Abstract
Rumination is considered a cognitive vulnerability factor in the development and maintenance of depression. The metacognitive model of rumination and depression suggests that the development of rumination and its association with depression partly depends on metacognitive beliefs. Two metacognitive beliefs about rumination have been identified: positive beliefs about its utility and negative beliefs about the uncontrollability and its negative social consequences. We conducted a systematic review and meta-analysis aimed: (1) to analyze the associations between metacognitive beliefs and rumination and depression; (2) to test the metacognitive model, using a Two-Stage Structural Equation Modeling approach (TSSEM). Literature search retrieved 41 studies. These 41 studies (N = 10,607) were included in the narrative synthesis and meta-analysis, and 16 studies (N = 4477) were comprised for the TSSEM. Results indicated metacognitive beliefs are associated with rumination and depression. Measures on metacognitive beliefs about rumination indicated that positive beliefs showed moderate associations with rumination (r = 0.50), and low with depression (r = 0.27); whereas negative beliefs showed moderate associations with both rumination (r = 0.46) and depression (r = 0.49). These results were consistent across studies using different instruments to measure metacognitive beliefs, and in both clinical and nonclinical samples. Moreover, results of the TSSEM analyses showed that the metacognitive model had a good fit. In sum, our results are in line with the metacognitive model of rumination and depression, highlighting that metacognitive beliefs are relevant factors to understand why people ruminate and get depressed. Future directions and clinical implications are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is one of the leading causes of disability worldwide (Kessler & Bromet, 2013) and one of the most debilitating mental disorders (Mrazek et al., 2014). It is a highly prevalent and often chronic condition with high costs, as shown in the relapse and recurrence rates, in addition to the substantial proportion of treatment-resistant patients (Beshai et al., 2011; Thomas et al., 2013). Therefore, research that examines the risk factors and underlying mechanism of depression is needed to achieve significant theoretical and clinical advances.
Rumination is a key cognitive feature of depression (Nolen-Hoeksema et al., 2008; Papageorgiou & Wells, 2004, 2009). According to Nolen-Hoeksema et al. (2008), it is defined as repetitive negative thinking that focuses an individual’s attention on his or her depressive symptoms and on the causes, implications, and meanings of these symptoms. Rumination is considered to be a maladaptive emotion regulation strategy used in response to negative affect (Joormann & Quinn, 2014). Moreover, it is a strategy that exacerbates and prolongs depression, for example, enhancing the depressed mood, negatively biasing thinking, or interfering with effective problem solving (Lyubomirsky & Tkach, 2004). Likewise, many studies have highlighted rumination as a cognitive vulnerability factor in the development and maintenance of depression (for a review, see Nolen-Hoeksema et al., 2008; Watkins & Roberts, 2020). After exposing the role of rumination in depression and its negative consequences, a relevant aim of research has been to examine what factors lead people to use this strategy.
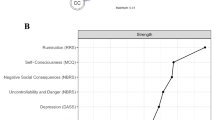
An answer to this can be found in the metacognitive model of rumination and depression (Papageorgiou & Wells, 2003, 2004; Wells, 2009). The metacognitive model, which is based on a broader model of emotional disorders called the self-regulatory executive function (S-REF; Wells, 2019; Wells & Matthews, 1994, 1996), suggests that the activation and maintenance of rumination, and its association with depression, are dependent on metacognitive beliefs. Metacognitive beliefs refer to stable beliefs people have about their own cognitive system, which influence the control, monitoring, and appraisal of cognition. There are two principal metacognitive beliefs: positive beliefs, referring to the utility of rumination (e.g., “I need to ruminate to find answers to my problems”), and negative beliefs, referring to the uncontrollability and danger of rumination (e.g., “rumination about my problems is uncontrollable”) and its negative interpersonal and social consequences (e.g., “people will reject me if I ruminate”). According to the model (see Fig. 1), positive metacognitive beliefs about the utility of rumination are activated in response to a trigger (negative mood or thoughts), leading people to use rumination. Rumination is supposed to overcome the negative situation and help understand the problem or solve it; however, as reviewed above, rumination is usually not useful and, instead, leads to even more negative thoughts and increases the negative effect. As a result, negative metacognitive beliefs related to the uncontrollability and harmfulness of rumination and its negative interpersonal and social consequences emerge. These negative beliefs lead people to appraise their own rumination as uncontrollable and dangerous (e.g., socially), increasing the accessibility of negative information (e.g., negative emotions or thoughts), and thus enhancing depressive symptomatology. From this approach, metacognitive beliefs are causal factors in predicting rumination and depression (Wells, 2009, 2019).
To test the metacognitive model, two different scales have been developed to assess positive and negative metacognitive beliefs: the Positive Beliefs About Rumination Scale (PBRS; Papageorgiou & Wells, 2001b) and the Negative Beliefs About Rumination Scale (NBRS; Papageorgiou & Wells, 2001a). Whereas the PBRS has a one-factor structure, the NBRS comprises two different subscales: negative beliefs about the uncontrollability and harmfulness of rumination and negative beliefs about the social and interpersonal consequences of rumination. Likewise, a few studies have used the PBRS-A (Watkins & Moulds, 2005), a modified version in which the wording of items was rephrased to avoid references to depression and rumination, thereby reducing the criterion contamination. The PBRS, the NBRS, and the adapted version (PBRS-A) have shown good psychometric properties and are valid measures to assess metacognitive beliefs about rumination (Luminet, 2004; Watkins & Moulds, 2005).
In addition to these scales specifically focused on rumination, the gold-standard instrument to assess metacognitive beliefs is the Meta-Cognitions Questionnaire (MCQ-30; Wells & Cartwright-Hatton, 2004). This questionnaire was designed to assess individual differences in dysfunctional metacognitive beliefs. It is composed of five subscales: (1) positive beliefs about worry (e.g., “Worrying helps me cope”); (2) negative beliefs of uncontrollability and danger (e.g., “I cannot ignore my worrying thoughts”); (3) cognitive confidence (e.g., “I have a poor memory”); (4) need to control thoughts (e.g., “I will be punished for not controlling certain thoughts”); and (5) cognitive self-consciousness (e.g., “I monitor my thoughts”). Although two of the MCQ subscales are specifically focused on worry, this instrument has been widely used to obtain evidence related to the metacognitive model of rumination and depression, and there is a growing body of research that has used the MCQ and shown that metacognitive beliefs are a transdiagnostic factor in psychopathology (for a review, see Sun et al., 2017; Wells, 2019).
The metacognitive model of rumination and depression is applicable both theoretically and clinically. It is theoretically relevant because it suggests that metacognitive beliefs have a causal role in explaining why people ruminate and get depressed, so its study could lead to a more complete understanding of vulnerability to depression. It is clinically relevant because metacognitive beliefs can be formulated as a major target in therapy, and therapeutic interventions can be developed to modify these beliefs. Thus, this model has led to a metacognitive-focused therapy for depression (Papageorgiou & Wells, 2004; Wells, 2009). This therapy works to bring rumination under executive control, modifying maladaptive metacognitive beliefs and allowing higher flexibility in processing negative thoughts and affect; it has shown promising preliminary results for depression (Hagen et al., 2017a; Hjemdal et al., 2017), even in recurrent and persistent cases (Wells et al., 2009; Winter et al., 2019). These implications warrant the need to review and delve into this model.
Our Study
We present a systematic review and meta-analysis of the empirical research focused on the study of the metacognitive model of rumination and depression (Papageorgiou & Wells, 2003, 2004; Wells, 2009). We had two specific goals: (a) to review studies that examined the link between metacognitive beliefs and rumination and depression, pooling the correlations between metacognitive scales (PBRS/NBRS and MCQ) and depression/rumination, and examining the effect of three moderator variables: type of instrument (PBRS/NBRS vs. MCQ), type of sample (clinical vs. nonclinical), and proportion of women in the sample; (b) to review studies that tested the model by jointly examining the associations between metacognitive beliefs, rumination, and depression, and testing the metacognitive model through the two-stage structural equation modeling approach (TSSEM; Cheung & Chan, 2005).
Our intention was to develop a clear picture of the current state of research about the model and draw conclusions that may help future research in the field and potentially guide the implementation of practical interventions.
Method
Literature Search
PsycINFO, PubMed, and Scopus databases were searched exhaustively over the period November 10–13, 2019, for articles published in Spanish and English in scientific journals. We searched for studies examining the link between metacognitive beliefs, rumination, and depression. For this purpose, relevant articles were tagged when they contained “metacognition” or “metacognitive beliefs” as keywords or as a term in the title or abstract, together with one or more additional search terms. In PsycINFO and Scopus, these additional terms were “rumination,” “brooding,” “depression,” and “major depression”; in PubMed, they were the medical subject headings (MeSH) terms “rumination, cognitive,” “depression,” and “major depression.”
Inclusion and Exclusion Criteria
We selected studies if they met the following inclusion criteria: (a) they were empirical studies that examined the relationship between metacognitive beliefs, rumination, and/or depression; (b) they used nonclinical samples or depressed samples (studies in which the primary disorder was depression); and (c) they measured metacognitive beliefs. We included studies that used instruments to specifically measure metacognitive beliefs about rumination but also considered those studies that measured metacognitive beliefs using the MCQ-30.
We rejected studies if they met the following exclusion criteria: (a) they were theoretical studies, reviews, or meta-analyses; (b) they were written in a language other than English or Spanish; and (c) they used clinical samples in which the primary disorder was not depression.
Data Extraction
Database searches identified 1,125 relevant studies: 248 in PsycINFO, 318 in PubMed, and 559 in Scopus (Fig. 2). Elimination of duplicates gave 499 potentially eligible studies. Two independent reviewers (JBCL and EGS) screened the titles and abstracts according to the inclusion and exclusion criteria. A third reviewer (JMS) participated in cases of disagreement. This review excluded 398 studies, thus leaving 101. The full text of these studies was read, and 60 were deleted principally because (a) the primary disorder in clinical samples was not depression, and/or (b) they did not include a measure of metacognitive beliefs. A final set of 41 studies met all inclusion criteria and empirically analyzed the relationship between metacognitive beliefs and rumination and/or depression.
Of the 41 studies, 16 used the PBRS and/or the NBRS, and the remaining 25 used the MCQ. It is important to note that some studies used the PBRS-A (Watkins & Moulds, 2005). On the other hand, the Ruminative Response Scale (RRS; Nolen-Hoeksema & Morrow, 1991) and the Beck Depression Inventory (BDI; Beck et al., 1961) were more frequently used to measure rumination and depression, respectively.
Results
Narrative Synthesis of Findings
To present the results systematically, we consider separately the studies performed with the PBRS/NBRS and the MCQ-30. Within each set of instrument-specific studies, we consider separately studies based on nonclinical and clinical samples. Thus, key information about the studies included in this review is presented as follows: Table 1 contains studies performed with the PBRS/NBRS using nonclinical samples, Table 2 describes studies performed with the PBRS/NBRS using clinical samples, Table 3 indicates studies performed with the MCQ-30 using nonclinical samples, and Table 4 specifies studies performed with the MCQ-30 using clinical samples. These tables describe the variables analyzed, the size and characteristics of the sample, the type of design used, the instruments used, and the principal findings of each study.
Results with the PBRS/NBRS
From the 16 studies that used the PBRS/NBRS, 12 used a nonclinical sample (eight cross-sectional and four longitudinal) and four used a clinical sample (three cross-sectional and one longitudinal). Most studies (12) examined the associations between the PBRS and/or NBRS with both depression and rumination, three did it only with rumination, and the remaining study only with depression. Furthermore, from the total, six tested the metacognitive model of depression and rumination through path analysis.
Nonclinical Sample
The 12 studies that used nonclinical samples were mainly composed of undergraduate students, regardless of the design. In general, the results of these studies showed positive and significant correlations between metacognitive beliefs and key variables.
In cross-sectional studies, the strongest associations with rumination were for the PBRS and the NBRS uncontrollability and harm subscale. On the other hand, the strongest correlations with depression were for the NBRS social consequences subscale. Four studies tested the metacognitive model of rumination and depression using path analysis; the results were in line with the tenets of the model: Positive beliefs lead to rumination, and rumination leads to depressive symptoms both directly and indirectly through negative metacognitive beliefs. However, there were contradictory results regarding what subscale of the NBRS was associated with depression. In this sense, Papageorgiou and Wells (2003) found that only metacognitive beliefs about social consequences lead to depressive symptoms, while Roelofs et al. (2007) found that the uncontrollability and harm subscale also did so. Solem et al. (2016), using the largest sample—1433 individuals from the general population—also found stronger correlations for the NBRS uncontrollability and harm subscale than for the social consequences subscale (Table 1).
The results from the four longitudinal studies partially corroborated those found in cross-sectional studies, with time intervals ranging from one to six months. Weber and Exner (2013) found that the time 1 PBRS explained significantly more variance in time 2 rumination after controlling time 1 rumination. Kubiak et al. (2014) carried out an ecological momentary assessment (EMA) and examined the effect of the PBRS on rumination and positive affect. They found that the PBRS predicted rumination and that the effect of the PBRS on momentary positive affect was significantly mediated by rumination, while the direct effect was not significant. Papageorgiou and Wells (2009) showed that the NBRS uncontrollability and harm subscale was the only significant predictor of depression at time 2 (after controlling for depressive symptoms at baseline). Notably in this study, the NBRS was a negative predictor, although the NBRS (time 1) and depression (time 2) were positively associated in bivariate correlations. More recently, Matsumoto and Mochizuki (2018) conducted a cross-lagged effect modeling and found that, except for the association between PBRS and depression at time 2, all the correlations of PBRS and NBRS were positive and significant with depression and rumination and that negative metacognitive beliefs predicted prominent levels of depression (at time 2).
Clinical Sample
The samples of the four studies were heterogeneous. In one study, participants were patients from a charitable organization, and in another one they were people seeking treatment in a mood disorder program. The only longitudinal study specified recurrent major depression disorder (MDD) as an inclusion criterion. All studies examined associations between metacognitive beliefs, depression, and rumination.
In cross-sectional studies, the PBRS showed stronger associations with rumination, while the NBRS subscales presented stronger associations with depression, especially the uncontrollability and harm subscale. Watkins and Moulds (2005) used both the PBRS and the PBRS-A and showed that both questionnaires had positive and significant correlations with depression and rumination, although the PBRS showed the strongest correlations. On the other hand, the remaining two studies tested the metacognitive model through path analysis (Papageorgiou & Wells, 2003; Roelofs et al., 2010), showing results in line with the tenets of the metacognitive model. Nevertheless, as in the nonclinical sample, they found contradictory results regarding which subscale of the NBRS led to depressive symptoms: Papageorgiou and Wells (2003) found that both subscales did so, while Roelofs et al. (2010) found that only the NBRS social consequences subscale led to depressive symptoms.
Only one study (Kraft et al., 2019) used a longitudinal design with a five-time interval over 12 months. The latent growth model showed that the PBRS, the NBRS, and rumination predicted depression levels. They found that positive metacognitions predicted depression levels, but rumination accounted for the effect. Rumination and negative metacognitions had independent contributions to depression. This finding is in line with previous studies and with the metacognitive model, but contrary to the model, negative metacognitions and rumination did not predict symptom recurrence. The authors concluded that although reduced metacognition is likely to reduce depressive symptoms, this phenomenon is probably not enough to prevent the recurrence of symptoms in the next 12 months (Kraft et al., 2019).
In sum, the results of the studies reviewed in this section show the following, regardless of the sample used: (a) the PBRS is associated with rumination and depression, both cross-sectionally and longitudinally, although it is more strongly correlated with rumination; (b) the NBRS is associated with rumination and depression, both cross-sectionally and longitudinally, although in this case the NBRS is more strongly correlated with depression; (c) studies using path analyses confirm the metacognitive model, showing that positive beliefs lead to rumination and that rumination leads to depressive symptoms both directly and indirectly through negative metacognitive beliefs; and (d) there are contradictory results with respect to which NBRS subscale leads to depression in path analyses.
Results with the MCQ-30
From the 25 studies we identified, 22 used a nonclinical sample (19 cross-sectional and three longitudinal) and three used a clinical sample (two cross-sectional and one longitudinal). Most studies examined the associations between each of the five MCQ-30 subscales. Furthermore, the vast majority (21 studies) examined the associations with depression, only three with rumination, and the remaining one with both variables.
Nonclinical Sample
All studies used a convenience sample: 12 of them used undergraduate students, eight community samples, and two a mixture of both. In general, regardless of the instrument used to measure depression, the results of the reviewed studies demonstrated that metacognitive beliefs are positively and significantly correlated with depression. From the studies that examined the specific effect of each MCQ subscale, there were stronger associations with depression for the negative beliefs subscale, followed by the need to control thoughts subscale. Moreover, Dethier et al. (2017) found that these results remained even after controlling for anxiety, a variable classically associated with the MCQ. Only two studies examined associations with rumination; they found contradictory results. Razavizadeh Tabadkan and Mohammadi Poor (2016) found negative correlations for all MCQ subscales and rumination, while Palmieri et al. (2018) only examined the MCQ total correlation and found a positive and significant correlation. Finally, Karatepe et al. (2013) examined associations of two MCQ subscales—negative beliefs and need to control thoughts—with both depression and rumination. Their results showed that correlations between these subscales and rumination were stronger than with depression.
Three studies used a longitudinal design with a nonclinical sample. First, McEvoy et al. (2013) examined associations between metacognitive beliefs and rumination in two studies; they found that negative beliefs showed the strongest positive associations with rumination, followed by the need to control thoughts subscale (study 1), and that these subscales were the only unique predictors of rumination (study 2). Subsequently, Yilmaz et al. (2011), using a six-month follow-up interval, found that negative beliefs concerning uncontrollability and danger predicted depressive symptoms, after controlling for the baseline depression level. Finally, Ruiz and Odriozola-González (2015) conducted the study with the longest time interval (nine months) and the largest sample (N = 286 at time 1) and examined the associations between depression and three of the five MCQ subscales (positive beliefs, negative beliefs, and need to control thoughts). Again, negative beliefs and the need to control thoughts were the two subscales most strongly related to depression at both times 1 and 2; however, they did not control for depression at time 1 in the analyses.
Clinical Sample
The three studies conducted with a clinical sample examined the associations between metacognitive beliefs and depression. In two studies, participants were patients with actual MDD, and the other one compared groups of currently depressed, previously depressed, and never depressed individuals.
The two cross-sectional studies reported different results. Sarisoy et al. (2013) showed that only the MCQ need to control thoughts subscale had significant associations with depression even though they used a small sample (N = 51). On the other hand, Solem et al. (2015a) found that the negative beliefs subscale showed the strongest correlations with depression, followed by the need to control thoughts subscale. The regression analyses showed that cognitive confidence, positive beliefs, and negative beliefs emerged as significant predictors of depression severity.
Only one study (Faissner et al., 2018) used a longitudinal design in a clinical sample, with a time interval of 3.5 years. They measured the severity of depression using both clinician-rated and self-report measures. According to the regression analysis, the negative beliefs subscale (initial status and change) was the only predictor of change in clinician-assessed depression. In the case of self-reported depression, both the negative beliefs and need to control thoughts subscales (initial status and change) had a significant effect on the change in the BDI. These results again indicate the importance of the negative beliefs subscale.
In summary, the vast majority of studies reviewed in this section have examined the associations between metacognitive beliefs and depression, and the results have shown that the most relevant subscale is the negative beliefs about worry, followed by the need to control thoughts. Few studies have measured rumination to examine its associations with metacognitive beliefs, but the results seem to point in the same direction. These results have also been corroborated in longitudinal studies, where the negative beliefs subscale also showed more relevance.
Meta-Analysis
In order to statistically combine the correlation coefficients, they were first converted into Fisher’s Z scores in order to avoid that the sampling variance is correlated to the magnitude of the effect size. For providing the results, Fisher’s Z were back transformed to correlation coefficients (the formulas can be found in Cooper et al., 2019, pp. 220–221). Most studies that used the instrument NBRS did not report the correlation of the total NBRS scale, but the correlation of the subdimensions (NBRS uncontrollability and harm and NBRS social consequences). Within these studies, a composite correlation between the subdimensions was obtained in order to get an overall correlation between NBRS and depression and rumination. To obtain this composite correlation, we followed the procedure explained in Borenstein et al., (2009, p. 225), assuming a correlation of 0.57 between NBRS subscales (Papageorgiou & Wells, 2003).
A random-effects model was performed, given that substantial heterogeneity was observed across studies. The I2 index was used to quantify the amount of heterogeneity (Higgins & Thompson, 2002) and can be interpreted as the percentage of variance observed that is due to between-studies variability. A meta-analysis was performed if there were more than five effect sizes available for a given correlation (see supplementary material for further information). Analyses were done in R, using the metafor package (Viechtbauer, 2010).
Publication Bias
The presence of publication bias was explored through the visual inspection of the funnel plot (see supplementary material) and through the Egger regression test (Egger et al., 1997). These analyses were only carried out on those subsets of data where more than 10 effect sizes were available. The visual inspection of the funnel plots revealed some asymmetries for the correlation between the MCQ negative beliefs and depression and between the NBRS negative beliefs with both variables, rumination and depression. For these correlations, less precise studies showed more attenuated correlations than more precise studies, meaning that the overall effect sizes might be slightly attenuated. Thus, the Egger regression test indicated that publication bias could exist in the correlations already mentioned, with all showing the same trend: highly precise studies show larger effect sizes.
Associations Between Metacognitive Beliefs and Rumination and Depression
Pooled correlations between the PBRS and NBRS scales with depression and rumination were all significant (see Table 5). Correlations of higher magnitude were found between NBRS uncontrollability and harm subscale with rumination and depression, respectively. Regarding the PBRS, we found a pooled correlation of moderate magnitude between the PBRS and rumination, whereas correlation with depression was the lowest. All the I2 indices, except for PBRS and depression and for NBRS (total) and rumination, were higher than 75%, meaning that there was a substantial between-studies variability (Table 5).
In the case of the MCQ scale, only pooled correlations with depression are shown (k > 5). All the pooled correlations were statistically significant (Table 5). The higher correlation was found between MCQ negative beliefs subscale and depression, followed by the pooled correlation between MCQ need to control thoughts and depression. The lowest correlation was found for MCQ self-consciousness. All the I2 indices, except for the MCQ positive beliefs subscale, were higher than 75% (Table 5).
We carried out a series of meta-regression models to investigate the effect of three moderator variables: type of instrument used to measure metacognitive beliefs (PRBS/NBRS vs. MCQ), type of sample (clinical vs. nonclinical), and the proportion of women in the sample. The pooled effect size and the difference among the pooled Fisher’s Z were calculated together with a statistical test that investigated whether this difference was statistically relevant. Data showed that no statistical differences were observed across types of instruments or types of samples. However, there were significant results for the moderator variable proportion of women in the sample. In the case of the MCQ, correlations between depression and the subscales negative beliefs, need to control thoughts and cognitive confidence were stronger the more women there were in the sample. No effect of the percentage of women were found for the correlations involving PBRS/NBRS. It is important to note that the lack of statistically significant results in some analyses (differences in rumination between type of instrument or by type of sample) can be explained by the lack of statistical power. For further information, see the supplementary material.
Two-Stage Structural Equation Modeling Approach
To carry out a meta-analysis on the theoretical metacognitive model of rumination and depression, we used the TSSEM approach proposed by Cheung and Chan (2005). This analysis was done only on the subset of studies that used the PBRS/NBRS measures (k = 16; n = 4477). The first stage of this approach consists of pooling together the correlation matrices extracted from each study, obtaining a pooled correlation matrix. In this stage, a homogeneity test and goodness-of-fit indexes are provided to see whether a fixed-effect model should be fitted (which assumes that all correlation matrices stem from a common population correlation matrix) or whether a random-effects model is more appropriate (which assumes that all correlation matrices stem from different population correlation matrices). In the second stage, the pooled correlation matrix obtained in Stage 1 is used to fit a path analysis, specifying the theoretical model displayed in Fig. 1. The fit of the path model was evaluated by looking at the root mean square error of approximation (RMSEA) and at the comparative fit index CFI (CFI). A value of RMSEA below 0.06 and a value of CFI above 0.95 were considered an acceptable fit (Hu & Bentler, 1999). Likelihood-based confidence intervals are reported instead of the traditional confidence intervals (Cheung, 2009). Analyses were undertaken in R using the metaSEM package (Cheung, 2015).
The homogeneity test at Stage 1 indicated that substantial heterogeneity existed across correlation matrices (X2 = 212.46; df = 59, p < 0.002). However, this homogeneity test is conservative, and the CFI indicated that the fit was adequate (CFI = 0.965). Therefore, a fixed-effect model was assumed for this stage. Figure 1 contains the parameter estimates obtained after carrying the path analysis at Stage 2, using the pooled correlation matrix obtained in Stage 1 (see supplementary material). Likelihood-based confidence intervals indicate that all regression coefficients were significantly different from zero and were positive. The fit of this path model was adequate (CFI = 0.999; RMSEA = 0.021).
Discussion
The present review has focused on studies that examined the empirical evidence of the metacognitive model of rumination and depression. We reviewed and analyzed studies that examined the link between metacognitive beliefs and rumination, between metacognitive beliefs and depression, and, together, the interplay between metacognitive beliefs, rumination, and depression.
The principal conclusion that can be drawn from these reviewed studies is that metacognitive beliefs are associated with both rumination and depression. That is, people who hold dysfunctional metacognitive beliefs show higher levels of rumination as well as higher levels of depressive symptomatology. This result is consistent in both clinical and nonclinical samples, regardless of the measure employed to assess metacognitive beliefs (e.g., PBRS/NBRS, PBRS-A, or MCQ), and across different populations and study designs, with the same trend being found in cross-sectional or prospective studies. Moreover, according to the meta-analysis, negative metacognitive beliefs showed the strongest pooled correlations with both rumination and depression. Other more specific conclusions can also be drawn.
Studies that have used the PBRS and NBRS are especially informative about the metacognitive model of rumination and depression because these instruments are focused on dysfunctional metacognitive beliefs about rumination. Taken together, the narrative synthesis and the meta-analysis evinced that positive beliefs are more strongly associated with rumination than depression, whereas negative beliefs are similarly (and moderately) associated with both rumination and depression. Specifically, when comparing both subscales of the NBRS, the uncontrollability and harm subscale showed the strongest pooled correlation for both rumination and depression, respectively.
Likewise, studies that have used the MCQ-30 are also informative. Although some of the MCQ subscales are focused on worry, the MCQ is a widely used measure to assess metacognitive beliefs. In this case, most studies have focused on examining the links with depression. Thus, both narrative synthesis and meta-analysis have reported the same trend found so far with the PBRS/NBRS: negative metacognitive beliefs were the most strongly associated with depression. It is also noteworthy that all the other MCQ subscales were positively associated with depression, mainly the need to control thoughts subscale. These results suggest the relevance of examining the role of other metacognitive beliefs (in addition to positive and negative beliefs) in depression. On the other hand, taking into account that the MCQ is focused on worry (and not on rumination), these results are supportive of the idea that metacognitive beliefs are a transdiagnostic factor in psychopathology (Luca, 2019; Sun et al., 2017; Wells, 2019).
The meta-regression models showed that there were no differences in associations between metacognitive beliefs and rumination and depression based on the type of measure or sample. Therefore, results were consistent regardless of the instrument used, the PBRS/NBRS or the MCQ, and regardless of whether it is a clinical or nonclinical population. However, these results must be interpreted cautiously since there is an evident lack of statistical power. Given that previous studies have found gender differences in rumination (women ruminate more than men; Johnson & Whisman, 2013), we examined whether the proportion of women in studies might yield stronger effect sizes in associations between metacognitive beliefs and rumination and depression. No significant differences were found for rumination. However, we found that studies with a higher proportion of women showed stronger associations between some of the MCQ subscales (negative beliefs, cognitive confidence, need to control thoughts) and depression. This result suggests that the association between MCQ and depression is particularly relevant for women and suggests the need to consider gender in future research. Finally, an examination of the results in the narrative synthesis with respect to the design show that they were consistent regardless of whether it was a cross-sectional or longitudinal study.
Of particular relevance are the results of the TSSEM testing the metacognitive model of rumination and depression. When considering the studies examining the associations between the PBRS/NBRS and rumination/depression together, results of path analysis support the principal tenets of the model, namely that positive beliefs lead people to use rumination and that rumination, in turn, leads to the activation of negative beliefs involved in an increase in depressive symptoms (Papageorgiou & Wells, 2003, 2004; Wells, 2009). Thus, we found that positive beliefs were moderately associated with rumination, whereas rumination was both directly and indirectly associated with depression, also moderately, via negative beliefs. Previous studies that have tested the metacognitive model using path analyses have drawn contradictory conclusions about which NBRS subscale contributes more to depression; in this sense, our results can be enlightening. The TSSEM results indicated that the uncontrollability and harm subscale showed the strongest association with depression.
Altogether, the results of the reviewed and analyzed studies are in line with the metacognitive model, which suggests that positive and negative beliefs about rumination are key factors in understanding why people ruminate and get depressed. Specifically, we conclude that positive beliefs are more strongly associated with rumination, and negative beliefs are more strongly associated with both rumination and depression. Furthermore, those studies performed with the MCQ-30 have revealed the relevance of the metacognitive beliefs about the need to control thoughts, suggesting that it could be interesting to consider the role of this metacognitive belief in future reviews of the metacognitive model of rumination and depression.
While analyzing the literature in this field, we identified several limitations. First, there is a considerable heterogeneity among effect sizes across studies, which indicates that study characteristics might moderate the magnitude of the effect. Future meta-analysis could further explore this issue. Second, for three correlations, we found some evidence of publication bias. These analyses indicated that highly precise studies showed larger effect sizes, meaning that the observed pooled correlations might be somewhat attenuated. Third, a considerable number of studies have used cross-sectional and longitudinal designs, but no studies have employed experimental paradigms. This factor precludes causal inferences. The metacognitive model postulates that metacognitive beliefs are relatively malleable, so future research may be interested in experimentally manipulating metacognitive beliefs. There are precedents from the study of meta-emotion beliefs. For example, De Castella et al. (2018) examined whether people’s beliefs about their ability to control their emotions play a causal role in relevant psychological outcomes. For that purpose, the authors experimentally manipulated the emotional beliefs of participants and found initial evidence for their causal role in avoidance-based emotion regulation. Similar procedures could be used in the context of metacognitive beliefs. Fourth, there is a scarcity of instruments that assess dysfunctional metacognitive beliefs. Although our analyses found that there are no differences between instruments used, this can be explained for an evident lack of statistical power, which encourages further examination since research on the metacognitive model could benefit from the development of more diverse instruments considering the scarcity of metacognitive measures. In this sense, instruments avoiding words that refer to rumination and/or depression, such as the PBRS-A, are especially welcome. Fifth, while those studies that tested the metacognitive model used path analysis, it would be worth using structural equation model (SEM) analysis because this methodology minimizes measurement error. And lastly, few studies have examined the link between metacognitive beliefs and rumination and/or depression while controlling for other relevant variables that might influence these associations. Studies that control for rumination/depression-related constructs, such as anxiety levels or worry, are needed to confirm the specific hypothesis of the metacognitive model of rumination and depression.
The insights from the included studies, as well as their limitations, suggest several lines of research to fill gaps in the literature and extend current knowledge. Despite TSSEM results suggesting that the uncontrollability and harm subscale is the one most strongly associated with depression, further research is needed to clarify this issue. It is possible that a third variable may help to explain why metacognitive beliefs about the uncontrollability and harm subscale appear to be more important than the ones about social consequences. One possible moderator variable would be cognitive schemas. Beck (1983) identified two core cognitive schemas: (1) sociotropy schemas, which refer to an excessive value on close interpersonal relationships and social dependence; and (2) autonomy schemas, which reflect an investment in preserving independence and freedom. In this sense, we hypothesize that whereas metacognitive beliefs about social consequences of rumination are more relevant in predicting depression in individuals with high sociotropic schemas, metacognitive beliefs about the need to control thoughts in order to achieve that autonomy are more relevant for individuals higher in autonomy schemas. On the other hand, more research is needed to clarify the mechanism by which negative beliefs are linked to depression. The metacognitive model proposes that negative beliefs lead people to appraise their own rumination as uncontrollable and dangerous, thus increasing the accessibility to negative information (e.g., negative emotions or thoughts) and enhancing depressive symptomatology. However, it is possible that other variables mediate the associations between negative beliefs and depression. For example, people with negative beliefs about social consequences could be prone to use maladaptive strategies, such as emotional suppression, which in turn has social costs, whereas people with negative beliefs about uncontrollability and harm could be prone to use other maladaptive strategies that aim to stop or avoid their rumination, such alcohol or drug abuse. Research on the association between metacognitive beliefs and these and other emotion regulation strategies linked to depression (i.e., inactivity) may lead to a more complete understanding of the role of metacognitive beliefs in depression.
In conclusion, this review gathers the empirical evidence obtained for the metacognitive model of rumination and depression and highlights its relevance and utility. Increasing knowledge about the role of metacognitive beliefs in rumination and depression has clinical implications. Metacognitive therapy (MCT) seems to be a promising treatment for depression. The goals of this intervention are to promote a metacognitive model of thinking, enhance attentional resources through cognitive training, and modify metacognitive beliefs. More specifically, MTC suggests particular interventions to promote this metacognitive thinking mode, where the therapist explicitly teaches the patient how to induce and retain this type of processing. These techniques include, among others, metacognitive focused exposure, metacognitive experiments, meta-level discourse, free-association tasks, rumination postponement, and worry-modulation procedures. Therefore, these techniques, when used, increase the range, choice, and flexibility with which the patient can relate to inner thoughts, memories, and events. Full descriptions of these techniques can be found elsewhere (Wells, 2009). Research could improve this therapy by investigating what types of negative beliefs are most important to each individual, knowing in depth what processes are involved, and thus focusing treatment on the most relevant aspects.
References
Articles marked with an asterisk were included in the systematic review.
*Barahmand, U. (2008). Using metacognitions to identify emotionally vulnerable college students. American Journal of Health Behavior, 32(6), 604–613. https://doi.org/10.5993/ajhb.32.6.5.
Beck, A. T. (1983). Cognitive therapy of depression: New perspectives. In P.-J. Clayton & J. E. Barrett (Eds.), Treatment of depression: Old controversies and new approaches (pp. 265–290). Raven Press.
Beck, A. T., & Steer, R. A. (1987). Manual for the Beck Depression Inventory. The Psychological Corporation.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory: Manual (2nd ed.). The Psychological Corporation.
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. https://doi.org/10.1001/archpsyc.1961.01710120031004
Beshai, S., Dobson, K. S., Bockting, C. L., & Quigley, L. (2011). Relapse and recurrence prevention in depression: Current research and future prospects. Clinical Psychology Review, 31, 1349–1360. https://doi.org/10.1016/j.cpr.2011.09.003
Bieling, P. J., Antony, M. M., & Swinson, R. P. (1998). The state-trait anxiety inventory, trait version: Structure and content re-examined. Behaviour Research and Therapy, 36, 777–788. https://doi.org/10.1016/s0005-7967(98)00023-0
Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2009). Introduction to meta-analysis. Wiley.
Brinker, J. K., & Dozois, J. A. (2009). Ruminative thought style and depressed mood. Journal of Clinical Psychology, 65(1), 1–19. https://doi.org/10.1002/jclp.20542
*Cangas, A. J., Errasti, J. M., García-Montes, J. M., Álvarez, R., & Ruiz, R. (2006). Metacognitive factors and alterations of attention related to predisposition to hallucinations. Personality and Individual Differences, 40(3), 487–496. https://doi.org/10.1016/j.paid.2005.07.005.
Cartwright-Hatton, S., & Wells, A. (1997). Beliefs about worry and intrusions: The metacognitions questionnaire and its correlates. Journal of Anxiety Disorders, 11, 279–296. https://doi.org/10.1016/s0887-6185(97)00011-x
Cheung, M.W.-L. (2009). Constructing approximate confidence intervals for parameters with structural equation models. Structural Equation Modeling, 16, 267–294. https://doi.org/10.1080/10705510902751291
Cheung, M. W. L. (2015). metaSEM: An R package for meta-analysis using structural equation modeling. Frontiers in Psychology, 5, 1521. https://doi.org/10.3389/fpsyg.2014.01521
Cheung, M. W. L., & Chan, W. (2005). Meta-analytic structural equation modeling: A two-stage approach. Psychological Methods, 10, 40–64. https://doi.org/10.1037/1082-989X.10.1.40
Cooper, H., Hedges, L. V., & Valentine, J. C. (Eds.). (2019). The handbook of research synthesis and meta-analysis. Russell Sage Foundation.
De Castella, K., Platow, M. J., Tamir, M., & Gross, J. (2018). Beliefs about emotion: Implications for avoidance-based emotion regulation and psychological health. Cognition and Emotion, 32(4), 773–795. https://doi.org/10.1080/02699931.2017.1353485
*Dethier, V., Heeren, A., Bouvard, M., Baeyens, C., & Philippot, P. (2017). Embracing the structure of metacognitive beliefs: Validation of the French Short Version of the Metacognitions Questionnaire. International Journal of Cognitive Therapy, 10(3), 219–233. https://doi.org/10.1521/ijct.2017.10.3.219.
Egger, M., Davey-Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315, 629–634.
*Faissner, M., Kriston, L., Moritz, S., & Jelinek, L. (2018). Course and stability of cognitive and metacognitive beliefs in depression. Depression and Anxiety, 35(12), 1239–1246. https://doi.org/10.1002/da.22834.
*Gawęda, Ł., & Kokoszka, A. (2014). Meta-cognitive beliefs as a mediator for the relationship between Cloninger’s temperament and character dimensions and depressive and anxiety symptoms among healthy subjects. Comprehensive Psychiatry, 55(4), 1029–1037. https://doi.org/10.1016/j.comppsych.2013.10.013.
Goldberg, D. P., & Hillier, V. F. (1979). A scaled version of the General Health Questionnaire. Psychological Medicine, 9(1), 139–145. https://doi.org/10.1017/s0033291700021644
Hagen, R., Hjemdal, O., Solem, S., Kennair, L. E. O., Nordahl, H. M., Fisher, P., & Wells, A. (2017a). Metacognitive therapy for depression in adults: A waiting list randomized controlled trial with six months follow-up. Frontiers in Psychology, 8, 31. https://doi.org/10.3389/fpsyg.2017.00031
*Hagen, K., Solem, S., Opstad, H. B., Hansen, B., & Hagen, R. (2017b). The role of metacognition and obsessive-compulsive symptoms in psychosis: An analogue study. BMC, Psychiatry, 17, 233. https://doi.org/10.1186/s12888-017-1392-1.
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23(1), 56–62. https://doi.org/10.1136/jnnp.23.1.56
Higgins, J. P. T., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21, 1539–1558. https://doi.org/10.1002/sim.1186
Hjemdal, O., Hagen, R., Solem, S., Nordahl, H., Kennair, L. E. O., Ryum, T., Nordahl, H. N., & Wells, A. (2017). Metacognitive therapy in major depression: An open trial of comorbid cases. Cognitive and Behavioral Practice, 24(3), 312–318. https://doi.org/10.1016/j.cbpra.2016.06.006
Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. https://doi.org/10.1080/10705519909540118
*Huntley, C. D., & Fisher, P. L. (2016). Examining the role of positive and negative metacognitive beliefs in depression. Scandinavian Journal of Psychology, 57(5), 446–452. https://doi.org/10.1111/sjop.12306.
Johnson, D. P., & Whisman, M. A. (2013). Gender differences in rumination: A meta-analysis. Personality and Individual Differences, 55(4), 367–374. https://doi.org/10.1016/j.paid.2013.03.019
Joormann, J., & Quinn, M. E. (2014). Cognitive processes and emotion regulation in depression. Depression and Anxiety, 31(4), 308–315. https://doi.org/10.1002/da.22264
*Karatepe, H. T., Yavuz, F. K., & Turkcan, A. (2013). Validity and reliability of the Turkish version of the Ruminative Thought Style Questionnaire. Klinik Psikofarmakoloji Bülteni/Bulletin of Clinical Psychopharmacology, 23(3), 231–241. https://doi.org/10.5455/bcp.20121130122311
Kessler, R. C., & Bromet, E. J. (2013). The epidemiology of depression across cultures. Annual Review of Public Health, 9, 119–138. https://doi.org/10.1146/annurev-publhealth-031912-114409
*Kolubinski, D. C., Marino, C., Nikčević, A. V., & Spada, M. M. (2019). A metacognitive model of self-esteem. Journal of Affective Disorders, 256, 42–53. https://doi.org/10.1016/j.jad.2019.05.050
*Kraft, B., Jonassen, R., Ulset, V., Stiles, T., & Landrø, N. I. (2019). A prospective test of the metacognitive model of depression in previously depressed individuals. Cognitive Therapy and Research, 43, 603–610. https://doi.org/10.1007/s10608-018-9972-z
*Kubiak, T., Zahn, D., Siewert, K., Jonas, C., & Weber, H. (2014). Positive beliefs about rumination are associated with ruminative thinking and affect in daily life: Evidence for a metacognitive view on depression. Behavioural and Cognitive Psychotherapy, 42(5), 568–576. https://doi.org/10.1017/s1352465813000325
Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the depression, anxiety and stress scales (2nd ed.). Psychology Foundation.
Luca, M. (2019). Maladaptive rumination as a transdiagnostic mediator of vulnerability and outcome in psychopathology. Journal of Clinical Medicine, 8(3), 314. https://doi.org/10.3390/jcm8030314
Luminet, O. (2004). Measurement of depressive rumination and associated constructs. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination. Nature, theory and treatment (pp. 187–215). Chichester, England: Wiley.
Lyubomirsky, S., & Tkach, C. (2004). The consequences of dysphoric rumination. In C. Papageorgiou & A. Wells (Eds.), Depressive rumination: Nature, theory, and treatment (pp. 21–42). Wiley.
*Mahoney, A. E. J., Hobbs, M. J., Williams, A. D., Andrews, G., & Newby, J. M. (2018). The mediating relationship between maladaptive behaviours, cognitive factors, and generalised anxiety disorder symptoms. Behaviour Change, 35(2), 123–138. https://doi.org/10.1017/bec.2018.13
*Matsumoto, N., & Mochizuki, S. (2018). Why do people overthink? A longitudinal investigation of a meta-cognitive model and uncontrollability of rumination. Behavioural and Cognitive Psychotherapy, 46(4), 504–509. https://doi.org/10.1017/s1352465818000103
McEvoy, P. M., Mahoney, A. E., & Moulds, M. L. (2010). Are worry, rumination, and post-event processing one and the same? Development of the repetitive thinking questionnaire. Journal of Anxiety Disorders, 24, 509–519. https://doi.org/10.1016/j.janxdis.2010.03.008
*McEvoy, P. M., Moulds, M. L., & Mahoney, A. E. J. (2013). Mechanisms driving pre- and post-stressor repetitive negative thinking: Metacognitions, cognitive avoidance, and thought control. Journal of Behavior Therapy and Experimental Psychiatry, 44(1), 84–93. https://doi.org/10.1016/j.jbtep.2012.07.011
Mrazek, D. A., Hornberger, J. C., Altar, C. A., & Degtiar, I. (2014). A review of the clinical, economic and societal burden of treatment-resistant depression: 1996–2013. Psychiatric Services, 65, 977–987. https://doi.org/10.1176/appi.ps.201300059
Nolen-Hoeksema, S., & Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Preita earthquake. Journal of Personality and Social Psychology, 61, 115–121. https://doi.org/10.1037//0022-3514.61.1.115
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x
*Nordahl, H., Ødegaard, I. H., Hjemdal, O., & Wells, A. (2019). A test of the goodness of fit of the generic metacognitive model of psychopathology symptoms. BMC Psychiatry, 19(1), 288. https://doi.org/10.1186/s12888-019-2266-5
*Ophir, Y., & Mor, N. (2014). If I only knew why: The relationship between brooding, beliefs about rumination, and perceptions of treatments. Behavior Therapy, 45(4), 553–563. https://doi.org/10.1016/j.beth.2014.03.004
*Palmieri, S., Mansueto, G., Scaini, S., Fiore, F., Sassaroli, S., Ruggiero, G. M., Borlimi, R., & Carducci, B. J. (2018). Role of rumination in the relationship between metacognition and shyness. World Journal of Psychiatry, 8(4), 108–113. https://doi.org/10.5498/wjp.v8.i4.108
Papageorgiou, C., & Wells, A. (2001a). Metacognitive beliefs about rumination in recurrent major depression. Cognitive and Behavioral Practice, 8(2), 160–164. https://doi.org/10.1016/S1077-7229(01)80021-3
*Papageorgiou, C., & Wells, A. (2001b). Positive beliefs about depressive rumination: Development and preliminary validation of a self-report scale. Behavior Therapy, 32(1), 13–26. https://doi.org/10.1016/S0005-7894(01)80041-1.
*Papageorgiou, C., & Wells, A. (2003). An empirical test of a clinical metacognitive model of rumination and depression. Cognitive Therapy and Research, 27, 261–273. https://doi.org/10.1023/A:1023962332399.
Papageorgiou, C., & Wells, A. (2004). Depressive rumination: Nature, theory and treatment. Wiley.
*Papageorgiou, C., & Wells, A. (2009). A prospective test of the clinical metacognitive model of rumination and depression. International Journal of Cognitive Therapy, 2(2), 123–131. https://doi.org/10.1521/ijct.2009.2.2.123
Raes, F., Hermans, D., Williams, J. M. G., Bijttebier, P., & Eelen, P. (2008). A “triple W”-model of rumination on sadness: Why am I feeling sad, what’s the meaning of my sadness, and wish I could stop thinking about my sadness (but I can’t!). Cognitive Therapy and Research, 32, 526–541. https://doi.org/10.1007/s10608-007-9137-y
*Razavizadeh Tabadkan, B. B. Z., & Mohammadi Poor, M. (2016). Relationship between meta-cognitive beliefs and mindfulness with ruminative thoughts in students. International Journal of Mental Health and Addiction, 14(6), 1052–1056. https://doi.org/10.1007/s11469-016-9688-9
*Roelofs, J., Huibers, M., Peeters, F., Arntz, A., & van Os, J. (2010). Positive and negative beliefs about depressive rumination: A psychometric evaluation of two self-report scales and a test of a clinical metacognitive model of rumination and depression. Cognitive Therapy and Research, 34(2), 196–205. https://doi.org/10.1007/s10608-009-9244-z
*Roelofs, J., Papageorgiou, C., Gerber, R. D., Huibers, M., Peeters, F., & Arntz, A. (2007). On the links between self-discrepancies, rumination, metacognitions, and symptoms of depression in undergraduates. Behaviour Research and Therapy, 45, 1295–1305. https://doi.org/10.1016/j.brat.2006.10.005.
*Ruiz, F. J., & Odriozola-González, P. (2015). Comparing cognitive, metacognitive, and acceptance and commitment therapy models of depression: A longitudinal study survey. The Spanish Journal of Psychology, 18, E39. https://doi.org/10.1017/sjp.2015.31.
Rush, A. J., Gullion, C. M., Basco, M. R., Jarrett, R. B., & Trivedi, M. H. (1996). The inventory of depressive symptomatology (IDS): Psychometric properties. Psychological Medicine, 26(3), 477–486. https://doi.org/10.1017/S0033291700035558
Rush, A. J., Trivedi, H., Ibrahim, H., Carmody, T. J., Arnow, B., Klein, D. N., Markowitz, J. C., Ninan, P. T., Kornstein, S., Manber, R., Thase, M. E., Kocsis, J. H., & Keller, M. B. (2003). The 16-item Quick Inventory of Depressive Symptomatology (QIDS), Clinician Ratings (QIDS-R), and Self-Report (QIDS-DR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54, 573–583. https://doi.org/10.1016/S0006-3223(02)01866-8
*Sarisoy, G., Pazvantoğlu, O., Özturan, D. D., Ay, N. D., Yilman, T., Mor, S., Korkmaz, I. Z., Kaçar, Ö. F., & Gümüş, K. (2013). Metacognitive beliefs in unipolar and bipolar depression: A comparative study. Nordic Journal of Psychiatry, 68(4), 275–281. https://doi.org/10.3109/08039488.2013.814710.
*Solem, S., Hagen, R., Hoksnes, J. J., & Hjemdal, O. (2016). The metacognitive model of depression: An empirical test in a large Norwegian sample. Psychiatry Research, 242, 171–173. https://doi.org/10.1016/j.psychres.2016.05.056.
*Solem, S., Hagen, R., Wang, C. E. A., Hjemdal, O., Waterloo, K., Eisemann, M., & Halvorsen, M. (2015a). Metacognitions and mindful attention awareness in depression: A comparison of currently depressed, previously depressed and never depressed individuals. Clinical Psychology & Psychotherapy, 24(1), 94–102. https://doi.org/10.1002/cpp.1983
*Solem, S., Thunes, S. S., Hjemdal, O., Hagen, R., & Wells, A. (2015b). A metacognitive perspective on mindfulness: An empirical investigation. BMC Psychology, 3(1), 24. https://doi.org/10.1186/s40359-015-0081-4.
*Spada, M. M., Hiou, K., & Nikcevic, A. V. (2006). Metacognitions, emotions, and procrastination. Journal of Cognitive Psychotherapy, 20(3), 319–326. https://doi.org/10.1891/jcop.20.3.319.
*Spada, M. M., Langston, B., Nikčević, A. V., & Moneta, G. B. (2008a). The role of metacognitions in problematic Internet use. Computers in Human Behavior, 24(5), 2325–2335. https://doi.org/10.1016/j.chb.2007.12.002.
*Spada, M. M., Nikčević, A. V., Moneta, G. B., & Wells, A. (2008b). Metacognition, perceived stress, and negative emotion. Personality and Individual Differences, 44(5), 1172–1181. https://doi.org/10.1016/j.paid.2007.11.010.
*Spada, M. M., & Wells, A. (2005). Metacognitions, emotion and alcohol use. Clinical Psychology & Psychotherapy, 12(2), 150–155. https://doi.org/10.1002/cpp.431.
Spitzer, R. L., Kroenke, K., & Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Prime Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA, 282(18), 1737–1744. https://doi.org/10.1001/jama.282.18.1737
Sun, X., Zhu, C., & So, S. H. W. (2017). Dysfunctional metacognition across psychopathologies: A meta-analytic review. European Psychiatry, 45, 139–153. https://doi.org/10.1016/j.eurpsy.2017.05.029
*Tan, S., Moulding, R., Nedeljkovic, M., & Kyrios, M. (2010). Metacognitive, cognitive and developmental predictors of generalised anxiety disorder symptoms. Clinical Psychologist, 14(3), 84–89. https://doi.org/10.1080/13284207.2010.521521.
Thomas, L., Kessler, D., Campbell, J., Morrison, J., Peters, T. J., Williams, C., Lewis, C., & Wiles, N. (2013). Prevalence of treatment-resistant depression in primary care: Cross-sectional data. British Journal of General Practice, 63(617), E852–E858. https://doi.org/10.3399/bjgp13X675430
Treynor, W., Gonzalez, R., & Nolen-Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy Research, 27, 247–259. https://doi.org/10.1023/a:1023910315561
Trivedi, M. H., Rush, A. J., Ibrahim, H. M., Carmody, T. J., Biggs, M. M., Suppes, T., Crismon, M. L., Shores-Wilson, K., Toprac, M. G., Dennehy, E. B., & Witte, B. (2004). The inventory of depressive symptomatology clinician rating (IDS-C) and self-report (IDS-SR), and the quick inventory of depressive symptomatology, clinical rating (QIDS-C) and self-report (QIDS-SR) in public sector patients with mood disorders.: A psychometric evaluation. Psychological Medicine, 34, 73–82. https://doi.org/10.1017/S0033291703001107.
*Vassilopoulos, S. P., Brouzos, A., & Moberly, N. J. (2015). The relationships between metacognition, anticipatory processing, and social anxiety. Behaviour Change, 32(2), 114–126. https://doi.org/10.1017/bec.2015.4.
Viechtbauer, W. (2010). Conducting Meta-Analyses in R with the metafor Package. Journal of Statistical Software, 36, 1–48.
*Watkins, E., & Moulds, M. (2005). Positive beliefs about rumination in depression—a replication and extension. Personality and Individual Differences, 39(1), 73–82. https://doi.org/10.1016/j.paid.2004.12.006.
Watkins, E., & Roberts, H. (2020). Reflecting on rumination: Consequences, causes, mechanisms and treatment of rumination. Behaviour Research and Therapy, 127, 1–28. https://doi.org/10.1016/j.brat.2020.103573
*Weber, F. & Exner, C. (2013). Metacognitive beliefs and rumination: A longitudinal study. Cognitive Therapy and Research, 37(6), 1257–1261. https://doi.org/10.1007/s10608-013-9555-y
Wells, A. (2009). Metacognitive therapy for anxiety and depression. Guilford Press.
Wells, A. (2019). Breaking the cybernetic code: Understanding and treating the human metacognitive control system to enhance mental health. Frontiers in Psychology, 10, 2621. https://doi.org/10.3389/fpsyg.2019.02621
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42, 385–396. https://doi.org/10.1016/S0005-7967(03)00145-5
Wells, A., Fisher, P., Myers, S., Wheatley, J., Patel, T., & Brewin, C. R. (2009). Metacognitive therapy in recurrent and persistent depression: A multiple-baseline study of a new treatment. Cognitive Therapy and Research, 33(3), 291–300. https://doi.org/10.1007/s10608-007-9178-2
Wells, A., & Matthews, G. (1994). Attention and emotion: A clinical perspective. Lawrence Erlbaum Associates.
Wells, A., & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34, 881–888. https://doi.org/10.1016/S0005-7967(96)00050-2
Winter, L., Gottschalk, J., Nielsen, J., Wells, A., Schweiger, U., & Kahl, K. (2019). A comparison of metacognitive therapy in current versus persistent depressive disorder: A pilot outpatient study. Frontiers in Psychology, 10, 1714. https://doi.org/10.3389/fpsyg.2019.01714
*Yilmaz, A. E. (2016). Examination of the metacognitive model of depression in a Turkish university student sample. Turkish Journal of Psychiatry, 27(2), 1–9. https://doi.org/10.5080/u13505
*Yılmaz, A. E., Gençöz, T., & Wells, A. (2008). Psychometric characteristics of the Penn State Worry Questionnaire and Metacognitions Questionnaire-30 and metacognitive predictors of worry and obsessive-compulsive symptoms in a Turkish sample. Clinical Psychology & Psychotherapy, 15(6), 424–439. https://doi.org/10.1002/cpp.589.
Yılmaz, A. E., Gençöz, T., & Wells, A. (2011). The temporal precedence of metacognition in the development of anxiety and depression symptoms in the context of life-stress: A prospective study. Journal of Anxiety Disorders, 25(3), 389–396. https://doi.org/10.1016/j.janxdis.2010.11.001
*Yilmaz, A. E., Gençöz, T., & Wells, A. (2015). Unique contributions of metacognition and cognition to depressive symptoms. The Journal of General Psychology, 142(1), 23–33. https://doi.org/10.1080/00221309.2014.964658.
Zigmond, A. S., & Snaith, R. P. (1983). The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica, 67, 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Zimmerman, M., Coryell, W., Corenthal, C., & Wilson, S. (1986). A self-report scale to diagnose major depressive disorder. Archives of General Psychiatry, 43, 1076–1081. https://doi.org/10.1001/archpsyc.1986.01800110062008
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This study was part of a project funded by Spanish Government (Grant Number: PSI2017-83463-R).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Julia B. Cano-López, Esperanza García-Sancho, Belén Fernández-Castilla, and José M. Salguero have no competing interests.
Animal Rights
No animal studies were carried out by the authors for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cano-López, J.B., García-Sancho, E., Fernández-Castilla, B. et al. Empirical Evidence of the Metacognitive Model of Rumination and Depression in Clinical and Nonclinical Samples: A Systematic Review and Meta-Analysis. Cogn Ther Res 46, 367–392 (2022). https://doi.org/10.1007/s10608-021-10260-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-021-10260-2