Abstract
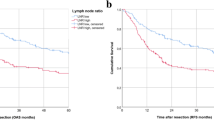
Overexpression of members of the ErbB receptor family is common in oral squamous cell carcinomas (OSCC); however, their prognostic value for aggressive OSCC has been debated. Extranodal spread to cervical lymph nodes is the most significant prognostic indicator in OSCC. In the present study, we investigated the clinical significance of single versus paired overexpression of members of the ErbB receptor family in 82 OSCC patients with lymph nodes metastasis, with or without capsular rupture (CR) followed by at least 10 years. Immunohistochemistry analysis revealed a common overexpression of ErbB1 (P = 0.021), ErbB2 (P = 0.001), ErbB4 (P = 0.048), as well as MMP-2 (P = 0.043) in OSCC cases with CR+. Increased expression of ErbB1 was associated with MMP-2 in tumors with advanced clinical stages, including poorly differentiated (grade III) tumors (P < 0.050). Vascular embolization was associated with MMP-2 (P = 0.021) and MMP-13 (P = 0.010) overexpression. Survival analysis revealed a lower survival probability in tumors overexpressing ErbB1 (P = 0.038), ErbB4 (P = 0.043), and MMP-12 (P = 0.050). As well a strong association was observed in cases with high risk of recurrence and strong immunostaining for ErbB1 (P = 0.017), ErbB4 (P = 0.008), MMP-1 (P = 0.003), MMP-2 (P = 0.016), MMP-10 (P = 0.041), and MMP-13 (P = 0.005). Stratified multivariate survival analysis revealed a strong prognostic interdependence of ErbB1 and ErbB4 cooverexpression in predicting the worst overall and disease-free survivals (P = 0.0013 and P = 0.0004, respectively). Taken together, these results support a cooperation of ErbB1, ErbB4, and members of the MMP family in predicting OSCC invasion and poor clinical outcomes.


Similar content being viewed by others
References
Curado MP, Hashibe M (2009) Recent changes in the epidemiology of head and neck cancer. Curr Opin Oncol 21:194–200
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Hardisson D (2003) Molecular pathogenesis of head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol 260:502–508
Cojocariu OM, Huguet F, Lefevre M, Périé S (2009) Prognosis and predictive factors in head-and-neck cancers. Bull Cancer 96:369–378
Choi S, Myers JN (2008) Molecular pathogenesis of oral squamous cell carcinoma: implications for therapy. J Dent Res 87:14–32
Takes RP, Rinaldo A, Silver CE, Piccirillo JF, Haigentz M Jr, Suárez C, Van der Poorten V, Hermans R, Rodrigo JP, Devaney KO, Ferlito A (2010) Future of the TNM classification and staging system in head and neck cancer. Head Neck 32:1693–1711
Gospodarowicz MK, Miller D, Groome PA, Greene FL, Logan PA, Sobin LH (2004) The process for continuous improvement of the TNM classification. Cancer 100:1–5
Greene FL (2002) The American Joint Committee on Cancer: updating the strategies in cancer staging. Bull Am Coll Surg 87:13–15
Kowalski LP, Sanabria A (2007) Elective neck dissection in oral carcinoma: a critical review of the evidence. Acta Otorhinolaryngol Ital 27:113–117
Shaw RJ, Lowe D, Woolgar JA, Brown JS, Vaughan ED, Evans C, Lewis-Jones H, Hanlon R, Hall GL, Rogers SN (2010) Extracapsular spread in oral squamous cell carcinoma. Head Neck 32:714–722
Rosenthal EL, Matrisian LM (2006) Matrix metalloproteases in head and neck cancer. Head Neck 28:639–648
Greenberg JS, Fowler R, Gomez J, Mo V, Roberts D, El Naggar AK, Myers JN (2003) Extent of extracapsular spread: a critical prognosticator in oral tongue cancer. Cancer 97:1464–1470
Silva SD, Cunha IW, Nishimoto IN, Soares FA, Carraro DM, Kowalski LP, Graner E (2009) Clinicopathological significance of ubiquitin-specific protease 2a (USP2a), fatty acid synthase (FASN), and ErbB2 expression in oral squamous cell carcinomas. Oral Oncol 45:e134–e139
Silva SD, Cunha IW, Rangel AL, Jorge J, Zecchin KG, Agostini M, Kowalski LP, Coletta RD, Graner E (2008) Differential expression of fatty acid synthase (FAS) and ErbB2 in nonmalignant and malignant oral keratinocytes. Virchows Arch 453:57–67
Lafky JM, Wilken JA, Baron AT, Maihle NJ (2008) Clinical implications of the ErbB/epidermal growth factor (EGF) receptor family and its ligands in ovarian cancer. Biochim Biophys Acta 1785:232–265
Syrigos KN, Zalonis A, Kotteas E, Saif MW (2008) Targeted therapy for oesophageal cancer: an overview. Cancer Metastasis Rev 27:273–288
Wei Q, Sheng L, Shui Y, Hu Q, Nordgren H, Carlsson J (2008) EGFR, HER2, and HER3 expression in laryngeal primary tumors and corresponding metastases. Ann Surg Oncol 5:1193–1201
Kassouf W, Black PC, Tuziak T, Bondaruk J, Lee S, Brown GA, Adam L, Wei C, Baggerly K, Bar-Eli M, McConkey D, Czerniak B, Dinney CP (2008) Distinctive expression pattern of ErbB family receptors signifies an aggressive variant of bladder cancer. J Urol 179:353–358
Silva SD, Agostini M, Nishimoto IN, Coletta RD, Alves FA, Lopes MA, Kowalski LP, Graner E (2004) Expression of fatty acid synthase, ErbB2 and Ki-67 in head and neck squamous cell carcinoma. A clinicopathological study. Oral Oncol 40:688–696
Marcu LG, Yeoh E (2009) A review of risk factors and genetic alterations in head and neck carcinogenesis and implications for current and future approaches to treatment. J Cancer Res Clin Oncol 135:1303–1314
Zhang H, Berezov A, Wang Q, Zhang G, Drebin J, Murali R, Greene MI (2007) ErbB receptors: from oncogenes to targeted cancer therapies. J Clin Invest 117:2051–2058
Holbro T, Civenni G, Hynes NE (2003) The ErbB receptors and their role in cancer progression. Exp Cell Res 284:99–110
O-charoenrat P, Rhys-Evans PH, Modjtahedi H, Eccles SA (2002) The role of c-erbB receptors and ligands in head and neck squamous cell carcinoma. Oral Oncol 38:627–640
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100:57–70
Zeren T, Inan S, Seda Vatansever H, Ekerbicer N, Sayhan S (2008) Significance of tyrosine kinase activity on malign transformation of ovarian tumors: a comparison between EGF-R and TGF-alpha. Acta Histochem 110:256–263
Pu J, McCaig CD, Cao L, Zhao Z, Segall JE, Zhao M (2007) EGF receptor signalling is essential for electric-field-directed migration of breast cancer cells. J Cell Sci 120:3395–3403
Klapper LN, Kirschbaum MH, Sela M, Yarden Y (2000) Biochemical and clinical implications of the ErbB/HER signaling network of growth factor receptors. Adv Cancer Res 77:25–79
Penuel E, Schaefer G, Akita RW, Sliwkowski MX (2001) Structural requirements for ErbB2 transactivation. Semin Oncol 28:36–42
Riese DJ 2nd, Stern DF (1998) Specificity within the EGF family/ErbB receptor family signaling network. BioEssays 20:41–48
Olayioye MA, Neve RM, Lane HA, Hynes NE (2000) The ErbB signaling network: receptor heterodimerization in development and cancer. EMBO J 19:3159–3167
Yarden Y, Sliwkowski MX (2001) Untangling the ErbB signalling network. Nat Rev Mol Cell Biol 2:127–137
O’Sullivan B, Shah J (2003) New TNM staging criteria for head and neck tumors. Semin Surg Oncol 21:30–42
Wahi PN, Cohen B, Luthra UK, Torloni H (1971) Histological typing of oral and oropharyngeal tumours. World Health Organization, Geneva 28
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, van de Vijver M, Wheeler TM, Hayes DF (2007) American Society of Clinical Oncology/College of American Pathologists. merican Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 131:18–43
Kononen J, Bubendorf L, Kallioniemi A, Bärlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP (1998) Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med 4:844–847
Geiger TR, Peeper DS (2009) Metastasis mechanisms. Biochim Biophys Acta 1796:293–308
Alaoui-Jamali MA, Song DJ, Benlimame N, Yen L, Deng X, Hernandez-Perez M, Wang T (2003) Regulation of multiple tumor microenvironment markers by overexpression of single or paired combinations of ErbB receptors. Cancer Res 63:3764–3774
Muraoka-Cook RS, Feng SM, Strunk KE, Earp HS 3rd (2008) ErbB4/HER4: role in mammary gland development, differentiation and growth inhibition. J Mammary Gland Biol Neoplasia 13:235–246
Ortega MC, Bribián A, Peregrín S, Gil MT, Marín O, de Castro F (2012) Neuregulin-1/ErbB4 signaling controls the migration of oligodendrocyte precursor cells during development. Exp Neurol 235:610–620
Olayioye MA, Graus-Porta D, Beerli RR, Rohrer J, Gay B, Hynes NE (1998) ErbB-1 and ErbB-2 acquire distinct signaling properties dependent upon their dimerization partner. Mol Cell Biol 18:5042–5051
Clark DE, Williams CC, Duplessis TT, Moring KL, Notwick AR, Long W, Lane WS, Beuvink I, Hynes NE, Jones FE (2005) ErbB4/HER4 potentiates STAT5A transcriptional activity by regulating novel STAT5A serine phosphorylation events. J Biol Chem 280:24175–24180
Salcini AE, McGlade J, Pelicci G, Nicoletti I, Pawson T, Pelicci PG (1994) Formation of Shc-Grb2 complexes is necessary to induce neoplastic transformation by overexpression of Shc proteins. Oncogene 9:2827–2836
Xu J, Rodriguez D, Petitclerc E, Kim JJ, Hangai M, Moon YS, Davis GE, Brooks PC (2001) Proteolytic exposure of a cryptic site within collagen type IV is required for angiogenesis and tumor growth in vivo. J Cell Biol 154:1069–1079
Giannelli G, Falk-Marzillier J, Schiraldi O, Stetler-Stevenson WG, Quaranta V (1997) Induction of cell migration by matrix metalloprotease-2 cleavage of laminin-5. Science 277:225–228
Ke Z, Lin H, Fan Z, Cai TQ, Kaplan RA, Ma C, Bower KA, Shi X, Luo J (2006) MMP-2 mediates ethanol-induced invasion of mammary epithelial cells over-expressing ErbB2. Int J Cancer 119:8–16
Kim IY, Yong HY, Kang KW, Moon A (2009) Overexpression of ErbB2 induces invasion of MCF10A human breast epithelial cells via MMP-9. Cancer Lett 275:227–233
Bao W, Fu HJ, Jia LT, Zhang Y, Li W, Jin BQ, Yao LB, Chen SY, Yang AG (2010) HER2-mediated upregulation of MMP-1 is involved in gastric cancer cell invasion. Arch Biochem Biophys 499:49–55
Aglund K, Rauvala M, Puistola U, Angström T, Turpeenniemi-Hujanen T, Zackrisson B, Stendahl U (2004) Gelatinases A and B (MMP-2 and MMP-9) in endometrial cancer-MMP-9 correlates to the grade and the stage. Gynecol Oncol 94:699–704
Dutton JM, Graham SM, Hoffman HT (2002) Metastatic cancer to the floor of mouth: the lingual lymph nodes. Head Neck 24:401–405
Davidson B, Goldberg I, Gotlieb WH, Kopolovic J, Ben-Baruch G, Nesland JM, Berner A, Bryne M, Reich R (1999) High levels of MMP-2, MMP-9, MT1-MMP and TIMP-2 mRNA correlate with poor survival in ovarian carcinoma. Clin Exp Metastasis 17:799–808
Patel BP, Shah SV, Shukla SN, Shah PM, Patel PS (2007) Clinical significance of MMP-2 and MMP-9 in patients with oral cancer. Head Neck 29:564–572
Yorioka CW, Coletta RD, Alves F, Nishimoto IN, Kowalski LP, Graner E (2002) Matrix metalloproteinase-2 and -9 activities correlate with the disease-free survival of oral squamous cell carcinoma patients. Int J Oncol 20:189–194
Köhrmann A, Kammerer U, Kapp M, Dietl J, Anacker J (2009) Expression of matrix metalloproteinases (MMPs) in primary human breast cancer and breast cancer cell lines: new findings and review of the literature. BMC Cancer 9:188
Acknowledgments
This work was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP 06/61039-8 and CEPID/FAPESP 98/14335). Silva SD was supported by a FAPESP fellowship (06/61040-6). The authors would like to acknowledge José Ivanildo Neves, Carlos Ferreira Nascimento, and Severino Ferreira for their technical assistance.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Silva, S.D., Alaoui-Jamali, M.A., Hier, M. et al. Cooverexpression of ERBB1 and ERBB4 receptors predicts poor clinical outcome in pN+ oral squamous cell carcinoma with extranodal spread. Clin Exp Metastasis 31, 307–316 (2014). https://doi.org/10.1007/s10585-013-9629-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-013-9629-y