Abstract
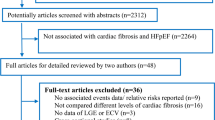
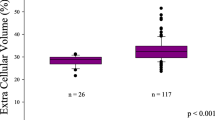
Evidence regarding the relationship between diffuse myocardial fibrosis and the prognosis of heart failure with reduced ejection fraction (HFrEF) was limited. Therefore, this study set out to investigate whether diffuse myocardial fibrosis was independently related to the prognosis of failure with reduced ejection fraction in Chinese patients after adjusting for other covariates. The present study was a cohort study. A total of 45 consecutive HFrEF patients were involved in Zhongshan Hospital of Fudan University in China from 1/9/2015 to 31/12/2016. The target-independent variable was extracellular volume (ECV) quantified by cardiac magnetic resonance T1 mapping using the modified Look-Locker inversion recovery (MOLLI) sequence at baseline. To assess the prognostic impact of MOLLI–ECV, its association with hospitalization for heart failure/cardiac death was tested by multivariable Cox regression analysis. Covariates involved in this study included age, gender, body mass index, heart rate, systolic blood pressure diastolic blood pressure, smoking, hypertension, diabetes mellitus, etiology, NYHA functional class, blood urea nitrogen, creatinine, serum uric acid, total bilirubin, and growth stimulation-expressed gene 2. Ten age- and sex-matched healthy participants with no history of cardiovascular disease served as a control group. Mean MOLLI–ECV was significantly higher in HFrEF patients versus healthy controls (29.55 ± 1.46% vs. 23.17 ± 1.93%, P < 0.001). Patients were followed for 9 months, during which the primary outcome (cardiac death or first heart failure hospitalization) occurred in 15 patients. By Kaplan–Meier analysis, patients with high MOLLI–ECV ≥ 30.10% had shorter event-free survival than the middle (MOLLI–ECV between 30.10 and 28.60) and low (MOLLI–ECV < 28.60) MOLLI–ECV patients (log-rank, P = 0.0035). Result of fully-adjusted multivariable Cox regression analysis showed MOLLI–ECV was positively associated with the composite outcome of HFrEF patients after adjusting confounders hazard ratio (HR) 2.57, 95% CI (1.09, 6.04). By subgroup analysis, a stronger association was seen in patients who with NYHA functional class III–IV, hematocrit < 39.8%, left atrial diameter ≥ 53.5 mm, or without the medical history of MRA or diuretics other than MRA. The P for interaction was < 0.05. In HFrEF patients, the relationship between MOLLI–ECV determined by CMR and the composite outcome is linear. High MOLLI–ECV was associated with a higher rate of cardiac mortality and first HF hospitalization in the short term follow up.




Similar content being viewed by others
Abbreviations
- HFrEF:
-
Heart failure with reduced ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- ECV:
-
Extracellular volume
- MOLLI:
-
Modified look-locker inversion recovery
- NYHA:
-
New york heart association
- HR:
-
Hazard ratio
- MRA:
-
Mineralocorticoid receptor antagonism
- HF:
-
Heart failure
- LV:
-
Left ventricle
- CMR:
-
Cardiovascular magnetic resonance
- LGE:
-
Late gadolinium enhancement
- NT-proBNP:
-
N-terminal prohormone of brain natriuretic peptide
- LVEF:
-
Left ventricular ejection fraction
- ECG:
-
Electrocardiogram
- bSSFP:
-
Balanced steady-state free precession sequence
- BMI:
-
Body mass index
- PINP:
-
N-terminal propeptide of type I procollagen
- PIIINP:
-
N-terminal propeptide of type III procollagen
- PICP:
-
Type I procollagen carboxyterminal propeptide
- CI:
-
Confidence interval
References
Yancy CW et al (2013) 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128(16):1810–1852
Heusch G et al (2014) Cardiovascular remodelling in coronary artery disease and heart failure. Lancet 383(9932):1933–1943
Liu T et al (2017) Current understanding of the pathophysiology of myocardial fibrosis and its quantitative assessment in heart failure. Front Physiol 8:238
Kong P, Christia P, Frangogiannis NG (2014) The pathogenesis of cardiac fibrosis. Cell Mol Life Sci 71(4):549–574
Scully PR et al (2018) Myocardial extracellular volume quantification by cardiovascular magnetic resonance and computed tomography. Curr Cardiol Rep 20(3):15
Haaf P et al (2016) Cardiac T1 mapping and extracellular volume (ECV) in clinical practice: a comprehensive review. J Cardiovasc Magn Reson 18(1):89
Barison A et al (2015) Myocardial interstitial remodelling in non-ischaemic dilated cardiomyopathy: insights from cardiovascular magnetic resonance. Heart Fail Rev 20(6):731–749
Duca F et al (2016) Interstitial fibrosis, functional status, and outcomes in heart failure with preserved ejection fraction: insights from a prospective cardiac magnetic resonance imaging study. Circ Cardiovasc Imaging 9(12):e005277
Roy C et al (2018) Associations and prognostic significance of diffuse myocardial fibrosis by cardiovascular magnetic resonance in heart failure with preserved ejection fraction. J Cardiovasc Magn Reson 20(1):55
Schelbert EB et al (2017) Temporal relation between myocardial fibrosis and heart failure with preserved ejection fraction: association with baseline disease severity and subsequent outcome. JAMA Cardiol 2(9):995–1006
Kanagala P et al (2019) Relationship between focal and diffuse fibrosis assessed by CMR and clinical outcomes in heart failure with preserved ejection fraction. JACC Cardiovasc Imaging 12(11 Pt 2):2291–2301
Mascherbauer J et al (2013) Cardiac magnetic resonance postcontrast T1 time is associated with outcome in patients with heart failure and preserved ejection fraction. Circ Cardiovasc Imaging 6(6):1056–1065
[Chinese guidelines for the diagnosis and treatment of heart failure 2018]. Zhonghua Xin Xue Guan Bing Za Zhi, 2018. 46(10): 760–789.
Lang RM et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270
Weber KT et al (2013) Myofibroblast-mediated mechanisms of pathological remodelling of the heart. Nat Rev Cardiol 10(1):15–26
Azevedo CF et al (2010) Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol 56(4):278–287
Brown PF et al (2018) Towards cardiac MRI based risk stratification in idiopathic dilated cardiomyopathy. Heart. https://doi.org/10.1136/heartjnl-2018-313767
Frangogiannis NG (2019) The extracellular matrix in ischemic and nonischemic heart failure. Circ Res 125(1):117–146
Gyongyosi M et al (2017) Myocardial fibrosis: biomedical research from bench to bedside. Eur J Heart Fail 19(2):177–191
Treibel TA et al (2019) Extracellular volume associates with outcomes more strongly than native or post-contrast myocardial T1. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2019.03.017
Barison A et al (2015) Prognostic significance of myocardial extracellular volume fraction in nonischaemic dilated cardiomyopathy. J Cardiovasc Med (Hagerstown) 16(10):681–687
Gulati A et al (2018) Absence of myocardial fibrosis predicts favorable long-term survival in new-onset heart failure. Circ Cardiovasc Imaging 11(9):e007722
Almehmadi F et al (2014) Prevalence of myocardial fibrosis patterns in patients with systolic dysfunction: prognostic significance for the prediction of sudden cardiac arrest or appropriate implantable cardiac defibrillator therapy. Circ Cardiovasc Imaging 7(4):593–600
Aoki T et al (2011) Prognostic impact of myocardial interstitial fibrosis in non-ischemic heart failure Comparison between preserved and reduced ejection fraction heart failure. Circ J 75(11):2605–2613
Acknowledgements
This study was supported by grants from the Program for the Outstanding Academic Leaders supported by Shanghai Science and Technology Commission (Grant No. 16XD1400700), National Natural Science Foundation of China (Grant No. 81370199),and National Basic Research Program of China (973 350 Program, 2012CB518605).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, F., Xu, M., Fan, Y. et al. Diffuse myocardial fibrosis and the prognosis of heart failure with reduced ejection fraction in Chinese patients: a cohort study. Int J Cardiovasc Imaging 36, 671–689 (2020). https://doi.org/10.1007/s10554-019-01752-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01752-0