Abstract
Purpose
Based on suggestive findings from a recent study of high-risk Japanese patients, we sought to determine whether the risk of colorectal polyps associated with smoking may be modified by daily use of aspirin in an analysis of a large US screening population.
Methods
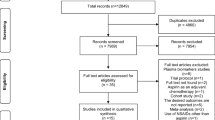
This is a cross-sectional study of 2,918 consecutive colonoscopy patients at a university hospital over a 30-month period. Data were abstracted from electronic medical records. Multivariate models of polyp counts were used to examine the competing risks of smoking and aspirin use. Models were further stratified by polyp location (proximal vs. distal) and pathologic subtype (dysplastic vs. serrated).
Results
Incidental rate of polyps was higher among active smokers [incidence rate ratio (IRR) 1.72; 95 % confidence interval (CI) 1.46–2.02] and lower among daily aspirin users (IRR 0.73; 95 % CI 0.61–0.86) compared to those who used neither. Smoking interacts significantly with aspirin use resulting in loss of aspirin protection (IRR 1.69; 95 % CI 1.28–2.24). Stratified analyses demonstrate that aspirin specifically reduces the risk of traditional dysplastic adenomas (IRR 0.72; 95 % CI 0.61–0.86) not serrated/hyperplastic polyps (IRR 0.92; 95 % CI 0.72–1.17) and that the modification of aspirin protection by smoking is primarily observed within the distal colorectum (p < 0.03).
Conclusions
We report for the first time, in a typical risk US clinical population, a lack of protective association of aspirin for polyps among active smokers. Future prospective studies are recommended to confirm this mitigating effect in order to improve the precision of the growing evidence base about the chemopreventive benefit of aspirin in colorectal cancer.


Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- CMH:
-
Cochran–Mantel–Haenszel
- CRC:
-
Colorectal cancer
- EMR:
-
Electronic medical record
- IRR:
-
Incidence rate ratio
- NSAID:
-
Nonsteroidal anti-inflammatory drug
- OR:
-
Odds ratio
- PDR:
-
Polyp Detection Rate
References
Fearon ER, Vogelstein B (1990) A genetic model for colorectal tumorigenesis. Cell 61:759–767
Drew DA, Devers TJ, O’Brien MJ, Horelik NA, Levine J, Rosenberg DW (2014) HD chromoendoscopy coupled with DNA mass spectrometry profiling identifies somatic mutations in microdissected human proximal aberrant crypt foci. Mol Cancer Res MCR 12:823–829
Kavanagh AM, Giovannucci EL, Fuchs CS, Colditz GA (1998) Screening endoscopy and risk of colorectal cancer in United States men. Cancer Causes Control CCC 9:455–462
Lieberman DA, Williams JL, Holub JL et al (2014) Colonoscopy utilization and outcomes 2000 to 2011. Gastrointest Endosc 80(133–43):e3
Siegel R, Desantis C, Jemal A (2014) Colorectal cancer statistics, 2014. CA Cancer J Clin 64:104–117
Potter JD, Slattery ML, Bostick RM, Gapstur SM (1993) Colon cancer: a review of the epidemiology. Epidemiol Rev 15:499–545
Choi SY, Kahyo H (1991) Effect of cigarette smoking and alcohol consumption in the etiology of cancers of the digestive tract. Int J Cancer 49:381–386
Sandler RS, Sandler DP, Comstock GW, Helsing KJ, Shore DL (1988) Cigarette smoking and the risk of colorectal cancer in women. J Natl Cancer Inst 80:1329–1333
Hoff G, Vatn MH, Larsen S (1987) Relationship between tobacco smoking and colorectal polyps. Scand J Gastroenterol 22:13–16
Zahm SH, Cocco P, Blair A (1991) Tobacco smoking as a risk factor for colon polyps. Am J Public Health 81:846–849
Botteri E, Iodice S, Raimondi S, Maisonneuve P, Lowenfels AB (2008) Cigarette smoking and adenomatous polyps: a meta-analysis. Gastroenterology 134:388–395
Rex DK, Johnson DA, Anderson JC et al (2009) American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol 104:739–750
Botteri E, Iodice S, Bagnardi V, Raimondi S, Lowenfels AB, Maisonneuve P (2008) Smoking and colorectal cancer: a meta-analysis. JAMA J Am Med Assoc 300:2765–2778
Din FV, Theodoratou E, Farrington SM et al (2010) Effect of aspirin and NSAIDs on risk and survival from colorectal cancer. Gut 59:1670–1679
Chan AT, Arber N, Burn J et al (2012) Aspirin in the chemoprevention of colorectal neoplasia: an overview. Cancer Prev Res 5:164–178
Giardiello FM, Offerhaus GJ, DuBois RN (1995) The role of nonsteroidal anti-inflammatory drugs in colorectal cancer prevention. Eur J Cancer 31A:1071–1076
Thun MJ, Henley SJ, Patrono C (2002) Nonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issues. J Natl Cancer Inst 94:252–266
Chan TA (2002) Nonsteroidal anti-inflammatory drugs, apoptosis, and colon-cancer chemoprevention. Lancet Oncol 3:166–174
Dube C, Rostom A, Lewin G et al (2007) The use of aspirin for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force. Ann Intern Med 146:365–375
Chan AT, Ogino S, Fuchs CS (2007) Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. N Engl J Med 356:2131–2142
Greenspan EJ, Madigan JP, Boardman LA et al (2011) Ibuprofen inhibits activation of nuclear {beta}-catenin in human colon adenomas and induces the phosphorylation of GSK-3{beta}. Cancer Prev Res 4:161–171
Ishikawa H, Mutoh M, Suzuki S, et al (2014) The preventive effects of low-dose enteric-coated aspirin tablets on the development of colorectal tumours in Asian patients: a randomised trial. Gut 63:1755–1759
Bettington M, Walker N, Rosty C et al (2014) Critical appraisal of the diagnosis of the sessile serrated adenoma. Am J Surg Pathol 38:158–166
Bosman FT, World Health Organization, International Agency for Research on Cancer (2010) WHO classification of tumours of the digestive system, 4th edn. International Agency for Research on Cancer, Lyon
Gill P, Wang LM, Bailey A, East JE, Leedham S, Chetty R (2013) Reporting trends of right-sided hyperplastic and sessile serrated polyps in a large teaching hospital over a 4-year period (2009–2012). J Clin Pathol 66:655–658
Lawless JF (1987) Negative binomial and mixed poisson regression. Can J Stat 15:209–225
Richardson DB, Kaufman JS (2009) Estimation of the relative excess risk due to interaction and associated confidence bounds. Am J Epidemiol 169:756–760
Knol MJ, VanderWeele TJ (2012) Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol 41:514–520
Boroff ES, Gurudu SR, Hentz JG, Leighton JA, Ramirez FC (2013) Polyp and adenoma detection rates in the proximal and distal colon. Am J Gastroenterol 108:993–999
Cole BF, Logan RF, Halabi S et al (2009) Aspirin for the chemoprevention of colorectal adenomas: meta-analysis of the randomized trials. J Natl Cancer Inst 101:256–266
Pommergaard HC, Burcharth J, Rosenberg J, Raskov H (2015) Aspirin, calcitriol, and calcium do not prevent adenoma recurrence in a randomized controlled trial. Gastroenterology. doi:10.1053/j.gastro.2015.09.010
Jamal A, Agaku IT, O’Connor E, King BA, Kenemer JB, Neff L (2014) Current cigarette smoking among adults—United States, 2005–2013. MMWR Morb Mortal Wkly Rep 63:1108–1112
Nishihara R, Lochhead P, Kuchiba A et al (2013) Aspirin use and risk of colorectal cancer according to BRAF mutation status. JAMA J Am Med Assoc 309:2563–2571
Chen D, Huang JF, Liu K et al (2014) BRAFV600E mutation and its association with clinicopathological features of colorectal cancer: a systematic review and meta-analysis. PLoS One 9:e90607
Fu X, Zhang X (2014) BRAF mutation as a potential marker to identify the proximal colon serrated polyps with malignant potential. Int J Clin Exp Pathol 7:7319–7322
Nishihara R, Morikawa T, Kuchiba A et al (2013) A prospective study of duration of smoking cessation and colorectal cancer risk by epigenetics-related tumor classification. Am J Epidemiol 178:84–100
Samowitz WS, Albertsen H, Sweeney C et al (2006) Association of smoking, CpG island methylator phenotype, and V600E BRAF mutations in colon cancer. J Natl Cancer Inst 98:1731–1738
Wallace K, Grau MV, Ahnen D et al (2009) The association of lifestyle and dietary factors with the risk for serrated polyps of the colorectum. Cancer Epidemiol Biomark Prev 18:2310–2317
Rosty C, Hewett DG, Brown IS, Leggett BA, Whitehall VL (2013) Serrated polyps of the large intestine: current understanding of diagnosis, pathogenesis, and clinical management. J Gastroenterol 48:287–302
Samadder NJ, Curtin K, Tuohy TM et al (2014) Characteristics of missed or interval colorectal cancer and patient survival: a population-based study. Gastroenterology 146:950–960
Dodou D, de Winter JC (2012) The relationship between distal and proximal colonic neoplasia: a meta-analysis. J Gen Intern Med 27:361–370
Nosho K, Kure S, Irahara N et al (2009) A prospective cohort study shows unique epigenetic, genetic, and prognostic features of synchronous colorectal cancers. Gastroenterology 137(1609–20):e1–e3
Lochhead P, Chan AT, Nishihara R et al (2015) Etiologic field effect: reappraisal of the field effect concept in cancer predisposition and progression. Mod Pathol 28:14–29
Raju GS, Vadyala V, Slack R et al (2013) Adenoma detection in patients undergoing a comprehensive colonoscopy screening. Cancer Med 2:391–402
Butterly L, Robinson CM, Anderson JC et al (2014) Serrated and adenomatous polyp detection increases with longer withdrawal time: results from the New Hampshire Colonoscopy Registry. Am J Gastroenterol 109:417–426 46
Anderson JC, Swede H, Rustagi T et al (2012) Aberrant crypt foci as predictors of colorectal neoplasia on repeat colonoscopy. Cancer Causes Control 23:355–361
Burnett-Hartman AN, Passarelli MN, Adams SV et al (2013) Differences in epidemiologic risk factors for colorectal adenomas and serrated polyps by lesion severity and anatomical site. Am J Epidemiol 177:625–637
Siddiqui AA, Nazario H, Mahgoub A, Patel M, Cipher D, Spechler SJ (2009) For patients with colorectal cancer, the long-term use of statins is associated with better clinical outcomes. Dig Dis Sci 54:1307–1311
Siddiqui A, Nazario HE, Patel M, Mahgoub A, Spechler SJ (2009) Reduction in low-density lipoprotein cholesterol levels during statin therapy is associated with a reduced incidence of advanced colon polyps. Am J Med Sci 338:378–381
Liu Y, Tang W, Wang J et al (2014) Association between statin use and colorectal cancer risk: a meta-analysis of 42 studies. Cancer Causes Control CCC 25:237–249
Ng K, Ogino S, Meyerhardt JA et al (2011) Relationship between statin use and colon cancer recurrence and survival: results from CALGB 89803. J Natl Cancer Inst 103:1540–1551
Lee JE, Baba Y, Ng K et al (2011) Statin use and colorectal cancer risk according to molecular subtypes in two large prospective cohort studies. Cancer Prev Res 4:1808–1815
Limburg PJ, Mahoney MR, Ziegler KL et al (2011) Randomized phase II trial of sulindac, atorvastatin, and prebiotic dietary fiber for colorectal cancer chemoprevention. Cancer Prev Res 4:259–269
Coogan PF, Smith J, Rosenberg L (2007) Statin use and risk of colorectal cancer. J Natl Cancer Inst 99:32–40
Bertagnolli MM, Hsu M, Hawk ET, Eagle CJ, Zauber AG, Adenoma Prevention with Celecoxib Study I (2010) Statin use and colorectal adenoma risk: results from the adenoma prevention with celecoxib trial. Cancer Prev Res 3:588–596
Leufkens AM, Van Duijnhoven FJ, Siersema PD et al (2011) Cigarette smoking and colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition study. Clin Gastroenterol Hepatol 9:137–144
Verla-Tebit E, Lilla C, Hoffmeister M, Brenner H, Chang-Claude J (2006) Cigarette smoking and colorectal cancer risk in Germany: a population-based case–control study. Int J Cancer 119:630–635
Slattery ML, Potter JD, Friedman GD, Ma KN, Edwards S (1997) Tobacco use and colon cancer. Int J Cancer 70:259–264
Weijenberg MP, Aardening PW, de Kok TM, de Goeij AF, van den Brandt PA (2008) Cigarette smoking and KRAS oncogene mutations in sporadic colorectal cancer: results from the Netherlands Cohort Study. Mutat Res 652:54–64
Newcomb PA, Storer BE, Marcus PM (1995) Cigarette smoking in relation to risk of large bowel cancer in women. Cancer Res 55:4906–4909
Corley DA, Jensen CD, Marks AR et al (2014) Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 370:1298–1306
Acknowledgment
This study was supported by National Institutes of Health Grant Number 1R01 CA159976 awarded to Daniel W. Rosenberg, and the State of Connecticut Department of Public Health, Biomedical Research Application Number 2012-0913 awarded to Daniel W. Rosenberg.
Author contributions
David A. Drew, James J. Grady, Helen Swede, Daniel W. Rosenberg, Richard G. Stevens, and Thomas J. Devers were involved in the study concept and design; David A. Drew, Allen Mo, Faripour Forouhar, Gretchen Egan, and Thomas J. Devers were involved in the acquisition of data; David A. Drew, Gyuhyeong Goh, Allen Mo, James J. Grady, Faripour Forouhar, Daniel W. Rosenberg, Richard G. Stevens, and Thomas J. Devers analysed and interpreted the data; David A. Drew, Faripour Forouhar, Daniel W. Rosenberg, and Richard G. Stevens drafted the manuscript; David A. Drew, Gyuhyeong Goh, James J. Grady, Helen Swede, Daniel W. Rosenberg, Richard G. Stevens, and Thomas J. Devers critically revised the manuscript for important intellectual content; David A. Drew, Gyuhyeong Goh, James J. Grady, Helen Swede, and Richard G. Stevens were involved in the statistical analysis; James J. Grady, Daniel W. Rosenberg, Richard G. Stevens, and Thomas J. Devers supervised the study; and Daniel W. Rosenberg funded the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Drew, D.A., Goh, G., Mo, A. et al. Colorectal polyp prevention by daily aspirin use is abrogated among active smokers. Cancer Causes Control 27, 93–103 (2016). https://doi.org/10.1007/s10552-015-0686-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-015-0686-1