Abstract
Background
Microscopic colitis (MC), a subtype of inflammatory bowel disease, is a chronic condition of unknown etiology. Recent evidence has linked MC with intriguing changes in the stool microbiota, which may be linked to disease pathogenesis. The composition of the mucosal microbiome in patients with MC remains unclear.
Methods
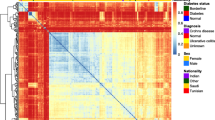
We performed a cross-sectional study comparing colonic tissue samples from patients with MC to those of healthy controls at the Michael E. DeBakey VA Medical Center. We included adults older than 18 who underwent a colonoscopy with biopsies to evaluate chronic diarrhea. Cases were defined by histology consistent with MC and controls by the absence of histologic disease. We conducted structured chart review to exclude other gastrointestinal diseases and obtain demographic (age, sex, race) and clinical (duration of symptoms and concurrent medications) information for cases and controls. We extracted bacterial DNA from formalin-fixed paraffin-embedded tissue samples and sequenced the v4 region of the 16S rRNA gene. Operational taxonomic unit (OTU) clustering was performed using UPARSE, and OTUs were assigned using the SILVA database. Statistical analysis was performed in QIIME and LEfSe. Comparisons with FDR-adjusted p values of less than 0.05 were considered statistically significant.
Results
We included 20 MC patients and 20 controls with mean ages of 62 and 54, respectively. Most cases were White (95%), 60% had symptoms for greater than 12 months, and 50% were taking PPIs and NSAIDs at the time of their diagnosis. Compared to controls, MC patients had a significant increase in the proinflammatory sulfur-reducing bacterial family Desulfovibrionales. The Coriobacteriaceae family, abundant in the healthy gut, was significantly decreased in MC cases. There was also an increase in the genus Actinomyces in MC patients on PPI and an increase in the class Bacilli among those taking NSAIDs.
Discussion
Patients with MC have an increase in the proinflammatory family Desulfovibrionales. Actinomyces and Bacilli were associated with medications (PPI and NSAID) known to increase the risk of MC. Our findings may have important implications for understanding the pathogenesis of MC.



Similar content being viewed by others
References
Tong J, Zheng Q, Zhang C, Lo R, Shen J, Ran Z. Incidence, prevalence, and temporal trends of microscopic colitis: a systematic review and meta-analysis. Am J Gastroenterol. 2015;110:265–276. (quiz 277).
Nyhlin N, Wickbom A, Montgomery SM, Tysk C, Bohr J. Long-term prognosis of clinical symptoms and health-related quality of life in microscopic colitis: a case-control study. Aliment Pharmacol Ther. 2014;39:963–972.
El-Salhy M, Gundersen D, Hatlebakk JG, Hausken T. Clinical presentation, diagnosis, pathogenesis and treatment options for lymphocytic colitis (Review). Int J Mol Med. 2013;32:263–270.
Fischer H, Holst E, Karlsson F, et al. Altered microbiota in microscopic colitis. Gut. 2015;64:1185–1186.
Rajilić-Stojanović M, Shanahan F, Guarner F, de Vos WM. Phylogenetic analysis of dysbiosis in ulcerative colitis during remission. Inflamm Bowel Dis. 2013;19:481–488.
Zoetendal EG, von Wright A, Vilpponen-Salmela T, Ben-Amor K, Akkermans AD, de Vos WM. Mucosa-associated bacteria in the human gastrointestinal tract are uniformly distributed along the colon and differ from the community recovered from feces. Appl Environ Microbiol. 2002;68:3401–3407.
Edgar RC. UPARSE: highly accurate OTU sequences from microbial amplicon reads. Nat Methods. 2013;10:996–998.
Cole JR, Wang Q, Fish JA, et al. Ribosomal Database Project: data and tools for high throughput rRNA analysis. Nucleic Acids Res. 2014;42:D633–D642.
Quast C, Pruesse E, Yilmaz P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41:D590–D596.
Caporaso JG, Kuczynski J, Stombaugh J, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7:335–336.
Segata N, Izard J, Waldron L, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60.
Rowan F, Docherty NG, Murphy M, Murphy B, Coffey JC, O‘Connell PR. Desulfovibrio bacterial species are increased in ulcerative colitis. Dis Colon Rectum. 2010;53:1530–1536.
Loubinoux J, Bronowicki JP, Pereira IA, Mougenel JL, Le Faou AE. Sulfate-reducing bacteria in human feces and their association with inflammatory bowel diseases. FEMS Microbiol Ecol. 2002;40:107–112.
Lennon G, Balfe A, Bambury N, et al. Correlations between colonic crypt mucin chemotype, inflammatory grade and Desulfovibrio species in ulcerative colitis. Colorectal Dis. 2014;16:O161–O169.
Png CW, Lindén SK, Gilshenan KS, et al. Mucolytic bacteria with increased prevalence in IBD mucosa augment in vitro utilization of mucin by other bacteria. Am J Gastroenterol. 2010;105:2420–2428.
Derrien M, Collado MC, Ben-Amor K, Salminen S, de Vos WM. The Mucin degrader Akkermansia muciniphila is an abundant resident of the human intestinal tract. Appl Environ Microbiol. 2008;74:1646–1648.
Kang CS, Ban M, Choi EJ, et al. Extracellular vesicles derived from gut microbiota, especially Akkermansia muciniphila, protect the progression of dextran sulfate sodium-induced colitis. PLoS ONE. 2013;8:e76520.
Reunanen J, Kainulainen V, Huuskonen L, et al. Akkermansia muciniphila adheres to enterocytes and strengthens the integrity of the epithelial cell layer. Appl Environ Microbiol. 2015;81:3655–3662.
Jackson MA, Goodrich JK, Maxan ME, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016;65:749–756.
Sokol H, Pigneur B, Watterlot L, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA. 2008;105:16731–16736.
Fujimoto T, Imaeda H, Takahashi K. Decreased abundance of Faecalibacterium prausnitzii in the gut microbiota of Crohn’s disease. J Gastroenterol Hepatol. 2013;28:613–619.
Human Microbiome Project, C. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–214.
Li G, Yang M, Zhou K, et al. Diversity of duodenal and rectal microbiota in biopsy tissues and luminal contents in healthy volunteers. J Microbiol Biotechnol. 2015;25:1136–1145.
Watt E, Gemmell MR, Berry S, et al. Extending colonic mucosal microbiome analysis-assessment of colonic lavage as a proxy for endoscopic colonic biopsies. Microbiome. 2016;4:61.
Tannock GW. The bowel microbiota and inflammatory bowel diseases. Int J Inflamm. 2010;2010:954051.
Huttenhower C, Kostic AD, Xavier RJ. Inflammatory bowel disease as a model for translating the microbiome. Immunity. 2014;40:843–854.
Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. 2014;146:1489–1499.
Berry D, Reinisch W. Intestinal microbiota: a source of novel biomarkers in inflammatory bowel diseases? Best Pract Res Clin Gastroenterol. 2013;27:47–58.
Funding
(1) The research reported here was supported in part by resources at the VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (#CIN 13-413), at the Michael E. DeBakey VA Medical Center, Houston, TX (JKH). (2) No writing assistance was used in the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
VM contributed in study design, data analysis, and authorship of the manuscript. She has approved of the final draft submission. DR contributed in study design, sample preparation, and authorship of the manuscript. He has approved of the final draft submission. JH contributed in authorship and editorial input. He has approved of the final draft submission. RS contributed in the study design, data abstraction, data analysis, and authorship of the manuscript. He has approved of the final draft submission.
Corresponding author
Ethics declarations
Conflict of interest
(1) JH has served as a speaker for AbbVie, Janssen, a consultant for UCB, and served on an advisory board for Pfizer. JH has received research funding from AbbVie, Janssen, Pfizer, Celgene, and RedHill Biopharma. (2) VM, DR, and RS have no financial disclosures.
Additional information
The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Millien, V., Rosen, D., Hou, J. et al. Proinflammatory Sulfur-Reducing Bacteria Are More Abundant in Colonic Biopsies of Patients with Microscopic Colitis Compared to Healthy Controls. Dig Dis Sci 64, 432–438 (2019). https://doi.org/10.1007/s10620-018-5313-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5313-z