Abstract
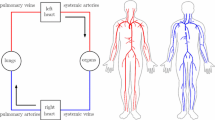
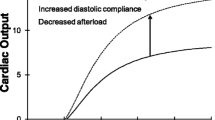
We upgraded our human cardiopulmonary (CP) model with additional data that enables it to more accurately simulate normal physiology. We then tested its ability to explain human disease by changing two parameter values that decrease ventricular compliance, and found that it could predict many of the hemodynamic, gas exchange, and autonomic abnormalities found in patients with left ventricular diastolic dysfunction (LVDD). The newly incorporated information includes high-fidelity pressure tracings simultaneously recorded from the RV and LV of a normal human in a cardiac catheterization laboratory, Doppler echocardiographic inlet flow velocity patterns, measures of right and left ventricular impedance, and atrial volumes. The revised cardiovascular section details the hemodynamics of a normal subject to the extent that it can now explain the effects of septal compliance on ventricular interaction, the differences in left and right ventricular pressure development, and venous blood gas mixing in the right atrium. The model can isolate the highly interrelated features of normal and abnormal physiology, and simultaneously demonstrate their interaction in a manner that would be very difficult or impossible using an intact organism. It may therefore help physicians and scientists understand, diagnose, and improve their treatment of complicated cardiovascular and pulmonary diseases. It could also simulate the hemodynamic and respiratory effects of ventricular and pulmonary assist devices, and thus help with their development.















Similar content being viewed by others
References
Batzel JJ, Kappel F, Timischl-Teschl S. A cardiovascular-respiratory control system model including state delay with application to congestive heart failure in humans. J Math Biol 2005;50:293–335
Blasi A, Jo JA, Valladares E, Juarez R, Baydur A, Khoo MC. Autonomic cardiovascular control following transient arousal from sleep: a time-varying closed-loop model. IEEE Trans Biomed Eng 2006;53:74–82
Boyd HL, Rosen SD, Rimoldi O, Cunningham VJ, Camici PG. Normal values for left ventricular volumes obtained using gated PET. G Ital Cardiol 1998;28:1207–14
Cash JR, Karp AH. A variable order Runge-Kutta method for initial value problems with rapidly varying right-hand sides. ACM Trans Math Soft 1990;16:201–22
Couture P, Denault AY, Sheridan P, Williams S, Cartier R. Partial inferior vena cava snaring to control ischemic left ventricular dysfunction. Can J Anesth 2003;50:404–10
Firstenberg MS, Greenberg NL, Smedira NG, Prior DL, Scalia GM, Thomas JD, Garcia MJ. Doppler echo evaluation of pulmonary venous-left atrial pressure gradients: human and numerical model studies. AJP – Heart 2000;279:594–600
Graham TP, Atwood GF, Faulkner SL, Nelson JH. Right atrial volume measurements from biplane cineangiocardiography: methodology, normal values, and alterations with pressure or volume overload. Circulation 1974;49:709–16
Gutierrez C, Blanchard DG. Diastolic heart failure: challenges of diagnosis and treatment. Am Fam Phys 2004;69:2609–16
Hamlin SK, Villars PS, Kanusky JT, Shaw AD. Role of diastole in left ventricular function, II: diagnosis and treatment. Am J Critical Care 2004;13:453–68
Izumi C, Iga K, Himura Y, Gen H, Konishi T. Influence of gravity on pulmonary venous flow velocity patterns: analysis of left and right pulmonary venous flow velocities in left and right decubitus positions. Am Heart J 1999;137:419–26
Kawaguchi M, Hay I, Fetics B, Kass DA. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation 2003;107:714–20
Lu K, Clark JW, Ghorbel FH, Ware DL, Bidani A. A human cardiopulmonary system model applied to the analysis of the Valsalva maneuver. Am J Physiol Heart Circ Physiol 2001;281:H2661–79
Lu K, Clark JW, Ghorbel FH, Ware DL, Zwischenberger JB, Bidani A. Whole-body gas exchange in human predicted by a cardiopulmonary model. J Cardiovasc Eng 2003;3:1–19
Lu K, Clark JW, Ghorbel FH, Robertson CS, Ware DL, Zwischenberger JB, Bidani A. Cerebral autoregulation and gas exchange studied with a human cardiopulmonary model. Am J Physiol 2004;286:H584–H601
Magosso E, Ursino M. Modeling study of the acute cardiovascular response to hypocapnic hypoxia in healthy and anemic subjects. Med Biol Eng Comput 2004;42:158–66
Mandinov L, Eberli FR, Seiler C, Hess OM. Diastolic heart failure. Cardiovasc Res 2000;45:813–25
Murgo JP, Westerhof N, Giolma JP, Altobelli SA. Aortic input impedance in normal man: relationship to pressure wave forms. Circulation Res 1980;62:105–16
Murgo JP, Westerhof N. Input impedance of the pulmonary arterial system in normal man: effects of respiration and comparison to systemic impedance. Circulation Res 1984;54:666–73
Press WH, Teukolsky SA, Plannery BP. Numerical recipe in C: the art of scientific computing, 2nd ed. Cambridge, UK: Cambridge University Press, 1992, p. 710–22
Rideout VC. Mathematical and Computer Modeling of Physiological Systems. Medical Physics Publishing, 732 N. Midvale Blvd, Madison, WI, 1991
Sandstede J, Lipke C, Beer M, Hofmann S, Pabst T, Kenn W, Neubauer S, Hahn D. Age- and gender-specific differences in left and right ventricular cardiac function and mass determined by cine magnetic resonance imaging. Eur Radiol 2000;10:438–42
Tsang TSM, Barnes ME, Gersh BJ, Bailey KR, Seward JB. Left Atrial Volume as a Morphophysiologic Expression of Left Ventricular Diastolic Dysfunction and Relation to Cardiovascular Risk Burden. Am J Cardiol 2002;90:1284–9
Valentine AL, Pope J, Read T. Evaluation of left atrial size and pressure as it relates to left ventricle diastolic measurements in patients with left ventricle hypertrophy. JDMS 2003;19:73–9
Vasan RS, Levy D. Defining diastolic heart failure: a call for standardized diagnostic criteria. Circulation; 2000 101:2118–21
Yalcin F, Thomas J. Diastolic dysfunction: pathogenesis, therapy and the importance of Doppler echocardiography. Turk J Med Sci; 1999:29:501–5
Acknowledgements
The authors would like to thank Dr. Bernie Rubal for his many helpful suggestions, the Cardiology Service at Brooke Army Medical Center and Millar Instruments, Inc. Houston, TX for access to the high fidelity pressure data from their collaborative research project (0104-T-C963).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luo, C., Ware, D.L., Zwischenberger, J.B. et al. Using a Human Cardiopulmonary Model to Study and Predict Normal and Diseased Ventricular Mechanics, Septal Interaction, and Atrio-Ventricular Blood Flow Patterns. Cardiovasc Eng 7, 17–31 (2007). https://doi.org/10.1007/s10558-007-9025-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10558-007-9025-9