been considered to rectify the organ donation crisis.
Aims
A secondary retrospective data analysis aimed to assess the impact of switching to a presumed consent organ donation model on organ donation rates.
Methods
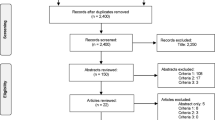
Deceased organ donation rates were compared before and after countries adopted presumed consent.
Results
Six countries met entry criteria. All six countries had an increase in liver donation rates, while 4 out of the six countries had an increase in kidney donation rates. The overall mean (± SD) liver donation rate was 3.23 (± 0.97) per million population (pmp) before the transition and 6.46 (± 1.81) pmp after the transition (p < 0.0001). The overall mean (± SD) kidney donation rate was 17.94 (± 3.34) pmp before the transition and 26.58 (± 4.23) pmp after the transition (p < 0.0001). The percentage increase in liver and kidney donation rates varied among countries, ranging from 28 to 1186%.
Conclusion
The transition from explicit to presumed consent was associated with a significant increase in liver donation rates in all countries that met our criteria, while the effect on kidney donation rates was partially realized. Although presumed consent alone is unlikely to explain the increase in donation rates, the adoption of such a policy may prove to be a worthwhile risk for countries experiencing consistently low organ donation rates.




Similar content being viewed by others
Abbreviations
- WHO:
-
World Health Organization
- GDP:
-
Gross domestic product
- ICU:
-
Intensive care unit
- R. Catholic:
-
Roman Catholic
- PMP:
-
Per million population
- Nd:
-
No date
- IRODaT:
-
International Registry in Organ Donation and Transplantation
- SD:
-
Standard deviation
- DCD:
-
Donation after cardiac death
- UAE:
-
United Arab Emirates
- OECD:
-
Organization for Economic Co-operation and Development
- IRB:
-
Institutional review board
- CIA:
-
Central Intelligence Agency
- UNDP:
-
United Nations Development Program
- n/a:
-
No value
- Slovak R:
-
Slovak Republic
- PMP:
-
Per million population
- M/F:
-
Male or female
- OPTN:
-
Organ Procurement and Transplantation Network
- GODT:
-
Global Observatory on Donation and Transplantation
References
Sheldon T. Dutch to start presumed consent for organ donation in 2020. BMJ. 2018;16:360.
Abouna GM. Organ shortage crisis: problems and possible solutions. Transplant Proc. 2008;40:34–38.
English V. Is presumed consent the answer to organ shortages? Yes. BMJ. 2007;26:334.
Merion RM, Schaubel DE, Dykstra DM, Freeman RB, Port FK, Wolfe RA. The survival benefit of liver transplantation. Am J Transplant. 2005;5:307.
Freeman RB, Wiesner RH, Edwards E, Harper A, Merion R, Wolfe R. Results of the first year of the new liver allocation plan. Liver Transplant. 2004;10:7.
Sharma P, Schaubel DE, Sima CS, Merion RM, Lok AS. Re-weighing the model for end stage liver disease score component. Gastroenterology. 2008;135:1575.
Merion RM, Sharma P, Mathur AK, Schaubel DE. Evidence-based development of liver allocation. Transpl Int. 2011;24:965.
Duffy JP, Kao K, Ko CY, et al. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010;252:652–661.
Saab S, Bownik H, Ayoub N, et al. Differences in health-related quality of life scores after orthotopic liver transplantation with respect to selected socioeconomic factors. Liver Transplant. 2011;17:580–590.
Crespo G, Trota N, Londoño MC, Mauro E, Baliellas C, Castells L, Castellote J, Tort J, Forns X, Navasa M. The efficacy of direct anti-HCV drugs improves early post-liver transplant survival and induces significant changes in wait-list composition. J Hepatol. 2018 in press.
Flemming JA, Kim WR, Brosgart CL, Terrault NA. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65:804–812.
Vagefi PA, Parekh J, Ascher NL, Roberts JP, Freise CE. Outcomes with split liver transplantation in 106 recipients: the University of California, San Francisco, experience from 1993 to 2010. Arch Surg. 2011;146:1052–1059.
Doyle MB, Maynard E, Lin Y, et al. Outcomes with split liver transplantation are equivalent to those with whole organ transplantation. J Am Coll Surg. 2013;217:102–112.
Aseni P, De Feo TM, De Carlis L, et al. A prospective policy development to increase split-liver transplantation for 2 adult recipients: results of a 12-year multicenter collaborative study. Ann Surg. 2014;259:157–165.
Muzaale AD, Dagher NN, Montgomery RA, Taranto SE, McBride MA, Segev DL. Estimates of early death, acute liver failure, and long-term mortality among live liver donors. Gastroenterology. 2012;142:273–280.
Sotiropoulos GC, Radtke A, Molmenti EP, et al. Long-term follow-up after right hepatectomy for adult living donation and attitudes toward the procedure. Ann Surg. 2011;254:694–700.
Kasahara M, Umeshita K, Inomata Y, Uemoto S. Long-term outcomes of pediatric living donor liver transplantation in Japan: an analysis of more than 2200 cases listed in the registry of the Japanese Liver Transplantation Society. Am J Transplant. 2013;13:1830–1839.
Hwang S, Lee SG, Lee YJ, et al. Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transplant. 2006;12:920–927.
Lew MA, et al. Long term medical and psychosocial outcomes in living liver donors. Am J Transplant. 2017;17:880.
Monbaliu D, Pirenne J, Talbot D. Liver transplantation using donation after cardiac death donors. J Hepatol. 2012;56:474.
Rithalia A, McDaid C, Suekarran S, Myers L, Sowden A. Impact of presumed consent for organ donation on donation rates: a systematic review. BMJ. 2009;338:a3162.
Davidai S, Gilovich T, Ross LD. The meaning of default options for potential organ donors. Proc Natl Acad Sci USA. 2012;109:15201–15205.
Johnson EJ, Goldstein D. Medicine. Do defaults save lives? Science. 2003;21:1338–1339.
Reibel M, Olmo C, Andrada S, Koertzen J. Deep demographics: understanding local variation in donor registration. Prog Transplant. 2016;26:191–198.
Wakefield CE, Watts KJ, Homewood J, Meiser B, Siminoff LA. Attitudes toward organ donation and donor behavior: a review of the international literature. Prog Transplant. 2010;20:380–391.
Regalia K, Zheng P, Sillau S, et al. Demographic factors affect willingness to register as an organ donor more than a personal relationship with a transplant candidate. Dig Dis Sci. 2014;59:1386–1391. https://doi.org/10.1007/s10620-014-3053-2.
Horvat LD, Cuerden MS, Kim SJ, Koval JJ, Young A, Garg AX. Informing the debate: rates of kidney transplantation in nations with presumed consent. Ann Intern Med. 2010;153:641–649.
Matesanz R. Factors influencing the adaptation of the Spanish model of organ donation. Transpl Int. 2003;16:736–741.
Gimbel RW, Strosberg MA, Lehrman SE, Gefenas E, Taft F. Presumed consent and other predictors of cadaveric organ donation in Europe. Prog Transplant. 2003;13:17–23.
World Health Organization guiding principles on human cell, tissue, and organ transplantation. 2008;1:1.
International Registry of Organ Donation and Transplantation. http://www.irodat.org/. Accessed March 25, 2018.
Law 26,066 Transfer of Organ and Tissues, Argentina. http://servicios.infoleg.gob.ar/infolegInternet/anexos/110000-114999/112375/norma.htm. Accessed February 20, 2018.
Rosenblum AM, Horvat LD, Siminoff LA, Prakash V, Beitel J, Garg AX. The authority of next-of-kin in explicit and presumed consent systems for deceased organ donation: an analysis of 54 nations. Nephrol Dial Transplant. 2012;27:2533–2546.
Hughes JA. Rethinking U.S. organ procurement policy. Vanderbilt J Transnatl Law. 2009;42:351–379.
Yordanova T. Ways to apply behavioral economics into organ donation and transplant system in Bulgaria. Manag Sustain Dev. 2014;45:52–58.
Lang MHK. The debate in Chile on organ donation revisited. Medwave. 2016;16:6525.
Willsher K. France introduces opt-out policy on organ donation. https://www.theguardian.com/society/2017/jan/02/france-organ-donation-law. Accessed February 20, 2018.
Symvoulakis EK, Markaki A, Galanakis C, Klinis S, Morgan M, Jones R. Shifting towards an opt-out system in Greece: a general practice based pilot study. Int J Med Sci. 2013;10:1547–1551.
Mihaly S, Smudla A, Kovacs J. Practices around communication about organ donation in Hungary. Transplant Proc. 2016;48:2529–2533.
Italy: provisions for organ harvesting and transplantation of organs and tissues, implementation of the requirements related to the declaration of citizens’ wishes on organ donation for transplantation purposes. http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=17738&articolo=3. Accessed February 20, 2018.
Wind J, Faut M, Van Smaalen TC, Van Heurn EL. Variability in protocols on donation after circulatory death in Europe. Crit Care. 2013;17:217.
Laurenco JS, Ciriolo E, Almeida SR, Troussard X. Behavioral insights applied to policy. Eur Rep. 2016;1:1–51.
Reilly K. Dutch bill would make everyone an organ donor unless they opt out. http://time.com/4490016/netherlands-organ-donation-bill/. Accessed February 20, 2018.
Norway Law No. 6 of 9 February 1973. http://www.lovdata.no/cgi-wift/wiftldles?doc¼/usr/www/lovdata/all/nl-19730209-006.html&emne¼transplantasjonslov*&&. Accessed April 2, 2018.
Rithalia A, McDaid C, Suekarran S, Norman G, Myers L. A systematic review of presumed consent systems for deceased organ donation. Health Technol Assess. 2009;13:1–95.
New Peru law permits removal of organs for transplant without kin’s consent. http://articles.latimes.com/1987-11-01/news/mn-17716_1_organ-removal. Accessed February 20, 2018.
The need for a soft opt-out plus approach to the proposed change in organ donor consent in Ireland. https://www.cfireland.ie/pdf/Joint_Submission_on_Organ_Donor_Consent.pdf. Accessed February 20, 2018.
Uruguay: modification of law 14.005 on organs and tissues. Global Observatory on Donation and Transplantation. http://www.transplant-observatory.org/download/ley-no-17-668-trasplantes-de-organos-y-tejidos-modificacion-de-la-ley-no-14-005-law-on-organs-and-tissues-2003-uruguay/. Accessed February 20, 2018.
Cruz PD. The Swedish law on transplantation. Comp Healthc Law. 2013;1:568.
Ministry of foreign affairs of Denmark. http://um.dk/en/. Accessed February 20, 2018.
Moy C. Improving Australia’s organ donation rates. https://ama.com.au/ausmed/improving-australia%E2%80%99s-organ-donation-rates. Accessed February 20, 2018.
Csillag C. Brazil abolishes presumed consent in organ donation. Lancet. 1998;352:1367.
Living donor liver transplantation: donor manual 2017. http://www.uhn.ca/MOT/Living_Donor_Program/Pages/living_liver_donor.aspx. Accessed February 20, 2017.
Reed GA. Organ donation and transplants in Cuba: promising results, challenges ahead. MEDICC Rev. 2016;18:11–14.
Li J, Nikolka T. The effect of presumed consent defaults on organ donation. CESifo DICE Report 2016; 4.
Organ donation in Hong Kong. Res Brief. 2016; 5:15–16.
Organ Donation - Introducing an opt-out system of consent, Ireland 2014. http://health.gov.ie/blog/policy/o/introducing-an-opt-out-system-of-consent-for-organ-donation/. Accessed February 20, 2018.
National organization for organ and tissue donation and transplantation Lebanese legislation historical overview. https://www.nodlb.org/en/support-my-decision/lebanese-legistlation/historical-overview. Accessed February 20, 2018.
Bagheri A. Organ transplantation laws in Asian countries: a comparative study. Transplant Proc. 2005;37:4159–4162.
Puerto Rico (government): Act No.296 Section 27. http://www.oslpr.org/download/en/2011/A-0026-2011.pdf. Accessed April 2, 2018.
Etheredge H, Penn C, Watermeyer J. Opt-in or opt-out to increase organ donation in South Africa? Appraising proposed strategies using an empirical ethics analysis. Dev World Bioethics. 2017;00:1–7.
Hsiao A. Most misinformed on organ donation: data. http://www.taipeitimes.com/News/taiwan/archives/2013/08/06/2003569051. Accessed February 20, 2018.
Organ procurement and transplantation network policies. https://optn.transplant.hrsa.gov/governance/policies/. Accessed February 20, 2018.
Need to improve the identification of potential organ donors. http://stm.fi/en/artikkeli/-/asset_publisher/need-to-improve-the-identification-of-potential-organ-donors. Accessed February 20, 2018.
Myerson B. Should families have the final say on organ donation? http://www.smh.com.au/federal-politics/the-question/should-families-have-the-final-say-on-organ-donation-20111209-1onde.html. Accessed February 20, 2018.
Venezuela enforces law on default organ donation. http://venezuela.um.dk/en/about-venezuela/news/newsdisplaypage/?newsid=dd59c17c-c27d-4bec-bc49-72b10c52d534. Accessed February 20, 2018.
Honduras: law for human organ and tissue donation and transplantation. http://www.transplant-observatory.org/download/ley-de-trasplante-y-extraccion-de-organos-y-tejidos-humanos-1982-law-for-human-organ-and-tissue-donation-and-transplantation-honduras/. Accessed February 20, 2018.
Dutch OK law: everyone is organ donor unless they opt out. Associated Press. http://www.businessinsider.com/ap-dutch-ok-law-everyone-is-organ-donor-unless-they-opt-out-2018-2. Accessed February 20, 2018.
Shepherd L, O’Carroll RE, Ferguson E. An international comparison of deceased and living organ donation/transplant rates in opt-in and opt-out systems: a panel study. BMC Med. 2014;12:131.
Bengali, Mostaghim. Kidney for sale’: Iran has a legal market for the organs, but the system doesn’t always work. http://www.latimes.com/world/middleeast/la-fg-iran-kidney-20171015-story.html. Accessed April 2, 2018.
Chamsi-Pasha H, Albar MA. Kidney transplantation: ethical challenges in the Arab world. Saudi J Kidney Dis Transplant. 2014;25:489–495.
Cacciatore R. Costa Rica organ trafficking trial links illicit transplant network to Ukraine. http://qcostarica.com/costa-rica-organ-trafficking-trial-links-illicit-transplant-network-to-ukraine/0/. Accessed April 2, 2018.
United Nations Office on Drugs and Crimes. Global Report on Trafficking in Persons. 2017.
Central intelligence agency world factbook. https://www.cia.gov/library/publications/the-world-factbook/fields/2103.html. Accessed February 20, 2018.
Baller S, Dutta S, Lanvin B. The global information technology report 2016. http://www3.weforum.org/docs/GITR2016/WEF_GITR_Full_Report.pdf. Accessed February 20, 2018.
Domínguez J, Rojas JL. Presumed consent legislation failed to improve organ donation in Chile. Transplant Proc. 2013;45:1316–1317.
Rodríguez-Arias D, Wright L, Paredes D. Success factors and ethical challenges of the Spanish Model of organ donation. Lancet. 2010;376:1109–1112.
Gavriluta C. Theoretical and practical premises in building up the health policies in the field of transplant. Transylvanian Review of Administrative Sciences 2013; S50.
Alexander JW, Vaughn WK. The use of marginal donors for organ transplantation. The influence of donor age on outcome. Transplantation. 1991;51:135–141.
Author information
Authors and Affiliations
Contributions
SS and SSS were involved in study concept and design, analysis and interpretation of data; SSS and MA contributed to acquisition of data; SS, SSS and MA were involved in drafting of the manuscript; SS and GC contributed to critical revision of the manuscript for important intellectual content; SSS contributed to statistical analysis; SS was involved in study supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Saab, S., Saggi, S.S., Akbar, M. et al. Presumed Consent: A Potential Tool for Countries Experiencing an Organ Donation Crisis. Dig Dis Sci 64, 1346–1355 (2019). https://doi.org/10.1007/s10620-018-5388-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5388-6