Abstract
Background
CBASP is a learning acquisition model of psychotherapy and until this present study, has not been systematically dismantled to identify the active ingredient.
Methods
The present investigation is the first formal dismantling pilot-study conducted to date on the Cognitive Behavioral Analysis System of Psychotherapy (CBASP). The two major treatment components of CBASP, Situational Analysis (SA) and the Interpersonal Discrimination Exercise (IDE), were administered alone and with CBASP treatment-as-usual (the combination of both) to determine if there were active ingredients operative in the model. Secondly, we questioned if the dismantling of CBASP should continue in a larger study in an effort to answer the greater dismantling question of whether to administer both SA and IDE separately based on the active ingredient outcomes.
Results
The study did achieve visually inspected differential data patterns across the three groups of the dependent measures. Based on these outcomes, a larger dismantling study seems warranted and is recommended.
Conclusions
We strongly urge that a larger dismantling study using a similar design be conducted in an effort to further the dismantling process of the CBASP model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The present pilot study denotes the first step of a component analysis project (Kazdin, 2007; Kazdin & Nock, 2003) that ultimately (over-time) may result in the identification of the mechanisms of change involved in the evidenced-based treatment, Cognitive Behavioral Analysis System of Psychotherapy (CBASP) (McCullough, 2000, 2006, 2015). CBASP is designed specifically to treat adult Persistent Depressive Disorder (PDD) (Furukawa et al., 2016; Hom et al., 2017; Keller et al., 2000; Negt et al., 2016; Schramm et al., 2017).
This pilot study represents a first-step to dismantle the CBASP model and identify its active ingredients. The study will attempt to investigate if CBASP, which usually administers concomitantly its two major component-techniques [Situational Analysis (SA) and the Interpersonal Discrimination Exercise (IDE)], produces visually-inspected differential data under controlled dismantling conditions (Ahn & Wampold, 2001; Beck et al., 1979; Bell et al., 2013; Jacobson et al., 1996; Papa & Follette, 2014). The SA pinpoints the problem areas and teaches adaptive problem-solving coping skills to counter the maladaptive patterns. The IDE focuses on the quality of the dyadic relationship discriminating the dyadic relationship from toxic significant other relationships that have hurt the patient. Under normal conditions, SA is administered in approximately 70% of the sessions while the IDE is administered in 30% of the sessions, respectively.
In order to achieve the first step toward our ultimate goal of identifying the mechanism(s) of change in CBASP, we will rely on the methodological formulations of Rounsaville et al. (2001) who proposed a two-stage program of research to address fledgling research questions. Thus, we begin our pilot dismantling project with a Rounsaville et al. Stage Ib design. Most of Rounsaville et al.’s requisite Stage Ib steps (2001, p. 135) for a research proposal have been met in previous CBASP Research (e.g., Keller et al., 2000, etc.). For example, the CBASP model is theoretically grounded, its treatment components are fully operationalized, the training criteria for therapists are in place, the training manuals for therapists and patients have been successfully used numerous times, and the inclusion and exclusion criteria for targeted patient-subjects (i.e. DSM-5, Persistent Depressive Disorder) (American Psychiatric Association: APA, 2013) have been thoroughly delineated.
However, despite CBASP having achieved some success to date, a basic issue remains and that is, determining the model’s mechanisms of change. The following query expresses the basic issue: what are the active ingredients (mechanisms of change) in CBASP given its two major treatment components, Situational Analysis (SA) and the Interpersonal Discrimination Exercise (IDE)? In this study, we will investigate individually and in combination, the two major treatment components of CBASP - that is, SA and the IDE. Contingent on our findings, we hope to continue this dismantling research project with a larger Stage II clinical trial (Rounsaville et al., 2001) that may provide more substantive answers to our query about component mechanisms.
Since no data are available that might contribute to our basic dismantling question (McCullough et al., 2015; Penberthy, 2019), no hypotheses will be proposed.
The Two Major CBASP Treatment Components. As noted above, CBASP is a psychotherapy model consisting of two major treatment components: a 5-step problem-solving algorithm labeled Situational Analysis (SA) and a 4-step dyadic interpersonal strategy labeled the Interpersonal Discrimination Exercise (IDE) (McCullough, 2000, 2006; McCullough et al., 2010).
Method
Participants
Six outpatients who met criteria for DSM-5 (APA, 2013) early-onset Persistent Depressive Disorder (PDD) criteria were recruited from local universities and other outpatient mental health organizations. The chronological age of the sample ranged from 20 to 45 with a mean age of 33.5 (SD = 9.7). The reported age of onset for the six participants ranged from 6 to 15 years of age with an onset mean age of 12 (SD = 3.2).
A total of 12 patients were screened, and five failed to meet the inclusion criteria. One patient dropped out of treatment after eight sessions due to an unexpected relocation. A new patient, who met criteria for the study, replaced the patient who dropped out. Due to the patient who dropped out being prior to the session minimum (which was a minimum of 10 sessions), none of the dropout patient data were included in the study. The replacement patient was administered 20 sessions of therapy. Criteria for inclusion in the final data analysis required that one remains for a “minimum” of 10 treatment sessions. Summarily, seven participants (including the patient who dropped from the study) were selected through the screening process, and all provided written informed consent to participate. However, only six patients completed the study due to the patient described above being excluded. The study was approved by the Liberty University Institutional Review Board.
Inclusion Criteria
To be eligible for the study, patients must have been between the ages of 18–55 years, met the early-onset criteria for PDD and obtained a score of ≥ 18 on the 17-item Structured Interview for the Guide the Hamilton Rating Scale (SIGH-D: Williams, 2001, 2013) and a score of ≥ 19 on the Beck Depression Inventory-II (BDI-II; Beck, 1996). Participants had to be English-speaking, have a high school education and obtain an IQ score of ≥ 85. Individuals taking selective serotonin reuptake inhibitors (SSRI), serotonin and norepinephrine reuptake inhibitors (SNRI), and anti-anxiety meds were eligible for participation. Three participants (one participant in each cell) remained on medication throughout the study under the care of their psychiatrist and no changes in medication doses occurred.
The only personality disorder inclusions included two categories from the DSM-5 (APA, 2013) Cluster C Personality Disorders: Histrionic and Dependent Personality disorders. No participant met the criteria for a Personality Disorder. Six participants who met the inclusion criteria were randomly assigned to one of three treatment cells. No participant had a prior treatment history that included CBASP psychotherapy.
Exclusion Criteria
Exclusion included anyone reporting the following disorders (lifetime): schizophrenia, schizotypal, or schizoaffective disorders; bipolar disorder, exhibiting a high level of suicidality judged by the clinical rater, borderline personality disorder; presenting with an active eating disorder (not in remission for at least 6 months), reporting an obsessive–compulsive disorder, dementia, attention deficit disorder or attention deficit hyperactive disorder as a primary diagnosis; reporting a primary diagnosis of panic, generalized anxiety, social phobia; current post-traumatic stress disorder if it was the primary diagnosis; a seizure disorder, history of a stroke, traumatic brain injury (TBI), active substance-use disorder or dependence disorder (nicotine and occasional marijuana usage were allowed) 6 months prior to screening; any potential disruptions to the commitment of the study (e.g., divorce pending, extended travel planned during the time of the study, planning for pregnancy during study, upcoming wedding) and a primary diagnosis of learning or processing disorder (the clinical significance was evaluated and the effect on their ability to learn at present was considered).
Study Design
Procedures
The study adhered to the guidelines for a single-case (N = 1) systematic replication design (Sidman, 1960). Eligible patients were randomly assigned to one of the three therapy groups to be administered 20 sessions. The CBASP model was dismantled into two monotherapy cells (Situational Analysis [SA], Interpersonal Discrimination Exercise [IDE]) and Combination [SA + IDE]. Two early-onset PDD patients were randomly assigned to each of the three cells.
Participants who completed 10 sessions were to be classified as “completers.” As noted, one participant dropped out after the eighth session; however, excluding the substituted participant who dropped out, all participants were completers and received a full dose of 20 sessions. Two psychotherapists each administered a SA cell, an IDE cell, and a treatment combination cell. Both therapists had 2 decades of experience and were certified in CBASP under the supervision of Dr. James P. McCullough, Jr. Every psychotherapy session was videotaped and approximately every third session was rated for protocol adherence by McCullough and Penberthy, both CBASP trainers.
Session Description of the Treatment Guidelines:
-
Session 1 of all three Cells: “Getting to know each other” introductory session. Significant Other History (SOH) List assigned to be reviewed during Session 2 of all three treatment Cells.
-
Session 2 of all three Cells: SOH administered, and Transference Hypothesis (TH) constructed.
-
Sessions 3–20 of the SA Cell: One SA administered per session. Generalization discussions were conducted concerning what had been learned and what could be applied to other similar situations. No discussion of dyadic interpersonal relationships was permitted nor was a discrimination discussion conducted involving the therapist and any significant other(s) that might mimic the work of the IDE exercise.
-
Sessions 3–20 of the IDE Cell: One IDE task administered per session focused on the therapist and significant other(s) in the patient’s life. No problem-solving interventions mimicking the work of the SA exercise were conducted.
-
Sessions 3–20 of the Combination Cell: Traditional CBASP therapist administration was conducted in the Combination Cell. SA was administered in approximately 70% of the sessions and the IDE was administered in approximately 30% of the sessions.
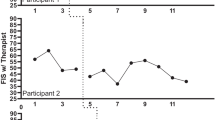
Acquisition learning was rated by the two therapists on the 5-step SA exercise and the 4-step IDE exercise at the end of every Session, 3–20. Rating acquisition learning was rated based on the degree to which participants could independently self-administer each of the five SA steps (Fig. 3) and each of the four IDE steps (Fig. 4) with no help or prompts from the therapist.
Dependent Measures
The dependent variables of the study were the following: (a) the 17-item Structured Interview Guide for the Hamilton Depression Rating Scale (SIGH-D: Williams, 2001, 2013) functioned as the primary outcome measure and was administered by the Study Coordinator at screening (prior to Session 1), mid-point (Session 10), and endpoint (Session 20); (b) the Beck Depression Inventory-II (BDI-II: Beck et al., 1996) was obtained at screening and at the beginning of every session thereafter; (c) the acquisition learning of the SA (5-point scale) and the IDE (4-point scale) exercises (McCullough, 2000) were rated by the two therapists at the end of sessions 3–20; (d) a Pre-post Revised Global Assessment of Functioning Scale (GAF-R: McCullough, 1996) was rated by the Study Coordinator at intake and endpoint; and (e) a post-Session 3 and post-Session 20 Impact Message Inventory (IMI: Kiesler & Schmidt, 1993) rating was obtained on each patient by the cell psychotherapist.
Data Analysis and Interpretation
Data were evaluated by visual inspection and clinical judgment. Data of the two patients assigned to each treatment cell (i.e. SA, IDE & Combination cells) were summed with means calculated to illustrate treatment response.
The IMI data enabled the therapists to interpret the impact scores in several ways: (1) the Octant Peak Score was the Impact Octant obtaining the highest impact rating; a Peak Score at baseline rated on the Hostile Side of the Interpersonal Circle (Kiesler, 1988) suggested “keeping one’s distance from others (i.e. moving away) in interpersonal interactions;” peak score on the Friendly side of the Interpersonal Circle suggested “moving toward the other in a facilitative manner;” (2) the Nadir Octant Score (Kiesler, 1988) denoted the Octant opposite the baseline Peak Score. Since PDD patients frequently obtain a Peak Score on the Hostile Side of the Interpersonal Circle at baseline, Nadir Score usually falls on the Friendly Side and was used as one interpersonal goal for the end of treatment. To be rated as a “clinical increase,” a pair-mean value of a 0.5 increase on the Nadir Octant must be rated when the endpoint octant score was compared to the baseline Octant score.
(3) The Total Amount of Space enclosed on the Hostile Side of the Interpersonal Circle at baseline and at endpoint of treatment was a judgment interpretation on the part of the therapist and was used as an index of interpersonal “avoidance” when compared to the Total Amount of Space enclosed on the Friendly Side. Comparing the Total Amount of Space changes when the baseline was compared to the endpoint denoted change in the degree of shift from avoidance to interpersonal approach. In addition, the endpoint Nadir Score at endpoint was also examined to see if it was consistent with the shift in the Total Amount of Space when baseline interpersonal impacts were compared to endpoint impacts.
Results
Therapist adherence was rated on a 3-point scale, and the ratings were completed by two CBASP clinical raters (McCullough and Penberthy) approximately every third session. The adherence-to-protocol data are shown in Table 1.
Table 1. Adherence Rating Scores for the two study therapists were averaged for 20 sessions of psychotherapy and presented as one value in the SA Cell, IDE Cell, and Combination Cell. The Adherence Rating Scale was rated three times approximately every third session. Ratings were scored: 1: Unsatisfactory Adherence; 2: Fair Adherence; 3: Satisfactory Adherence; N/R: Segment not Ratable.
The Structured Interview Guide for the Hamilton Depression Rating Scale (SIGH-D) data are shown in Fig. 1 at intake (screening), Week 10 (midpoint), and Week 20 (endpoint).
The Beck Depression Inventory scores were rated every session and averaged for two patients per treatment cell for Weeks 1–20. The BDI-II data are shown in Fig. 2.
The acquisition learning of the SA and IDE are shown below in Figs. 3 and 4. BDI-II data are also illustrated in both figures for comparative purposes and illustrate the M BDI-II averaged scores calculated for the same two Treatment Cell patients each week.
The Revised Global Assessment of Functioning Scale (GAF-R) evaluated the degree to which the participant’s depression symptoms interfered with their daily functioning in the work, school, or social interaction domains (i.e., symptoms causing the participant to miss work, interrupting school performance, or leading to withdrawal from social contacts). The GAF-R data are illustrated in Fig. 5.
As noted above, the Impact Message Inventory (IMI) assessed for interpersonal functioning change in three ways at pre-post Sessions 3 and 20: (1) peak octant score values, (2) nadir score values, and (3) total amount of circle space included when the Hostile (left side) and Friendly (right side) hemispheres were compared. The study therapists completed the IMI on each of their three cell participants at the end of the Sessions 3 (pre) and 20 (post). Again, the peak and nadir scores, and total space areas for the two participants in each treatment cell condition were averaged and plotted on three IMI circles as one data point on the respective treatment circles. The IMI data are presented in Fig. 6.
Discussion
This Stage 1b pilot study reflects a first-step attempt to dismantle the CBASP model with the ultimate, long-term research goal being that of identifying possible active ingredients. The present investigation administered the two CBASP major component-techniques (SA & the IDE) alone while a third component group administered both SA and the IDE in a treatment-as-usual format. As noted earlier, our goal herein was to determine if the outcome data across the three groups produced visually-inspected differential data patterns under controlled dismantling conditions.
Differential data patterns between all three groups were achieved across all dependent measures; that is, the SIGH-D, the Beck Depression Inventory, the GAF-R, and Kiesler’s IMI. When we placed the dependent measures across groups beside one another to observe the patterns, we found that both the SA and IDE treatment conditions decreased depression intensity in the treatment groups; however, the greatest differential decreases were observed in the SA problem-solving cells (i.e. the SA group and the combination SA & IDE group).
The pre-post GAF-R ratings reflected similar differential patterns for the three cells. Both cells involving SA appeared to improve familial, school, social, and occupational functioning to a greater degree than the IDE-alone group. Of the three domains assessed on the IMI, the Peak Octant scores (Hostile, Hostile-Submissive, & Submissive) in all three groups were consistent with the usual profiles of a PDD patient (McCullough, 2000; McCullough et al., 2015, p. 83ff). One notable outcome pattern on the IMI was the Nadir Goals which were achieved in the Interpersonal Group that achieved the + 0.5 rate increases in all three endpoint Nadir Octants. It should be mentioned that interpersonal functioning was the primary focus of the IDE Group.
Summarily, we did achieve visually-inspected differential data patterns across the three groups when we observed the group x dependent measure domains. Based on these data, a larger dismantling study seems warranted and should be undertaken.
Strengths and Limitations of the Study
Strengths of the study were observed in the therapist adherence ratings; the two therapists clearly administered the the SA and IDE groups to acceptable protocol levels. Patients also learned both the SA and IDE exercises to criterion suggesting that as far as the patient-subjects were concerned, they mastered the subject matter of the SA and IDE groups. Why is this important? If patients provide evidence that they have learned the subject matter of CBASP, they should be in an optimal position to cope effectively with the theoretical stress-challenges that CBASP opines maintain the PDD disorder (McCullough, 2000;, 2006; McCullough et al., 2015).
Finally, a serious limitation of this Stage Ib pilot study (Rounsaville et al., 2001) was the small N that limits any comparative conclusions we might otherwise draw. A Stage II replicated study is clearly mandated by these results.
References
Ahn, H. N., & Wampold, B. E. (2001). Where oh where are the specific ingredients? A meta-analysis of component studies in counseling and psychotherapy. Journal of Counseling Psychology, 48(3), 251–257. https://doi.org/10.1037/0022-0167.48.3.251.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed). American Psychiatric Publishing. https://doi.org/10.1176/appi.books.9780890425596.
Beck, A., Steer, R., & Brown, G. (1996). BDI-II: Beck depression inventory. Pearson. https://doi.org/10.1037/t00742-000.
Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of Depression. Guilford Press.
Bell, E. C., Marcus, D. K., & Goodlad, J. K. (2013). Are the parts as good as the whole? A meta-analysis of component treatment studies. Journal of Consulting and Clinical Psychology, 81(4), 722–736. https://doi.org/10.1037/a0033004
Furukawa, T., Schramm, E., Weitz, E., Salanti, G., Efthimiou, O., Michalak, J., Watanabe, N., Cipriani, A., Keller, M., Kocsis, J., Klein, D., & Cuijpers, P. (2016). Cognitive- Behavioral Analysis System of Psychotherapy (CBASP), a drug, or their combination: differential therapeutics for persistent depressive disorder: A study protocol of an individual participant data network meta-analysis. BMJ Open, 6(5), 1–6. https://doi.org/10.1136/bmjopen-2016-011769
Hom, M., Stanley, I., Vazquez, A., Belz, M., & Joiner, T. (2017). Gains in cognitive behavioral analysis system of psychotherapy: Examining treatment progress and processes of change in a psychiatric outpatient sample. International Journal of Cognitive Therapy, 10(3), 255–268. https://doi.org/10.1521/ijct.2017.10.3.255
Jacobson, N. S., Dobson, K. S., Truax, P. A., Addis, M. E., Koerner, K., Gollan, J. K., Gortner, E., & Prince, S. E. (1996). A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology, 64(2), 295–304. https://doi.org/10.1037/0022-006X.64.2.295.
Kazdin, A. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432
Kazdin, A., & Nock, M. (2003). Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, 44, 1116–1129. https://doi.org/10.1111/1469-7610.00195
Keller, M., McCullough, J., Klein, D., Arnow, B., Dunner, D., Gelenberg, A., Markowitz, J., Nemeroff, C., Russell, J., Thase, M., Trivedi, M., & Zajecka, J. (2000). A comparison of nefazodone, the cognitive behavioral analysis system of psychotherapy, and their combination for the treatment of chronic depression. New England Journal of Medicine, 342(20), 1462–1470. https://doi.org/10.1056/NEJM200005183422001
Kiesler, D. (1988). Therapeutic metacommunication: Therapist Impact Disclosure as Feedback in Psychotherapy. Consulting Psychologist Press.
Kiesler, D. J., & Schmidt, J. A. (1993). Impact message inventory–circumplex octant scale version (IMI). APA PsycTests. https://doi.org/10.1037/t64697-000
McCullough, J. (1996). The procedure for standardizing the rating of Axis V functioning in the DSM-IV-TR (GAF-R). Virginia Commonwealth University. Unpublished Manuscript.
McCullough, J. (2000). Treatment for Chronic Depression: Cognitive behavioral analysis system of psychotherapy (CBASP). Guilford Press.
McCullough, J. P. Jr. (2006). Treating Chronic Depression with disciplined personal involvement: CBASP. Springer. https://doi.org/10.1007/978-0-387-31066-4.
McCullough, J. P. Jr., Lord, B. D., Conley, K. A., & Martin, A. M. (2010). A method for conducting intensive psychological studies with early-onset chronically depressed patients. American Journal of Psychotherapy, 64 (4), 317–337.
McCullough, J. P. Jr., Schramm, E., & Penberthy, J. K. (2015). CBASP as a distinctive treatment for persistent depressive disorder. Routledge. https://doi.org/10.1176/appi.psychotherapy.2010.64.4.317
Negt, P., Brakemeier, E., Winter, L., Bleich, S., & Kahl, K. (2016). The treatment of chronic depression with cognitive behavioral analysis system of psychotherapy: A systematic review and meta-analysis of randomized-controlled clinical trials. Brain and Behavior, 6(8), 1–25. https://doi.org/10.1002/brb3.486
Papa, A., & Follette, W. C. (2015). Dismantling studies of psychotherapy. The encyclopedia of clinical psychology (pp. 1–6). John Wiley. https://doi.org/10.1002/9781118625392.wbecp523
Penberthy, J. K. (2019). Persistent depressive disorders. Hogrefe Publishing. https://doi.org/10.1027/00505-000.
Rounsaville, B. J., Carroll, K. M., & Onken, L. S. (2001). A stage model of behavioral therapies research: Getting started and moving on from Stage I. Clinical Psychology: Science and Practice, 8 (2), 133–142.
Schramm, E., Kriston, L., Zobel, I., Bailer, J., Wambach, K., Backenstrass, M., Klein, J., Schoepf, D., Schnell, D., Gumz, A., Bausch, P., Fangmeier, T., Meister, R., Berger, M., Hautzinger, M., & Härter, M. (2017). Effective disorder-specific vs nonspecific psychotherapy for chronic depression: A randomized clinical trial. JAMA Psychiatry, 74(3), 233–242. https://doi.org/10.1001/jamapsychiatry.2016.3880
Sidman, M. (1960). Tactics of scientific research: Evaluating experimental data in psychology. Basic Books.
Williams, J. B. (2001). Standardizing the Hamilton Depression Rating Scale: Past, present, and future. European Archive of Psychiatry and Clinical Neuroscience, 251(2), 6–12. https://doi.org/10.1007/BF03035120
Williams, J. B. (2013). Structured interview guide for the Hamilton Depression Rating Scale-17 Item Version (SIGH-D-17) – SLE since last evaluation (SLE) version.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Long, L.R., Foster, M., Burr, K. et al. Pilot Study Dismantling the Cognitive Behavioral Analysis System of Psychotherapy: Identifying the Active Ingredients. Cogn Ther Res (2024). https://doi.org/10.1007/s10608-024-10467-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s10608-024-10467-z