Abstract
Background
Most studies assessing the influence of a low fermentable oligo-, di-, monosaccharides and polyols (FODMAP) diet on irritable bowel syndrome (IBS) symptoms were clinical trials with a small sample size.
Objective
This study was done to examine the association between adherence to a low FODMAP diet and symptoms of irritable bowel syndrome in Iranian adults.
Methods
In this cross-sectional study, data on 3362 Iranian adults were collected. Dietary intakes of study participants were assessed using a validated 106-item self-administered dish-based, semi-quantitative food frequency questionnaire. Based on earlier studies, we identified all foods with a high FODMAP content in our dataset. Participants were categorized into quartiles in terms of dietary intakes of these foods. Total FODMAP score for each individual was computed by summing up the scores of all foods. Individuals in the highest quintile of FODMAP score were defined as those with the greatest adherence to the low FODMAP diet. A modified Persian version of the ROME III questionnaire was used for assessment of IBS, which was defined according to ROME III criteria.
Results
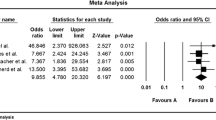
Adherence to the low FODMAP diet was significantly associated with low intakes of macro- and micro-nutrients as well as all food groups (P < 0.001 for all). Participants with the greatest adherence to the low FODMAP diet, compared to those with the lowest adherence, had not significantly lower odds for having IBS, either before (95% CI 0.93, 1.58, P < 0.05) or after adjustment for potential confounders (95% CI 0.80, 1.60, P < 0.05). This was also the case for IBS subtypes; such that those with the greatest adherence to the low FODMAP diet, compared to those with the lowest adherence, were not less likely to have these types of IBS.
Conclusion
In conclusion, we did not find any significant association between adherence to the low FODMAP diet and IBS. Further studies are required to reach a definite conclusion in this regard.
Similar content being viewed by others
Abbreviations
- FODMAP:
-
Fermentable oligo-, di-, monosaccharides and polyols
- GI:
-
Gastrointestinal
- LFD:
-
Low FODMAP diet
- HFD:
-
High FODMAP diet
- TACD:
-
Typical American childhood diet
- IBS:
-
Irritable bowel syndrome
- IBS-D:
-
IBS with diarrhea predominant
- IBS-C:
-
IBS with constipation predominant
References
Corazziari E. Definition and epidemiology of functional gastrointestinal disorders. Best Pract Res Clin Gastroenterol. 2004;18:613–631.
Nanayakkara WS, Skidmore PM, O’Brien L, Wilkinson TJ, Gearry RB. Efficacy of the low FODMAP diet for treating irritable bowel syndrome: the evidence to date. Clin Exp Gastroenterol. 2016;9:131.
Hungin A, Chang L, Locke G, Dennis E, Barghout V. Irritable bowel syndrome in the United States: prevalence, symptom patterns and impact. Aliment Pharmacol Ther. 2005;21:1365–1375.
Khademolhosseini F, Mehrabani D, Nejabat M, et al. Irritable bowel syndrome in adults over 35 years in Shiraz, southern Iran: prevalence and associated factors. J Res Med Sci. 2011;16:200.
Dean BB, Aguilar D, Barghout V, et al. Impairment in work productivity and health-related quality of life in patients with IBS. Am J Manag Care. 2005;11:S17–S26.
El-Serag HB. Impact of irritable bowel syndrome: prevalence and effect on health-related quality of life. Rev Gastroenterol Disord. 2002;3:S3–S11.
El-Serag H, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16:1171–1185.
Longstreth GF, Bolus R, Naliboff B, et al. Impact of irritable bowel syndrome on patients’ lives: development and psychometric documentation of a disease-specific measure for use in clinical trials. Eur J Gastroenterol Hepatol. 2005;17:411–420.
Hulisz D. The burden of illness of irritable bowel syndrome: current challenges and hope for the future. J Manag Care Pharm. 2004;10:299–309.
Roest Rd, Dobbs B, Chapman B, et al. The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study. Int J Clin Pract. 2013;67:895–903.
Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146:67–75.e5.
Böhn L, Störsrud S, Liljebo T, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial. Gastroenterology. 2015;149:1399–1407.e2.
Pedersen N, Andersen NN, Végh Z, et al. Ehealth: low FODMAP diet vs Lactobacillus rhamnosus GG in irritable bowel syndrome. World J Gastroenterol. 2014;20:16215.
Chumpitazi BP, Cope JL, Hollister EB, et al. Randomised clinical trial: gut microbiome biomarkers are associated with clinical response to a low FODMAP diet in children with the irritable bowel syndrome. Aliment Pharmacol Ther. 2015;42:418–427.
Ong DK, Mitchell SB, Barrett JS, et al. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010;25:1366–1373.
Adibi P, Keshteli AH, Esmaillzadeh A, et al. The study on the epidemiology of psychological, alimentary health and nutrition (SEPAHAN): overview of methodology. J Res Med Sci. 2012;17:S291–S297.
Willett W. Nutritional epidemiology. Oxford: Oxford University Press; 2012.
Keshteli AH, Esmaillzadeh A, Rajaie S, Askari G, Feinle-Bisset C, Adibi P. A dish-based semi-quantitative food frequency questionnaire for assessment of dietary intakes in epidemiologic studies in Iran: design and development. Int J Prev Med. 2014;5:29.
Staudacher H, Whelan K, Irving P, Lomer M. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011;24:487–495.
y López NP, Torres-Lopez E, Zamarripa-Dorsey F. Clinical response in Mexican patients with irritable bowel syndrome treated with a low diet low in fermentable carbohydrates (FODMAP). Rev Gastroenterol Mex. 2015;80:180–185.
Staudacher HM, Lomer MC, Anderson JL, et al. Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 2012;142:1510–1518.
Barrett JS, Gearry RB, Muir JG, et al. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther. 2010;31:874–882.
Undseth R, Berstad A, Kløw NE, Arnljot K, Moi K, Valeur J. Abnormal accumulation of intestinal fluid following ingestion of an unabsorbable carbohydrate in patients with irritable bowel syndrome: an MRI study. Neurogastroenterol Motil. 2014;26:1686–1693.
Acknowledgments
We wish to thank all staff of Isfahan University of Medical Sciences, who kindly participated in our study and staffs of Public Relations Unit, and other authorities of IUMS for their excellent cooperation. The present study was supported by a grant from National Institute for Medical Research Development (NIMAD), Islamic Republic of Iran. The Grant Number is 963261. The authors would like to thank all participants and their parents.
Author information
Authors and Affiliations
Contributions
HP and AE conducted the study, carried out the statistical analyses, wrote the manuscript and contributed in the interpretation of the findings. AHK, PS, HD and PA contributed to the conception, design and data collection. AE supervised the study. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors had any personal or financial conflicts of interest.
Rights and permissions
About this article
Cite this article
Pourmand, H., Keshteli, A.H., Saneei, P. et al. Adherence to a Low FODMAP Diet in Relation to Symptoms of Irritable Bowel Syndrome in Iranian Adults. Dig Dis Sci 63, 1261–1269 (2018). https://doi.org/10.1007/s10620-018-4986-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-4986-7