Abstract
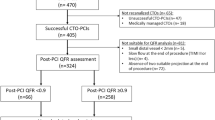
The feasibility and prognostic value of quantitative flow ratio (QFR) after percutaneous coronary intervention (PCI) in ST-segment elevation myocardial infarction (STEMI) patients have not been assessed. The aim of this study was to investigate the prognostic utility of post-PCI QFR to predict outcomes in STEMI and determine the influence of functional results, in both culprit and nonculprit lesions, after PCI. Patients undergoing PCI of culprit lesions and receiving staged procedures of nonculprit lesions after 7 days were enrolled from 2 centers and underwent post-PCI QFR. The primary outcome was the vessel-oriented composite endpoints (VOCEs), defined as vessel-related cardiovascular death, vessel-related myocardial infarction, and target vessel revascularization. Four hundred fifteen vessels (186 culprit lesions and 219 nonculprit lesions) in 186 patients were analyzed. Measured at staged PCI, the post-PCI QFR of culprit lesions was significantly lower than that of nonculprit lesions (0.92 ± 0.10 versus 0.95 ± 0.08, p < 0.001). The multivariable model demonstrated that low post-PCI QFR was an independent predictor of 2-year VOCE (20.8% versus 5.7%; hazard ratio 2.718; 95% CI 1.347–5.486; p = 0.005). In STEMI patients with a low angiography-derived index of microcirculatory resistance (≤ 40U), a good correlation and agreement between post-PCI QFR value of culprit lesions at primary and staged procedures (r = 0.942; mean difference: − 0.0017 [− 0.074 to 0.070]) was identified. In conclusion, culprit lesions suffered from suboptimal functional results more frequently compared to nonculprit lesions after PCI in STEMI patients. Low post-PCI QFR was associated with subsequent adverse clinical outcomes. After stenting, culprit lesions may feasibly be assessed through QFR without significant microvascular dysfunction.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Abbreviations
- ACS:
-
Acute coronary syndrome
- AUC:
-
Area under the curve
- CABG:
-
Coronary artery bypass graft
- CMR:
-
Cardiac magnetic resonance
- cTFC:
-
Corrected TIMI frame count
- IMRangio :
-
Angiography‐derived index of microcirculatory resistance
- IMR:
-
Index of microcirculatory resistance
- IVUS:
-
Intravascular ultrasound
- FFR:
-
Fractional flow reserve
- MBG:
-
Myocardial blush grade
- OCT:
-
Optical coherence tomography
- PCI:
-
Percutaneous coronary intervention
- QCA:
-
Quantitative coronary angiography
- QFR:
-
Quantitative flow ratio
- ROC:
-
Receiver-operating characteristic
- STEMI:
-
ST-segment elevation myocardial infarction
- TIMI:
-
Thrombolysis in myocardial infarction
- TVR:
-
Target vessel revascularization
- VOCE:
-
Vessel-oriented composite endpoint
References
Neumann FJ, Sousa-Uva M, Ahlsson A et al (2019) 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 40:87–165. https://doi.org/10.1093/eurheartj/ehy394
Sabate M, Brugaletta S, Cequier A et al (2016) Clinical outcomes in patients with ST-segment elevation myocardial infarction treated with everolimus-eluting stents versus bare-metal stents (EXAMINATION): 5-year results of a randomised trial. Lancet 387:357–366. https://doi.org/10.1016/S0140-6736(15)00548-6
Pedersen F, Butrymovich V, Kelbæk H et al (2014) Short- and long-term cause of death in patients treated with primary PCI for STEMI. J Am Coll Cardiol 64:2101–2108. https://doi.org/10.1016/j.jacc.2014.08.037
Sorajja P, Gersh BJ, Cox DA et al (2007) Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J 28:1709–1716. https://doi.org/10.1093/eurheartj/ehm184
Brieger D, Pocock SJ, Blankenberg S et al (2020) Two-year outcomes among stable high-risk patients following acute MI. Insights from a global registry in 25 countries. Int J Cardiol 311:7–14. https://doi.org/10.1016/j.ijcard.2020.01.070
Zimmermann FM, Ferrara A, Johnson NP et al (2015) Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J 36:3182–3188. https://doi.org/10.1093/eurheartj/ehv452
De Bruyne B, Pijls NH, Kalesan B et al (2012) Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367:991–1001. https://doi.org/10.1056/NEJMoa1205361
Johnson NP, Toth GG, Lai D et al (2014) Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol 64:1641–1654. https://doi.org/10.1016/j.jacc.2014.07.973
Zimmermann FM, Omerovic E, Fournier S et al (2019) Fractional flow reserve-guided percutaneous coronary intervention vs. medical therapy for patients with stable coronary lesions: meta-analysis of individual patient data. Eur Heart J 40:180–186. https://doi.org/10.1093/eurheartj/ehy812
Piroth Z, Toth GG, Tonino PAL et al (2017) Prognostic value of fractional flow reserve measured immediately after drug-eluting stent implantation. Circ Cardiovasc Interv 10:e005233. https://doi.org/10.1161/CIRCINTERVENTIONS.116.005233
Agarwal SK, Kasula S, Hacioglu Y et al (2016) Utilizing post-intervention fractional flow reserve to optimize acute results and the relationship to long-term outcomes. JACC Cardiovasc Interv 9:1022–1031. https://doi.org/10.1016/j.jcin.2016.01.046
Kasula S, Agarwal SK, Hacioglu Y et al (2016) Clinical and prognostic value of poststenting fractional flow reserve in acute coronary syndromes. Heart 102:1988–1994. https://doi.org/10.1136/heartjnl-2016-309422
Li SJ, Ge Z, Kan J et al (2017) Cutoff value and long-term prediction of clinical events by FFR Measured immediately after implantation of a drug-eluting stent in patients with coronary artery disease: 1- to 3-year results from the DKCRUSH VII Registry Study. JACC Cardiovasc Interv 10:986–995. https://doi.org/10.1016/j.jcin.2017.02.012
Rimac G, Fearon WF, De Bruyne B et al (2017) Clinical value of post-percutaneous coronary intervention fractional flow reserve value: a systematic review and meta-analysis. Am Heart J 183:1–9. https://doi.org/10.1016/j.ahj.2016.10.005
Tu S, Westra J, Yang J et al (2016) Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the International Multicenter FAVOR Pilot Study. JACC Cardiovasc Interv 9:2024–2035. https://doi.org/10.1016/j.jcin.2016.07.013
Xu B, Tu S, Qiao S et al (2017) Diagnostic accuracy of angiography-based quantitative flow ratio measurements for online assessment of coronary stenosis. J Am Coll Cardiol 70:3077–3087. https://doi.org/10.1016/j.jacc.2017.10.035
Collet C, Onuma Y, Sonck J et al (2018) Diagnostic performance of angiography-derived fractional flow reserve: a systematic review and Bayesian meta-analysis. Eur Heart J 39:3314–3321. https://doi.org/10.1093/eurheartj/ehy445
Westra J, Andersen BK, Campo G et al (2018) Diagnostic performance of in-procedure angiography-derived quantitative flow reserve compared to pressure-derived fractional flow reserve: the FAVOR II Europe-Japan Study. J Am Heart Assoc 7:e009603. https://doi.org/10.1161/JAHA.118.009603
Biscaglia S, Tebaldi M, Brugaletta S et al (2019) Prognostic value of QFR measured immediately after successful stent implantation: the International Multicenter Prospective HAWKEYE Study. JACC Cardiovasc Interv 12:2079–2088. https://doi.org/10.1016/j.jcin.2019.06.003
Kogame N, Takahashi K, Tomaniak M et al (2019) Clinical implication of quantitative flow ratio after percutaneous coronary intervention for 3-vessel disease. JACC Cardiovasc Interv 12:2064–2075. https://doi.org/10.1016/j.jcin.2019.08.009
Lauri F, Macaya F, Mejia-Renteria H et al (2019) Angiography-derived functional assessment of non-culprit coronary stenoses during primary percutaneous coronary intervention for ST-elevation myocardial infarction. EuroIntervention 15:e1594–e1601. https://doi.org/10.4244/EIJ-D-18-01165
Spitaleri G, Tebaldi M, Biscaglia S et al (2018) Quantitative flow ratio identifies nonculprit coronary lesions requiring revascularization in patients with ST-segment-elevation myocardial infarction and multivessel disease. Circ Cardiovasc Interv 11:e006023. https://doi.org/10.1161/CIRCINTERVENTIONS.117.006023
Tang J, Lai Y, Tu S et al (2019) Quantitative flow ratio guided residual functional SYNTAX score for risk assessment in patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention. EuroIntervention. https://doi.org/10.4244/EIJ-D-19-00369
Smits PC, Abdel-Wahab M, Neumann FJ et al (2017) Fractional flow reserve-guided multivessel angioplasty in myocardial infarction. N Engl J Med 376:1234–1244. https://doi.org/10.1056/NEJMoa1701067
Engstrøm T, Kelbæk H, Helqvist S et al (2015) Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet 386:665–671. https://doi.org/10.1016/s0140-6736(15)60648-1
De Bruyne B, Pijls NH, Bartunek J et al (2001) Fractional flow reserve in patients with prior myocardial infarction. Circulation 104:157–162. https://doi.org/10.1161/01.cir.104.2.157
Hennigan B, Layland J, Fearon WF et al (2014) Fractional flow reserve and the index of microvascular resistance in patients with acute coronary syndromes. EuroIntervention 10(Suppl T):T55–T63. https://doi.org/10.4244/EIJV10STA10
Sianos G, Morel MA, Kappetein AP et al (2005) The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1:219–227
Ng VG, Lansky AJ, Toro S et al (2016) Prognostic utility of myocardial blush grade after PCI in patients with NSTE-ACS: analysis from the ACUITY trial. Catheter Cardiovasc Interv 88:215–224. https://doi.org/10.1002/ccd.25865
Jolly SS, Cairns JA, Lavi S et al (2018) Thrombus aspiration in patients with high thrombus burden in the TOTAL trial. J Am Coll Cardiol 72:1589–1596. https://doi.org/10.1016/j.jacc.2018.07.04
Nijveldt R, Beek AM, Hirsch A et al (2008) Functional recovery after acute myocardial infarction: comparison between angiography, electrocardiography, and cardiovascular magnetic resonance measures of microvascular injury. J Am Coll Cardiol 52:181–189. https://doi.org/10.1016/j.jacc.2008.04.006
Song L, Tu S, Sun Z et al (2020) Quantitative flow ratio-guided strategy versus angiography-guided strategy for percutaneous coronary intervention: rationale and design of the FAVOR III China trial. Am Heart J 223:72–80. https://doi.org/10.1016/j.ahj.2020.02.015
De Maria GL, Scarsini R, Shanmuganathan M et al (2020) Angiography-derived index of microcirculatory resistance as a novel, pressure-wire-free tool to assess coronary microcirculation in ST elevation myocardial infarction. Int J Cardiovasc Imaging 36:1395–1406. https://doi.org/10.1007/s10554-020-01831-7
Hoshino M, Kanaji Y, Hamaya R et al (2019) Prognostic value of post-intervention fractional flow reserve after intravascular ultrasound-guided second-generation drug-eluting coronary stenting. Eurointervention 15:e779–e787. https://doi.org/10.4244/EIJ-D-18-01032
Cho YK, Nam CW, Han JK et al (2015) Usefulness of combined intravascular ultrasound parameters to predict functional significance of coronary artery stenosis and determinants of mismatch. EuroIntervention 11:163–170. https://doi.org/10.4244/EIJV11I2A30
Tebaldi M, Biscaglia S, Fineschi M et al (2018) Evolving routine standards in invasive hemodynamic assessment of coronary stenosis: the Nationwide Italian SICI-GISE Cross-Sectional ERIS Study. JACC Cardiovasc Interv 11:1482–1491. https://doi.org/10.1016/j.jcin.2018.04.037
Jeremias A, Davies JE, Maehara A et al (2019) Blinded physiological assessment of residual ischemia after successful angiographic percutaneous coronary intervention: the DEFINE PCI study. J Am Coll Cardiol Interv 12:1991–2001. https://doi.org/10.1016/j.jcin.2019.05.054
van Werkum JW, Heestermans AA, Zomer AC et al (2009) Predictors of coronary stent thrombosis: the Dutch Stent Thrombosis Registry. J Am Coll Cardiol 53:1399–1409. https://doi.org/10.1016/j.jacc.2008.12.055
Tamita K, Akasaka T, Takagi T et al (2002) Effects of microvascular dysfunction on myocardial fractional flow reserve after percutaneous coronary intervention in patients with acute myocardial infarction. Catheter Cardiovasc Interv 57:452–459. https://doi.org/10.1002/ccd.27529
van de Hoef TP, Nolte F, EchavarrÍa-Pinto M et al (2014) Impact of hyperaemic microvascular resistance on fractional flow reserve measurements in patients with stable coronary artery disease: insights from combined stenosis and microvascular resistance assessment. Heart 100:951–959. https://doi.org/10.1136/heartjnl-2013-305124
Ntalianis A, Sels JW, Davidavicius G et al (2010) Fractional flow reserve for the assessment of nonculprit coronary artery stenoses in patients with acute myocardial infarction. JACC Cardiovasc Interv 3:1274–1281. https://doi.org/10.1016/j.jcin.2010.08.025
Lee JM, Kim HK, Lim KS et al (2018) Influence of local myocardial damage on index of microcirculatory resistance and fractional flow reserve in target and nontarget vascular territories in a porcine microvascular injury model. JACC Cardiovasc Interv 11:717–724. https://doi.org/10.1016/j.jcin.2017.11.028
De Maria GL, Cuculi F, Patel N et al (2015) How does coronary stent implantation impact on the status of the microcirculation during primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction? Eur Heart J 36:3165–3177. https://doi.org/10.1093/eurheartj/ehv353
Cuculi F, De Maria GL, Meier P et al (2014) Impact of microvascular obstruction on the assessment of coronary flow reserve, index of microcirculatory resistance, and fractional flow reserve after ST-segment elevation myocardial infarction. J Am Coll Cardiol 64:1894–1904. https://doi.org/10.1016/j.jacc.2014.07.987
van Zandvoort LJC, Masdjedi K, Witberg K et al (2019) Explanation of postprocedural fractional flow reserve below 0.85: a comprehensive ultrasound analysis of the FFR SEARCH registry. Circ Cardiovasc Interv 12:e007030. https://doi.org/10.1161/CIRCINTERVENTIONS.118.007030
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 81670403), Grant of Shanghai Science and Technology Committee (Nos. 18411950300, 19XD1403300 and 19411963200) and the Shanghai Municipal Health Commission (No. 2019LJ10).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Tu has received research support from Medis Medical Imaging and Pulse Medical Imaging. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki. The Institutional Review Board or ethics committee approved the study protocol, and all patients provided written informed consent before enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tang, J., Chu, J., Hou, H. et al. Clinical implication of QFR in patients with ST-segment elevation myocardial infarction after drug-eluting stent implantation. Int J Cardiovasc Imaging 37, 755–766 (2021). https://doi.org/10.1007/s10554-020-02068-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02068-0