Abstract
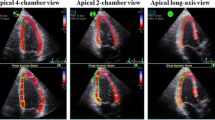
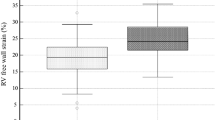
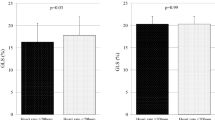
Left ventricular (LV) diastolic dysfunction and longitudinal systolic dysfunction were identified in patients with diabetes mellitus (DM). This study’s aim was to investigate the impact of LV longitudinal systolic function on LV diastolic function in DM patients with preserved LV ejection fraction (LVEF). We studied 177 DM patients with preserved LVEF (all ≥50%), and 82 age-, gender- and LVEF-matched healthy volunteers as control. Global longitudinal strain (GLS) was defined as the average peak strain of 18 segments from standard apical views, GLS <18% as subclinical LV systolic dysfunction (LVSD), and LV dispersion as the standard deviation of time-to-peak strain from the same views. For DM patients with LVSD (n = 74), E/A and E’ were lower, and E/E’ and isovolumic relaxation time (IVRT) were greater than for DM patients without LVSD (n = 103) and normal controls (n = 82). Moreover, these parameters were lower for DM patients without LVSD than for normal controls. Multivariate analysis revealed that GLS was a strong determinative factor for E’ and E/E’ (β = 0.30, p < 0.001 and β = −0.25, p < 0.001, respectively), as was LV dispersion for E-wave deceleration time and IVRT (β = 0.21, p = 0.002 and β = 0.30, p < 0.001, respectively) independently of age. For normal subjects, however, only age was associated with all LV diastolic parameters. In conclusions, in contrast to age-related LV diastolic dysfunction in normal subjects, in DM patients with preserved LVEF, LV diastolic function was associated with LV longitudinal systolic function and LV dispersion independently of age. Our findings have obvious clinical implications for the management of DM patients.



Similar content being viewed by others
References
Rubler S, Dlugash J, Yuceoglu YZ, Kumral T, Branwood AW, Grishman A (1972) New type of cardiomyopathy associated with diabetic glomerulosclerosis. Am J Cardiol 30:595–602
Fang ZY, Prins JB, Marwick TH (2004) Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocr Rev 25:543–567
MacDonald MR, Petrie MC, Varyani F, Ostergren J, Michelson EL, Young JB et al (2008) Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) programme. Eur Heart J 29:1377–1385
Galderisi M (2006) Diastolic dysfunction and diabetic cardiomyopathy: evaluation by Doppler echocardiography. J Am Coll Cardiol 48:1548–1551
From AM, Scott CG, Chen HH (2010) The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction a population-based study. J Am Coll Cardiol 55:300–305
Poirier P, Bogaty P, Garneau C, Marois L, Dumesnil JG (2001) Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care 24:5–10
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 28:1–39, e14
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of echocardiography and the European Association of cardiovascular imaging. J Am Soc Echocardiogr 29:277–314
Haugaa KH, Smedsrud MK, Steen T, Kongsgaard E, Loennechen JP, Skjaerpe T et al (2010) Mechanical dispersion assessed by myocardial strain in patients after myocardial infarction for risk prediction of ventricular arrhythmia. JACC Cardiovasc Imaging 3:247–256
Ernande L, Rietzschel ER, Bergerot C, De Buyzere ML, Schnell F, Groisne L et al (2010) Impaired myocardial radial function in asymptomatic patients with type 2 diabetes mellitus: a speckle-tracking imaging study. J Am Soc Echocardiogr 23:1266–1272
Ernande L, Bergerot C, Girerd N, Thibault H, Davidsen ES, Gautier Pignon-Blanc P et al (2014) Longitudinal myocardial strain alteration is associated with left ventricular remodeling in asymptomatic patients with type 2 diabetes mellitus. J Am Soc Echocardiogr 27:479–488
Ernande L, Bergerot C, Rietzschel ER, De Buyzere ML, Thibault H, Pignonblanc PG et al (2011) Diastolic dysfunction in patients with type 2 diabetes mellitus: is it really the first marker of diabetic cardiomyopathy? J Am Soc Echocardiogr 24:1268–75, e1
Mochizuki Y, Tanaka H, Matsumoto K, Sano H, Toki H, Shimoura H et al (2015) Clinical features of subclinical left ventricular systolic dysfunction in patients with diabetes mellitus. Cardiovasc Diabetol 14:37
Mochizuki Y, Tanaka H, Matsumoto K, Sano H, Toki H, Shimoura H et al (2015) Association of peripheral nerve conduction in diabetic neuropathy with subclinical left ventricular systolic dysfunction. Cardiovasc Diabetol 14:47
Ng AC, Delgado V, Bertini M, van der Meer RW, Rijzewijk LJ, Shanks M et al (2009) Findings from left ventricular strain and strain rate imaging in asymptomatic patients with type 2 diabetes mellitus. Am J Cardiol 104:1398–1401
Nakai H, Takeuchi M, Nishikage T, Lang RM, Otsuji Y (2009) Subclinical left ventricular dysfunction in asymptomatic diabetic patients assessed by two-dimensional speckle tracking echocardiography: correlation with diabetic duration. Eur J Echocardiogr 10:926–932
Ernande L, Thibault H, Bergerot C, Moulin P, Wen H, Derumeaux G et al (2012) Systolic myocardial dysfunction in patients with type 2 diabetes mellitus: identification at MR imaging with cine displacement encoding with stimulated echoes. Radiology 265:402–409
Liu JE, Palmieri V, Roman MJ, Bella JN, Fabsitz R, Howard BV et al (2001) The impact of diabetes on left ventricular filling pattern in normotensive and hypertensive adults: the strong heart study. J Am Coll Cardiol 37:1943–1949
Liu JE, Robbins DC, Palmieri V, Bella JN, Roman MJ, Fabsitz R et al (2003) Association of albuminuria with systolic and diastolic left ventricular dysfunction in type 2 diabetes: the strong heart study. J Am Coll Cardiol 41:2022–2028
Yip G, Wang M, Zhang Y, Fung JW, Ho PY, Sanderson JE (2002) Left ventricular long axis function in diastolic heart failure is reduced in both diastole and systole: time for a redefinition? Heart 87:121–125
Vinereanu D, Lim PO, Frenneaux MP, Fraser AG (2005) Reduced myocardial velocities of left ventricular long-axis contraction identify both systolic and diastolic heart failure-a comparison with brain natriuretic peptide. Eur J Heart Fail 7:512–519
Zoroufian A, Razmi T, Taghavi-Shavazi M, Lotfi-Tokaldany M, Jalali A (2014) Evaluation of subclinical left ventricular dysfunction in diabetic patients: longitudinal strain velocities and left ventricular dyssynchrony by two-dimensional speckle tracking echocardiography study. Echocardiography 31:456–463
Ring M, Persson H, Mejhert M, Edner M (2007) Post-systolic motion in patients with heart failure—a marker of left ventricular dyssynchrony? Eur J Echocardiogr 8:352–359
Santos AB, Kraigher-Krainer E, Bello N, Claggett B, Zile MR, Pieske B et al (2014) Left ventricular dyssynchrony in patients with heart failure and preserved ejection fraction. Eur Heart J 35:42–47
Vanninen E, Unsitupa MI, Lansimies E (1996) Ventricular repolarization is correlated with metabolic control in newly diagnosed type 2 diabetes. Clin Physiol 16:449–461
van Hoeven KH, Factor SM (1990) A comparison of the pathological spectrum of hypertensive, diabetic, and hypertensive-diabetic heart disease. Circulation 82:848–855
Mottram PM, Marwick TH (2005) Assessment of diastolic function: what the general cardiologist needs to know. Heart 91:681–695
Lester SJ, Tajik AJ, Nishimura RA, Oh JK, Khandheria BK, Seward JB (2008) Unlocking the mysteries of diastolic function: deciphering the Rosetta Stone 10 years later. J Am Coll Cardiol 51:679–689
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from the patient.
Rights and permissions
About this article
Cite this article
Mochizuki, Y., Tanaka, H., Matsumoto, K. et al. Impact of left ventricular longitudinal functional mechanics on the progression of diastolic function in diabetes mellitus. Int J Cardiovasc Imaging 33, 1905–1914 (2017). https://doi.org/10.1007/s10554-017-1198-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-017-1198-8