Abstract
Background
Air insufflation is essential in routine colonoscopy, but obtaining optimal insufflation levels has not been discussed in the literature. The aim of this study was to determine optimal air insufflation during colonoscopic examination.
Methods
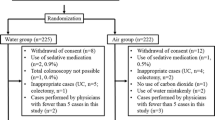
Consecutive patients who underwent colonoscopy were randomized to receive high-air insufflation (group A, n = 83), low-air insufflation (group B, n = 84), or low-air insufflation limited to the rectum and sigmoid colon (group C, n = 83). Completion rate, cecal intubation time, propofol dose, need for abdominal compression, and turning of patients, were evaluated. The post-procedure abdominal bloating was assessed with a 0–10 visual analog scale.
Results
The completion rates were similar among the three groups. The cecal intubation time was significantly shorter in group C than in group B (4.1 ± 1.7 min vs. 5.2 ± 3.0 min, mean ± SD, p = 0.005). The dose of propofol was significantly less in group C than in group A (11.7 ± 3.2 mg vs. 12.7 ± 3.6 mg, mean ± SD, p = 0.045). Group C needed the least manual abdominal compression (group A, B, and C: 81.9, 69, and 59%, respectively, p = 0.005) and had the least post-procedure abdominal bloating (group A, B, and C: 2.2 ± 2.4, 2.2 ± 2.1, and 1.5 ± 1.9, respectively, p = 0.04).
Conclusions
We found that limited use of low-air insufflation in the rectum and sigmoid is the procedure of choice for colonoscopic examination.

Similar content being viewed by others
References
Rex DK, Rahmani EY, Haseman JH, et al. Relative sensitivity of colonoscopy and barium enema for detection of colorectal cancer in clinical practice. Gastroenterology. 1997;112:17–23.
Lindsay DC, Freeman JG, Cobden I, et al. Should colonoscopy be the first investigation for colonic disease? Br Med J (Clin Res Ed). 1988;296:167–169.
Waye JD, Bashkoff E. Total colonoscopy: Is it always possible? Gastrointest Endosc. 1991;37:152–154.
Brooker JC, Saunders BP, Shah SG, et al. A new variable stiffness colonoscope makes colonoscopy easier: a randomised controlled trial. Gut. 2000;46:801–805.
Shah SG, Brooker JC, Williams CB, et al. Effect of magnetic endoscope imaging on colonoscopy performance: a randomised controlled trial. Lancet. 2000;356:1718–1722.
Cheung HY, Chung CC, Kwok SY, et al. Improvement in colonoscopy performance with adjunctive magnetic endoscope imaging: a randomized controlled trial. Endoscopy. 2006;38:214–217.
Brocchi E, Pezzilli R, Tomassetti P, et al. Warm water or oil-assisted colonoscopy: toward simpler examinations? Am J Gastroenterol. 2008;103:581–587.
Cotton PB, Williams CB (1996) Practical Gastrointestinal Endoscopy. Blackwell Science, p 224.
Brandt LJ, Boley SJ, Sammartano R. Carbon dioxide and room air insufflation of the colon. Effects on colonic blood flow and intraluminal pressure in the dog. Gastrointest Endosc. 1986;32:324–329.
Church JM. Warm water irrigation for dealing with spasm during colonoscopy: simple, inexpensive, and effective. Gastrointest Endosc. 2002;56:672–674.
Leung JW, Mann S, Leung FW. Options for screening colonoscopy without sedation: a pilot study in United States veterans. Aliment Pharmacol Ther. 2007;26:627–631.
Woltjen JA. A retrospective analysis of cecal barotrauma caused by colonoscope air flow and pressure. Gastrointest Endosc. 2005;61:37–45.
Bretthauer M, Hoff GS, Thiis-Evensen E, et al. Air and carbon dioxide volumes insufflated during colonoscopy. Gastrointest Endosc. 2003;58:203–206.
Shah SG, Brooker JC, Thapar C, et al. Patient pain during colonoscopy: an analysis using real-time magnetic endoscope imaging. Endoscopy. 2002;34:435–440.
Shah SG, Saunders BP, Brooker JC, et al. Magnetic imaging of colonoscopy: an audit of looping, accuracy and ancillary maneuvers. Gastrointest Endosc. 2000;52:1–8.
Stevenson GW, Wilson JA, Wilkinson J, et al. Pain following colonoscopy: elimination with carbon dioxide. Gastrointest Endosc. 1992;38:564–567.
Lee JG, Vigil H, Leung JW. A randomized controlled trial of total colonic decompression after colonoscopy to improve patient comfort. Am J Gastroenterol. 2001;96:95–100.
Sumanac K, Zealley I, Fox BM, et al. Minimizing postcolonoscopy abdominal pain by using CO(2) insufflation: a prospective, randomized, double blind, controlled trial evaluating a new commercially available CO(2) delivery system. Gastrointest Endosc. 2002;56:190–194.
Steinberg EN, Howden CW. Randomized controlled trial of rectal tube placement for the management of abdominal distension following colonoscopy. Gastrointest Endosc. 1997;46:444–446.
Rex DK. Colonoscopic withdrawal technique is associated with adenoma miss rates. Gastrointest Endosc. 2000;51:33–36.
Rex DK. Maximizing detection of adenomas and cancers during colonoscopy. Am J Gastroenterol. 2006;101:2866–2877.
Leung JW, Salera R, Toomsen L et al. (2008) Pilot feasibility study of the method of water infusion without air insufflation in sedated colonoscopy. Dig Dis Sci.
Hamamoto N, Nakanishi Y, Morimoto N, et al. A new water instillation method for colonoscopy without sedation as performed by endoscopists-in-training. Gastrointest Endosc. 2002;56:825–828.
Baumann UA. Water intubation of the sigmoid colon: Water instillation speeds up left-sided colonoscopy. Endoscopy. 1999;31:314–317.
Bernstein C, Thorn M, Monsees K, et al. A prospective study of factors that determine cecal intubation time at colonoscopy. Gastrointest Endosc. 2005;61:72–75.
Yoshikawa I, Honda H, Nagata K, et al. Variable stiffness colonoscopes are associated with less pain during colonoscopy in unsedated patients. Am J Gastroenterol. 2002;97:3052–3055.
Waye JD, Bashkoff E. Total colonoscopy: is it always possible? Gastrointest Endosc. 1991;37:152–154.
Saunders BP, Fukumoto M, Halligan S, et al. Why is colonoscopy more difficult in women? Gastrointest Endosc. 1996;43:124–126.
Anderson JC, Gonzalez JD, Messina CR, et al. Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol. 2000;95:2784–2787.
Robinson FP, Dundee JW, Halliday NJ. Age affects the induction dose of propofol (‘Diprivan’). Postgrad Med J. 1985;61(Suppl 3):157–159.
Hilton P, Dev VJ, Major E. Intravenous anaesthesia with propofol and alfentanil. The influence of age and weight. Anaesthesia. 1986;41:640–643.
Acknowledgments
This study was supported by research funds from Buddhist Dalin Tzu Chi General Hospital.
Conflict of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hsieh, YH., Tseng, KC. & Lin, HJ. Limited Low-Air Insufflation Is Optimal for Colonoscopy. Dig Dis Sci 55, 2035–2042 (2010). https://doi.org/10.1007/s10620-010-1210-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1210-9