Abstract
Background and Aims
Angioectasias (AVMs) are the most common vascular anomaly of the gastrointestinal (GI) tract, and these lesions are often associated with obscure gastrointestinal bleeding (OGIB). It is unknown if the presence of upper and/or lower gastrointestinal AVMs are predictive of small bowel AVMs. The aims of this study are to define the small bowel segmental distribution of AVMs and to identify the factors predicting the presence of small bowel AVMs among a cohort of patients with a known history of AVMs in the upper and/or lower GI tracts who are undergoing capsule endoscopy (CE) for OGIB.
Methods
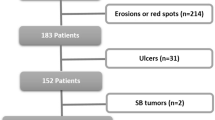
We performed a retrospective cohort analysis of 1,125 patients undergoing CE at our institution between 11/1/2001 and 8/31/2007. Inclusion criteria were: (1) complete esophagoduodenoscopy (EGD), CE, and colonoscopy, (2) OGIB indication for CE, and (3) history of ≥1 AVM on EGD and/or colonoscopy that was previously treated in the past or deemed not to be a clinically significant source of bleeding. Exclusion criteria were: (1) history of radiation therapy to the GI tract, and (2) presence of a congenital or systemic disease associated with GI AVMs. Data were extracted on: (1) age; (2) gender; (3) presence of diabetes, (4) presence of hypertension, (5) presence of aortic stenosis, (6) history of non-steroidal anti-inflammatory therapy, (7) history of anticoagulant therapy, (8) hemoglobin, platelet, and INR values prior to CE; (9) baseline serum creatinine; and (10) presence and GI tract segmental location of AVMs. Multivariate logistic regression was used to identify independent predictors of small bowel AVMs.
Results
1,125 patients underwent EGD, CE, and colonoscopy. One hundred and fourteen patients had a history of ≥1 AVM on EGD and/or colonoscopy and met inclusion and exclusion criteria. The mean age was 69 years, and 63% of patients were women. 37% of patients were found to have ≥1 jejunal AVM and 15% were found to have ≥1 ileal AVM. In multivariate analysis, age ≥ 65 (OR 2.62, P = 0.05) and the presence of AVMs on EGD (OR 4.61, P = 0.02) were predictive of jejunal AVMs. AVMs on colonoscopy alone were not predictive of jejunal or ileal AVMs. No factors were found to predict the presence of ileal AVMs.
Conclusions
Patients with AVMs on EGD have an increased risk of jejunal AVMs on CE, particularly if they are elderly. Future studies should validate these findings in a prospective cohort.

Similar content being viewed by others
Abbreviations
- AGA:
-
American gastroenterological association
- AVM:
-
Angioectasia
- CE:
-
Capsule endoscopy
- DBE:
-
Double-balloon enteroscopy
- EGD:
-
Esophagoduodenoscopy
- GI:
-
Gastrointestinal
- vWF:
-
von Willebrand’s factor
References
Boley SJDA, Brandt LJ, Sammartano RJ. Lower intestinal bleeding in the elderly. Am J Surg. 1979;137:57–64.
Rogers BH. Endoscopic diagnosis and therapy of mucosal vascular abnormalities of the gastrointestinal tract occurring in elderly patients and associated with cardiac, vascular, and pulmonary disease. Gastrointest Endosc. 1980;26:134–138.
Baum S, Athanasoulis CA, Waltman AC. Angiodysplasia of the right colon: a cause of gastrointestinal bleeding. AJR Am J Roentgenol. 1977;129:789–794.
Raju GS, Gerson L, Das A, Lewis B. American gastroenterological association (AGA) institute technical review on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1697–1717.
Saurin JC, Delvaux M, Gaudin JL, et al. Diagnostic value of endoscopic capsule in patients with obscure digestive bleeding: Blinded comparison with video push-enteroscopy. Endoscopy. 2003;35:576–584.
Porush J, Faubert PF. Chronic renal failure in renal disease in the aged. Boston: Little, Brown; 1991:285.
Zuckerman GR, Cornette GL, Clouse RE, Harter HR. Upper gastrointestinal bleeding in patients with chronic renal failure. Ann Intern Med. 1985;102:588–592.
Duray PH, Marcal JM Jr, LiVolsi VA, Fisher R, Scholhamer C, Brand MH. Small intestinal angiodysplasia in the elderly. J Clin Gastroenterol. 1984;6:311–319.
Alhumood SA, Devine DV, Lawson L, Nantel SH, Carter CJ. Idiopathic immune-mediated acquired von Willebrand’s disease in a patient with angiodysplasia: Demonstration of an unusual inhibitor causing a functional defect and rapid clearance of von Willebrand factor. Am J Hematol. 1999;60:151–157.
Veyradier A, Balian A, Wolf M, et al. Abnormal von Willebrand factor in bleeding angiodysplasias of the digestive tract. Gastroenterology. 2001;120:346–353.
Vincentelli A, Susen S, Le Tourneau T, et al. Acquired von Willebrand syndrome in aortic stenosis. N Engl J Med. 2003;349:343–349.
Warkentin TE, Moore JC, Anand SS, Lonn EM, Morgan DG. Gastrointestinal bleeding, angiodysplasia, cardiovascular disease, and acquired von Willebrand syndrome. Transfus Med Rev. 2003;17:272–286.
Warkentin TE, Moore JC, Morgan DG. Aortic stenosis and bleeding gastrointestinal angiodysplasia: Is acquired von Willebrand’s disease the link? Lancet. 1992;340:35–37.
Pareti FI, Lattuada A, Bressi C, et al. Proteolysis of von Willebrand factor and shear stress-induced platelet aggregation in patients with aortic valve stenosis. Circulation. 2000;102:1290–1295.
O’Brien JR, Etherington MD, Brant J, Watkins J. Decreased platelet function in aortic valve stenosis: High shear platelet activation then inactivation. Br Heart J. 1995;74:641–644.
Cappell MS. Spatial clustering of simultaneous nonhereditary gastrointestinal angiodysplasia. Small but significant correlation between nonhereditary colonic and upper gastrointestinal angiodysplasia. Dig Dis Sci. 1992;37:1072–1077.
Clouse RE, Costigan DJ, Mills BA, Zuckerman GR. Angiodysplasia as a cause of upper gastrointestinal bleeding. Arch Intern Med. 1985;145:458–461.
Moreto M, Figa M, Ojembarrena E, Zaballa M. Vascular malformations of the stomach and duodenum: An endoscopic classification. Endoscopy. 1986;18:227–229.
Rockey DC, Cello JP. Evaluation of the gastrointestinal tract in patients with iron-deficiency anemia. N Engl J Med. 1993;329:1691–1695.
Gostout CJ, Bowyer BA, Ahlquist DA, Viggiano TR, Balm RK. Mucosal vascular malformations of the gastrointestinal tract: Clinical observations and results of endoscopic neodymium: Yttrium-aluminum-garnet laser therapy. Mayo Clin Proc. 1988;63:993–1003.
Apostolopoulos P, Liatsos C, Gralnek IM, et al. The role of wireless capsule endoscopy in investigating unexplained iron deficiency anemia after negative endoscopic evaluation of the upper and lower gastrointestinal tract. Endoscopy. 2006;38:1127–1132.
Foutch PG. Angiodysplasia of the gastrointestinal tract. Am J Gastroenterol. 1993;88:807–818.
ASGE Standards of Practice Committee, Fisher L, Lee Krinsky M, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Cash BD, Decker GA, Fanelli RD, Friis C, Fukami N, Harrison ME, Ikenberry SO, Jain R, Jue T, Khan K, Maple JT, Strohmeyer L, Sharaf R, Dominitz JA. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010;72:471–479.
Hanauer DA. EMERSE: The electronic medical record search engine. AMIA Annu Symp Proc. 2006;941.
Giustini D. How google is changing medicine. BMJ. 2005;331:1487–1488.
Bonow RO, Carabello BA, Chatterjee K, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: A report of the American college of cardiology/American heart association task force on practice guidelines (writing committee to revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the society of cardiovascular anesthesiologists endorsed by the society for cardiovascular angiography and interventions and the society of thoracic surgeons. J Am Coll Cardiol. 2006;48:e1–e148.
Ortiz V, Ortuño J, Rodríguez-Soler M, et al. Outcome of non-variceal acute upper gastrointestinal bleeding in patients with antithrombotic therapy. Digestion. 2009;80:89–94. Epub 2009 Jun 19.
Saperas E, Videla S, Dot J, et al. Risk factors for recurrence of acute gastrointestinal bleeding from angiodysplasia. Eur J Gastroenterol Hepatol. 2009;21:1333–1339.
Raju GS, Gerson L, Das A, Lewis B. American gastroenterological association (AGA) institute medical position statement on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1694–1696.
Raju GS, Gerson L, Das A, Lewis B. American gastroenterological association (AGA) institute technical review on obscure gastrointestinal bleeding. Gastroenterology. 2007;133:1697–1717.
Triester SL, Leighton JA, Leontiadis GI, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK. A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2005;100:2407–2418.
Hartmann D, Schmidt H, Bolz G, et al. A prospective two-center study comparing wireless capsule endoscopy with intraoperative enteroscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2005;61:826–832.
Pennazio M, Eisen G, Goldfarb N. ICCE consensus for obscure gastrointestinal bleeding. Endoscopy. 2005;37:1046–1050.
Pasha S, Leighton J, Das A, et al. DBE and CE have comparable diagnostic yield in SB disease; a meta-analysis. Clin Gastroenterol Hepatol. 2008;6:671–676.
Kamal AGL. Cost-benefit analysis of double balloon enteroscopy compared to other diagnostic modalities for obscure gastrointestinal hemorrhage. Gastrointest Endosc. 2006;63:AB90.
Acknowledgments
We would like to thank Brian Burtraw, Mark McDermott, and Jason Baker (University of Michigan Health System Gastrointestinal Physiology Laboratory Technicians) for their assistance in the management of our CE data.
Conflict of interest
The authors declare no conflicts of interests associated with the creation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DeBenedet, A.T., Saini, S.D., Takami, M. et al. Do Clinical Characteristics Predict the Presence of Small Bowel Angioectasias on Capsule Endoscopy?. Dig Dis Sci 56, 1776–1781 (2011). https://doi.org/10.1007/s10620-010-1506-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1506-9