Abstract
Tumor establishment, growth, and survival are supported by interactions with microenvironment components. Here, we investigated whether the interactions between prostate cancer cells and cortical astrocytes are associated to a potential role for astrocytes in tumor establishment. We demonstrate that astrocytes interact in vitro with prostatic cancers cells derived from different metastatic sites. Astrocytes and their secreted extracellular matrix, stimulate DU145 cell (a brain-derived prostate tumor cell line) proliferation while inhibiting cell death and modulating the expression of several genes related to prostate cancer progression, suggesting the activation of EMT process in these cells. In contrast, DU145 cells and their conditioned medium inhibited cell proliferation and induced cell death of astrocytes. On the other hand, the astrocytes were unable to significantly induce an increment of LNCaP cell (a lymph node-derived prostate tumor cell line) proliferative activity. In addition, LNCaP cells were also unable to induce cell death of astrocytes. Thus, we believe that DU145 cells, but not LNCaP cells, present an even more aggressive behavior when interacting with astrocytes. These results provide an important contribution to the elucidation of the cellular mechanisms involved in the brain microenvironment colonization.





Similar content being viewed by others
Abbreviations
- EMT:
-
Epithelial mesenchymal transition
- TGF-β:
-
Transforming growth factor beta
- CNS:
-
Central nervous system
- ECM:
-
Extracellular matrix
- FBS:
-
Fetal bovine serum
- 24-CM:
-
Conditioned medium collected after 24 h of culture
- 48-CM:
-
Conditioned medium collected after 48 h of culture
- PBS:
-
Phosphate buffered saline
- GFAP:
-
Glial fibrillary acidic protein
- CK:
-
Cytokeratin
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- V T :
-
Tangential velocity
- V S :
-
Spreading velocity
- MMP:
-
Matrix metalloproteinase
References
Chambers AF, Groom AC, MacDonald IC (2002) Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer 2:563–572
Grenader T, Shavit L, Lossus A, Pizov G, Wygoda M (2007) Brain metastasis: a rare initial presentation of prostate cancer. Int Urol Nephrol 39:537–539
Tremont-Lukats IW, Bobustuc G, Lagos GK, Lolas K, Kyritsis AP, Puduvalle VK (2003) Brain metastasis from prostate carcinoma: the M. D. Anderson Cancer Center experience. Cancer 2:363–368
McCutcheon IE, Eng DY, Logothetis CJ (1999) Brain metastasis from prostate carcinoma: antemortem recognition and outcome after treatment. Cancer 86:2301–2311
Deryugina EI, Quigley JP (2006) Matrix metalloproteinases and tumor metastasis. Cancer Metastasis Rev 25:9–34
Thiery JP, Acloque H, Huang RY, Nieto MA (2009) Epithelial-mesenchymal transitions in development and disease. Cell 139:871–890
Nieto MA (2011) The ins and outs of the epithelial to mesenchymal transition in health and disease. Annu Rev Cell Dev Biol 27:347–376
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Russel JP, Bennett S, Stricker P (1998) Growth factor involvement in progression of prostate cancer. Clin Chem 44(4):705–723
Lee SJ, Benveniste N (1999) Adhesion molecule expression and regulation on cells of the central nervous system. J Neuroimmunol 98(2):77–88
Gomes FC, Spohr TC, Martinez R, Moura-Neto V (2001) Cross-talk between neurons and glia: highlights on soluble factors. Braz J Med Biol Res 34:611–620
Taylor AR, Robinson MB, Gifondorwa DJ, Tytell M, Milligan CE (2007) Regulation of heat shock protein 70 release in astrocytes: role of signaling kinases. Dev Neurobiol 67:1815–1829
Cornell RJ, Rowley D, Wheeler T, Ali N, Ayala G (2003) Neuroepithelial Interactions in prostate cancer are enhanced in the presence of prostatic stroma. Urulogy 61(4):870–875
Trentin AG, Moura-Neto V (1995) T3 affects cerebellar astrocyte proliferation, GFAP and fibronectin organization. NeuroRep 2:293–296
Lima FRS, Arantes CP, Muras AG, Nomizo R, Brentani R, Martins VR (2007) Cellular prion protein expression in astrocytes modulates neuronal survival and differentiation. J Neurochem 103:2164–2176
Er HM, Cheng EH, Radhakrishnan AK (2007) Anti-proliferative and mutagenic activities of aqueous and methanol extracts of leaves from Pereskia bleo (Kunth) DC (Cactaceae). J Ethnopharmacol 113(3):448–456
Palumbo A, Ferreira LB, Souza PR, Oliveira FL, Pontes B, Vianna NB, Machado DE, Palmero CY, Miranda-Alves L, Gimba E, Nasciutti LE (2012) Extracellular matrix secreted by reactive stroma is a main inducer of pro-tumorigenic features on LNCaP prostate cancer cells. Cancer Lett 321:55–64
Christiansen JJ, Rajasekaran AK (2006) Reassessing epithelial to mesenchymal transition as a prerequisite for carcinoma invasion and metastasis. Cancer Res 66(17):8319–8326
Erasmus CE, Verhagen WIM, Wauters CAP, Van Lindert EJ (2002) Brain metastasis from prostate small cell carcinoma: not to be neglected. Can J Neurol Sci 29:375–377
Iacopino F, Angelucci C, Sica G (2012) Interactions between normal human fibroblasts and human prostate cancer cells in a co-culture system. Anticancer Res 32:1579–1588
Stone KR, Mickey DD, Wunderlli H, Mickey GH, Paulson DF (1978) Isolation of a human prostate carcinoma cell line (DU145). Int J Cancer 21:274–281
Coulson-Thomas VJ, Gesteira TF, Coulson-Thomas YM, Vicente CM, Tersariol IL, Nader HB, Toma L (2010) Fibroblast and prostate tumor cell cross-talk: fibroblast differentiation, TGF-β, and extracellular matrix down-regulation. Exp Cell Res 316(19):3207–3226
Yamaguchi H, Condeelis J (2007) Regulation of the actin cytoskeleton in cancer cell migration and invasion. Biochim Biophys Acta 1773:642–652
Nabeshima K, Inoue T, Shimao Y (1999) Cohort migration of carcinoma cells: differentiated colorectal carcinoma cells move as coherent cell clusters or sheets. Histol Histopathol 14:1183–1197
Nabeshima K, Inoue T, Shimao Y (2000) Front-cell specific expression of membrane-type 1 matrix metalloproteinase and gelatinase A during cohort migration of colon carcinoma cells induced by hepatocyte growth factor/scatter factor. Cancer Res 60:3364–3369
Friedl P, Noble PB, Walton PA (1995) Migration of coordinated cell clusters in mesenchymal and epithelial cancer explants in vitro. Cancer Res 55:4557–4560
Friedl P, Wolf K (2003) Tumour-cell invasion and migration: diversity and escape mechanisms. Nat Rev Cancer 3:362–374
Lee JM, Dedhar S, Kalluri R, Thompson EW (2006) The epithelial-mesenchymal transition: new insights in signaling, development, and disease. J Cell Biol 172:973–981
Chen PS, Shih YW, Huang HC, Cheng HW (2011) Diosgenin, a steroidal saponin, inhibits migration and invasion of human prostate cancer PC-3 cells by reducing matrix metalloproteinases expression. PLoS ONE 6(5):e20164
Drobnjak M, Osman I, Scher HI (2000) Overexpression of cyclin D1 is associated with metastatic prostate cancer to bone. Clin Cancer Res 6(5):1891–1895
Adams JM, Cory S (2007) The Bcl-2 apoptotic switch in cancer development and therapy. Oncogene 26:1324–1337
Lang SH, Hyde C, Reid IN (2002) Enhanced expression of vimentin in motile prostate cell lines and in poorly differentiated and metastatic prostate carcinoma. Prostate 52:253–263
Eklov S, Funa K, Nordgen H, Olofsson A, Kanzaki T, Miyazono K, Nilsson S (1993) Lack of the latent transforming growth factor beta binding protein in malignant but not benign prostatic tissue. Cancer Res 53:3193–3197
Mingfang AO, Franco OE, Park D, Raman D, Williams K, Hayward SW (2007) Cross-talk between paracrine acting cytokine and chemokine pathways promotes malignancy in benign human prostatic epithelium. Cancer Res 67:4244–4253
Sharifi N, Lechleider RJ, Farrar WL (2007) Transforming growth factor-beta receptor III downregulation in prostate cancer: is inhibin B a tumor suppressor in prostate? J Mol Endocrinol 39:329–332
Acknowledgments
The authors thank Dr. Vivaldo Moura Neto for discussion and comments on the study; Dr. Jane Faria and Morgana Ferreira Sobrinho for the encouragement; and Maria Aparecida de Oliveira Domingos and Grasiella Ventura for technical assistance. This work was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Tecnológico (CNPq), and Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ).
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10585_2014_9640_MOESM1_ESM.tif
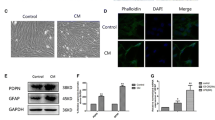
Electronic Supplementary Material Fig. 1 Characterization by immunofluorescence and cell proliferation and cell death analysis of astrocytes and LNCaP cells in co-culture. (A)The cells were incubated for 24 and 48 h in medium supplemented with 0.5 FBS, and immunostained with anti-GFAP and human anti-cytokeratin. The astrocytes (red) LNCaP cells (white). In co-culture, LNCaP cells formed small clusters arranged over the astrocytes monolayer. (B) Quantification of cell number present in co-culture by flow cytometry. (C) TUNEL assay performed in co-culture of astrocytes and LNCaP cells. DAPI (blue), nuclei staining. Scale bar, 200 µm (TIFF 5792 kb)
10585_2014_9640_MOESM2_ESM.tif
Electronic Supplementary Material Fig. 2 Cell viability analysis of astrocytes and DU145 cells isolated and in co-culture. Cell viability was measured by the MTT colorimetric assay after 24 (A) and 48 (B) h of culture in supplemented medium with 10 %, 0.5 %, and without FBS. Note that after 48 h in 0.5 % FBS, the viability of astrocytes begins to be rescue. The results are expressed as the means ± CI of three independent experiments. CI = confidence interval. (*)p < 0.05, (**) p < 0.01, (***) p < 0.001 (TIFF 2144 kb)
10585_2014_9640_MOESM3_ESM.tif
Electronic Supplementary Material Fig. 3 Schematic model of co-culture and cell sorting. (A) Schematic model of co-culture of astrocytes labeled with Green CMFDA and unlabeled DU145 cells. (B) Separation of cells by flow cytometry. Note that there are differences in fluorescence emission peaks of labeled astrocytes and unlabeled DU145 cells (TIFF 2228 kb)
Supplementary material 4 (MPG 1378 kb)
Rights and permissions
About this article
Cite this article
de Oliveira Barros, E.G., Palumbo, A., Mello, P.L.P. et al. The reciprocal interactions between astrocytes and prostate cancer cells represent an early event associated with brain metastasis. Clin Exp Metastasis 31, 461–474 (2014). https://doi.org/10.1007/s10585-014-9640-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-014-9640-y