Abstract
Background
Patients with chronic kidney disease (CKD) are at high risk for developing cardiovascular events. However, limited evidence is available regarding the use of aspirin in CKD patients to decrease cardiovascular risk and to slow renal disease progression.
Study Design
Prospective, multicenter, open-label randomized controlled trial.
Setting and Participants
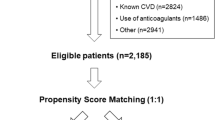
One hundred eleven patients with estimated glomerular filtration rate (eGFR) 15–60 ml/min/1.73 m2 without previous cardiovascular events.
Intervention
Aspirin treatment (100 mg/day) (n = 50) or usual therapy (n = 61). Mean follow-up time was 64.8 ± 16.4 months.
Outcomes
The primary endpoint was composed of cardiovascular death, acute coronary syndrome (nonfatal MI, coronary revascularization, or unstable angina pectoris), cerebrovascular disease, heart failure, or nonfatal peripheral arterial disease. Secondary endpoints were fatal and nonfatal coronary events, renal events (defined as doubling of serum creatinine, ≥ 50% decrease in eGFR, or renal replacement therapy), and bleeding episodes.
Results
During follow-up, 17 and 5 participants suffered from a primary endpoint in the control and aspirin groups, respectively. Aspirin did not significantly reduce primary composite endpoint (HR, 0.396 (0.146–1.076), p = 0.069. Eight patients suffered from a fatal or nonfatal coronary event in the control group compared to no patients in the aspirin group. Aspirin significantly reduced the risk of coronary events (log-rank, 5.997; p = 0.014). Seventeen patients in the control group reached the renal outcome in comparison with 3 patients in the aspirin group. Aspirin treatment decreased renal disease progression in a model adjusted for age, baseline kidney function, and diabetes mellitus (HR, 0.272; 95% CI, 0.077–0.955; p = 0.043) but did not when adjusted for albuminuria. No differences were found in minor bleeding episodes between groups and no major bleeding was registered.
Limitations
Small sample size and open-label trial.
Conclusions
Long-term treatment with low-dose aspirin did not reduce the composite primary endpoint; however, there were reductions in secondary endpoints with fewer coronary events and renal outcomes. ClinicalTrials.gov Identifier: NCT01709994.



Similar content being viewed by others
References
Miner J, Hoffhines A. The discovery of aspirin’s antithrombotic effects. Tex Heart Inst J. 2007;34(2):179–86.
Violi F, Targher G, Vestri A, Carnevale R, Averna M, Farcomeni A, et al. Background effect of aspirin on renal disease progression in patients with type 2 diabetes: a multicenter, double-blind, placebo-controlled, randomized trial. The renaL disease progression by aspirin in diabetic patients (LEDA) trial. Rationale and study design. Am Heart J. 2017;189:120–7.
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–47.
Mathew RO, Bangalore S, Lavelle MP, Pellikka PA, Sidhu MS, Boden WE, et al. Diagnosis and management of atherosclerotic cardiovascular disease in chronic kidney disease: a review. Kidney Int. 2017;91:797–807.
Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative metaanalysis of individual participant data from randomised trials. Lancet. 2009;373:1849–60.
US Food and Drug Administration. Information for consumers (drugs): use of aspirin for primary prevention of heart attack and stroke. Available at: https:// www.fda.gov/Drugs/ResourcesForYou/Consumers/ucm390574.htm. Accessed 17 Mar 2017.
Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: recommendations from the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(12):836–45.
Charytan D, Kuntz RE. The exclusion of patients with chronic kidney disease from clinical trials in coronary artery disease. Kidney Int. 2006;70:2021–30.
Palmer SC, Di Micco L, Razavian M, et al. Effects of antiplatelet therapy on mortality and cardiovascular and bleeding outcomes in persons with chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med. 2012;156:445–59.
Desai D, Ahmed HM, Michos ED. Preventing cardiovascular disease in patients with diabetes: use of aspirin for primary prevention. Curr Cardiol Rep. 2015;17(3):566.
Weigert AL, Schafer AI. Uremic bleeding: pathogenesis and therapy. Am J Med Sc. 1998;316:94–104.
Lenderink T, Boersma E, Ruzyllo W, GUSTO IV-ACS Investigators, et al. Bleeding events with abciximab in acute coronary syndromes without early revascularization: an analysis of GUSTO IV-ACS. Am Heart J. 2004;147(5):865–73.
Guirguis-Blake JM, Evans CV, Senger CA, O'Connor EA, Whitlock EP. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(12):804–13.
Cedeño Mora S, Goicoechea M, Torres E, Verdalles Ú, Pérez de José A, Verde E, et al. Cardiovascular risk prediction in chronic kidney disease patients. Nefrologia. 2017;37(3):293–300.
Peto R, Gray R, Collins R, Wheatley K, Hennekens C, Jamrozik K, et al. Randomised trial of prophylactic daily aspirin in British male doctors. Br Med J (Clin Res Ed). 1988;296(6618):313–6.
Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med. 1989;321(3):129–35.
Kim AJ, Lim HJ, Ro H, Ko KP, Han SY, Chang JH, et al. Low-dose aspirin for prevention of cardiovascular disease in patients with chronic kidney disease. PLoS One. 2014;9(8):e104179. Published online 2014 Aug 5
Jardine MJ, Ninomiya T, Perkovic V, Cass A, Turnbull F, Gallagher MP, et al. Aspirin is beneficial in hypertensive patients with chronic kidney disease: a post-hoc subgroup analysis of a randomized controlled trial. J Am Coll Cardiol. 2010;56(12):956–65.
Tang WH, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575–84.
Harris RC, Breyer MD. Physiological regulation of cyclooxygenase-2 in the kidney. Am J Physiol Renal Physiol. 2001;281(1):F1–11.
Okumura M, Imanishi M, Yamashita T, Yamamura Y, Kim S, Iwao H, et al. Renal production of thromboxane and prostaglandins in a rat model of type 2 diabetes. Life Sci. 2000;66(5):371–7.
Boffa JJ, Just A, Coffman TM, Arendshorst WJ. Thromboxane receptor mediates renal vasoconstriction and contributes to acute renal failure in endotoxemic mice. J Am Soc Nephrol. 2004;15(9):2358–65.
Lomnicka M, Karouni K, Sue M, Wessel LA, Bing RJ. Effects of nonsteroidal anti-inflammatory drugs on prostacyclin and thromboxane in the kidney. Pharmacology. 2003;68(3):147–53.
Boffa JJ, Just A, Coffman TM, et al. Thromboxane receptor mediates renal vasoconstriction and contributes to acute renal failure in endotoxemic mice. J Am Soc. 2004;15(9):2358–65.
Baigent C, Landray M, Leaper C, Altmann P, Armitage J, Baxter A, et al. First United Kingdom Heart and Renal Protection (UK-HARP-I) study: biochemical efficacy and safety of simvastatin and safety of low-dose aspirin in chronic kidney disease. Am J Kidney Dis. 2005;45:473–84.
Kurth T, Glynn RJ, Walker AM, Rexrode KM, Buring JE, Stampfer MJ, et al. Analgesic use and change in kidney function in apparently healthy men. Am J Kidney Dis. 2003;42(2):234–44.
Yao L, Young N, Liu H, Li Z, Sun W, Goldhammer J, et al. Evidence for preoperative aspirin improving major outcomes in patients with chronic kidney disease undergoing cardiac surgery: a cohort study. Ann Surg. 2015;261(1):207–12.
Pastori D, Pignatelli P, Perticone F, Sciacqua A, Carnevale R, Farcomeni A, et al. Aspirin and renal insufficiency progression in patients with atrial fibrillation and chronic kidney disease. Int J Cardiol. 2016;223:619–24.
Evans M, Fored CM, Bellocco R, Fitzmaurice G, Fryzek JP, McLaughlin JK, et al. Acetaminophen, aspirin and progression of advanced chronic kidney disease. Nephrol Dial Transplant. 2009;24(6):1908–18.
Okada S, Morimoto T, Ogawa H, Sakuma M, Soejima H, Nakayama M, et al. Is long-term low-dose aspirin therapy associated with renal dysfunction in patients with type 2 diabetes? JPAD2 Cohort Study. PLoS One. 2016;11(1):e0147635.
Ethier J, Bragg-Gresham JL, Piera L, et al. Aspirin prescription and outcomes in hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2007;50:602–11.
Funding
AASER was supported by Sociedad Española de Nefrologia (SEN) and Sociedad Madrileña de Nefrología (SOMANE). MG, GFJ, DA, AO, and JL are supported by ISCIII RETIC REDINREN RD016/009 and FEDER funds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments.
Electronic supplementary material
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Goicoechea, M., de Vinuesa, S.G., Quiroga, B. et al. Aspirin for Primary Prevention of Cardiovascular Disease and Renal Disease Progression in Chronic Kidney Disease Patients: a Multicenter Randomized Clinical Trial (AASER Study). Cardiovasc Drugs Ther 32, 255–263 (2018). https://doi.org/10.1007/s10557-018-6802-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-018-6802-1