Abstract
Background and Aims
The location of mucosal damage and changes in mucin content in the rat small intestine following administration of non-steroidal anti-inflammatory drugs (NSAIDs) have not been well elucidated.
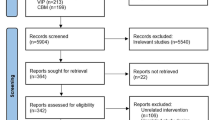
Methods
After subcutaneous administration of loxoprofen sodium (10–40 mg/kg), the small intestinal mucosa of male Wistar rats was evaluated macroscopically, histologically, and immunohistochemically by measuring the total mucin content and immunoreactivity for anti-mucin monoclonal antibody, HCM31, 1, 3, 7, and 14 days later. Changes in the number of enterobacteria invading the mucosa around the lesions were also determined.
Results
Loxoprofen sodium induced erosions and ulcers along the mesenteric margin of the distal jejunum. Early (≤6 h) mucosal lesions were small and round, located between the branches of the mesenteric arteries. In the jejunum, there was a transient increase in the total mucin content, and HCM31-positive mucin in the mucosa around the ulcers increased significantly on days 3 and 7, but in the ileum there were no marked changes and few ulcers. Bacterial translocation following loxoprofen sodium administration significantly increased, according to the site of the intestinal lesions.
Conclusions
Vascularly compromised sites along the jejunal mesenteric margin are vulnerable to NSAIDs-induced damage and show increased numbers of enterobacteria in the NSAIDs-treated mucosa. Increased sialomucin content in the mucus around the lesions may play an important role in the healing of NSAIDs-induced intestinal lesions.







Similar content being viewed by others
References
Anthony A, Pounder RE, Dhillon AP, Wakefield AJ. Vascular anatomy defines sites of indomethacin induced jejunal ulceration along the mesenteric margin. Gut. 1997;41:763–770.
Iwai T, Ichikawa T, Goso Y, et al. Effects of indomethacin on the rat small intestinal mucosa: immunohistochemical and biochemical studies using antimucin monoclonal antibodies. J Gastroenterol. 2009;44:277–284.
Takeuchi K, Miyazawa T, Tanaka A, Kato S, Kunikata T. Pathogenic importance of intestinal hypermotility in NSAIDs-induced small intestinal damage in rats. Digestion. 2002;66:30–41.
Evans SM, Whittle BJ. Role of bacteria and inducible nitric oxide synthase activity in the systemic inflammatory microvascular response provoked by indomethacin in the rat. Eur J Pharmacol. 2003;461:63–71.
Hagiwara M, Kataoka K, Arimochi H, Kuwahara T, Ohnishi Y. Role of unbalanced growth of gram-negative bacteria in ileal ulcer formation in rats treated with a nonsteroidal anti-inflammatory drug. J Med Invest. 2004;51:43–51.
Reuter BK, Davies NM, Wallace JL. Nonsteroidal anti-inflammatory drug enteropathy in rats: role of permeability, bacteria, and enterohepatic circulation. Gastroenterology. 1997;112:109–117.
Misaka E, Yamaguchi T, Iizuka Y, et al. Anti-inflammatory, analgesic and antipyretic activities of sodium 2-(4-(2-oxocycyclopentan-1-ylmethyl) phenyl) propionate dehydrate (CS-600). Pharmacometrics. 1981;21:753–771 (Abstract).
Suzuki G, Ooishi M, Kato T, et al. Multiple ileal ulcers and an ileal dieulafoy’s lesion induced by loxoprofen sodium. Dig Endosc. 2003;15:243–246.
Allen A, Flemstrom G. Gastroduodenal mucus bicarbonate barrier: protection against acid and pepsin. Am J Physiol Cell Physiol. 2005;288:C1–C19.
Azuumi Y, Ohara S, Ishihara K, Okabe H, Hotta K. Correlation of quantitative changes of gastric mucosal glycoproteins with aspirin-induced gastric damage in rats. Gut. 1980;21:533–536.
Ichikawa T, Ota H, Sugiyama A, et al. Effects of a novel histamine H2-receptor antagonist, lafutidine, on the mucus barrier of human gastric mucosa. J Gastroenterol Hepatol. 2007;22:1800–1805.
Bentley MD, Ortiz MC, Ritman EL, Romero JC. The use of microcomputed tomography to study microvasculature in small rodents. Am J Physiol Regul Integr Comp Physiol. 2002;282:R1267–R1279.
Ota H, Katsuyama T. Alternating laminated array of two types of mucin in the human gastric surface mucous layer. Histochem J. 1992;24:86–92.
Ishihara K, Kurihara M, Goso Y, Ota H, Katsuyama T, Hotta K. Establishment of monoclonal antibodies against carbohydrate moiety of gastric mucins distributed in the different sites and layers of rat gastric mucosa. Glycoconj J. 1996;13:857–864.
Kojima T, Iizuka Y. Favorable feature of loxoprofen sodium, a prodrug, for the irritating effect on gastric mucosa in rats. Jpn Pharmacol Ther. 1988;16:611–619. (In Japanese with English abstract).
Matsuzawa T, Saito H, Kurihara A, Ninomiya S, Uohama K, Ebine H. Absorption, distribution, metabolism and excretion after dermal application of hyrdogel patch containing loxoprofen sodium in rats. J Clini Ther Med. 2006;22:187–203. (In Japanese with English abstract).
Shimizu K, Koga H, Iida M, Haruma K. Microcirculatory changes in experimental mesenteric longitudinal ulcers of the small intestine in rats. Dig Dis Sci. 2007;52:3019–3028.
Kelly DA, Piasecki C, Anthony A, Dhillon AP, Pounder RE, Wakefield AJ. Focal reduction of villous blood flow in early indomethacin enteropathy: a dynamic vascular study in the rat. Gut. 1998;42:366–373.
Hatazawa R, Ohno R, Tanigami M, Tanaka A, Takeuchi K. Roles of endogenous prostaglandins and cyclooxygenase isozymes in healing of indomethacin-induced small intestinal lesions in rats. J Pharmacol Exp Ther. 2006;318:691–699.
Azuumi Y, Ishihara K, Ohara S, Okabe H, Hotta K. Efficacy of anti-ulcer drugs on the recovery of gastric mucosal glycoproteins with aspirin-induced gastric damage in rat. Gastroenterol Jpn. 1981;16:331–334.
Kojima Y, Ishihara K, Ohara S, Saigenji K, Hotta K. Effects of the M1 muscarinic receptor antagonist pirenzepine on gastric mucus glycoprotein in rats with or without ethanol-induced gastric damage. Scand J Gastroenterol. 1992;27:764–768.
Yusuf S, Nok AJ, Ameh DA, Adelaiye AB, Balogun EO. Correlation of gastric mucosal damage with sialic acid profile in rats: effect of hydrochloric acid, pepsin and hypertonic saline. Cell Biochem Funct. 2005;23:339–345.
Watanabe T, Higuchi K, Kobata A, et al. Non-steroidal anti-inflammatory drug-induced small intestinal damage is Toll-like receptor 4 dependent. Gut. 2008;57:181–187.
Kinouchi T, Kataoka K, Bing SR, et al. Culture supernatants of Lactobacillus acidophilus and Bifidobacterium adolescentis repress ileal ulcer formation in rats treated with a nonsteroidal antiinflammatory drug by suppressing unbalanced growth of aerobic bacteria and lipid peroxidation. Microbiol Immunol. 1998;42:347–355.
Onderdonk AB, Richardson JA, Hammer RE, Taurog JD. Correlation of cecal microflora of HLA-B27 transgenic rats with inflammatory bowel disease. Infect Immun. 1998;66:6022–6023.
Yokota A, Ohno R, Takahira Y, Tanaka A, Takeuchi K. Protective effect of teprenone against indomethacin-induced small intestinal lesion in rats. Jpn Pharmacol Ther. 2005;33:51–61.
Mizoguchi H, Ogawa Y, Kanatsu K, Tanaka A, Kato S, Takeuchi K. Protective effect of rebamipide on indomethacin-induced intestinal damage in rats. J Gastroenterol Hepatol. 2001;16:1112–1119 (Abstract).
Niwa Y, Nakamura M, Ohmiya N, et al. Efficacy of rebamipide for diclofenac-induced small-intestinal mucosal injuries in healthy subjects: a prospective, randomized, double-blinded, placebo-controlled, cross-over study. J Gastroenterol. 2008;43:270–276.
Atuma C, Strugala V, Allen A, Holm L. The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver Physiol. 2001;280:G922–G929.
Acknowledgments
We would like to express our sincere thanks to S. Sugawara, M. Hashimura, and Y. Numata for their technical assistance. This work was supported in part by grants from the Shin-Caterpillar Mitsubishi Co., and the Integrative Research Project of the Graduate School of Medical Sciences, Kitasato University. The authors report no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iwai, T., Ichikawa, T., Kida, M. et al. Vulnerable Sites and Changes in Mucin in the Rat Small Intestine After Non-steroidal Anti-inflammatory Drugs Administration. Dig Dis Sci 55, 3369–3376 (2010). https://doi.org/10.1007/s10620-010-1185-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-010-1185-6