Abstract
Purpose
Circadian genes may be involved in regulating cancer-related pathways, including cell proliferation, DNA damage response, and apoptosis. We aimed to assess the role of genetic variation in core circadian rhythm genes with the risk of fatal prostate cancer and first morning void urinary 6-sulfatoxymelatonin levels.
Methods
We used unconditional logistic regression to evaluate the association of 96 single-nucleotide polymorphisms (SNPs) across 12 circadian-related genes with fatal prostate cancer in the AGES-Reykjavik cohort (n = 24 cases), the Health Professionals Follow-Up Study (HPFS) (n = 40 cases), and the Physicians’ Health Study (PHS) (n = 105 cases). We used linear regression to evaluate the association between SNPs and first morning void urinary 6-sulfatoxymelatonin levels in AGES-Reykjavik. We used a kernel machine test to evaluate whether multimarker SNP sets in the pathway (gene based) were associated with our outcomes.
Results
None of the individual SNPs were consistently associated with fatal prostate cancer across the three cohorts. In each cohort, gene-based analyses showed that variation in the CRY1 gene was nominally associated with fatal prostate cancer (p values = 0.01, 0.01, and 0.05 for AGES-Reykjavik, HPFS, and PHS, respectively). In AGES-Reykjavik, SNPs in TIMELESS (four SNPs), NPAS2 (six SNPs), PER3 (two SNPs) and CSNK1E (one SNP) were nominally associated with 6-sulfatoxymelatonin levels.
Conclusion
We did not find a strong and consistent association between variation in core circadian clock genes and fatal prostate cancer risk, but observed nominally significant gene-based associations with fatal prostate cancer and 6-sulfatoxymelatonin levels.

Similar content being viewed by others
References
Fu L, Lee CC (2003) The circadian clock: pacemaker and tumour suppressor. Nat Rev Cancer 3(5):350–361
Zhu Y et al (2009) Testing the circadian gene hypothesis in prostate cancer: a population-based case–control study. Cancer Res 69(24):9315–9322
Davis S, Mirick DK (2006) Circadian disruption, shift work and the risk of cancer: a summary of the evidence and studies in Seattle. Cancer Causes Control 17:539–545
Blask DE (2009) Melatonin, sleep disturbance and cancer risk. Sleep Med Rev 13(4):257–264
Costa G, Haus E, Stevens R (2010) Shift work and cancer—considerations on rationale, mechanisms, and epidemiology. Scand J Work Environ Health 36(2):163–179
Buja A et al (2005) Cancer incidence among male military and civil pilots and flight attendants: an analysis on published data. Toxicol Ind Health 21(10):273–282
Straif K et al (2007) Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol 8(12):1065–1066
Parent ME et al (2012) Night work and the risk of cancer among men. Am J Epidemiol 176(9):751–759
Sigurdardottir LG et al (2014) Urinary melatonin levels, sleep disruption, and risk of prostate cancer in elderly men. Eur Urol. doi:10.1016/j.eururo.2014.07.008
Sigurdardottir LG et al (2012) Circadian disruption, sleep loss, and prostate cancer risk: a systematic review of epidemiologic studies. Cancer Epidemiol Biomarkers Prev 21:1002–1011
Sigurdardottir LG et al (2013) Sleep disruption among older men and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev 22(5):872–879
Kondratov RV, Gorbacheva VY, Antoch MP (2007) The role of mammalian circadian proteins in normal physiology and genotoxic stress responses. Curr Top Dev Biol 78:173–216
Young MW, Kay SA (2001) Time zones: a comparative genetics of circadian clocks. Nat Rev Genet 2(9):702–715
Utge SJ et al (2010) Systematic analysis of circadian genes in a population-based sample reveals association of TIMELESS with depression and sleep disturbance. PLoS One 5(2):e9259
Slominski RM et al (2012) Melatonin membrane receptors in peripheral tissues: distribution and functions. Mol Cell Endocrinol 351(2):152–166
Antoch MP, Kondratov RV, Takahashi JS (2005) Circadian clock genes as modulators of sensitivity to genotoxic stress. Cell Cycle 4(7):901–907
Gauger MA, Sancar A (2005) Cryptochrome, circadian cycle, cell cycle checkpoints, and cancer. Cancer Res 65(15):6828–6834
Borgs L et al (2009) Cell “circadian” cycle: new role for mammalian core clock genes. Cell Cycle 8(6):832–837
Hua H et al (2006) Circadian gene mPer2 overexpression induces cancer cell apoptosis. Cancer Sci 97(7):589–596
DeBruyne JP, Weaver DR, Reppert SM (2007) CLOCK and NPAS2 have overlapping roles in the suprachiasmatic circadian clock. Nat Neurosci 10(5):543–545
Chu LW et al (2008) Variants in circadian genes and prostate cancer risk: a population-based study in China. Prostate Cancer Prostatic Dis 11(4):342–348
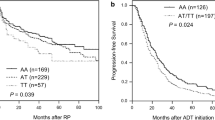
Lin DW et al (2011) Genetic variants in the LEPR, CRY1, RNASEL, IL4, and ARVCF genes are prognostic markers of prostate cancer-specific mortality. Cancer Epidemiol Biomarkers Prev 20(9):1928–1936
Harris TB et al (2007) Age, gene/environment susceptibility-Reykjavik Study: multidisciplinary applied phenomics. Am J Epidemiol 165(9):1076–1087
Giovannucci E et al (2003) Nutritional predictors of insulin-like growth factor I and their relationships to cancer in men. Cancer Epidemiol Biomarkers Prev 12(2):84–89
Schumacher FR et al (2011) Genome-wide association study identifies new prostate cancer susceptibility loci. Hum Mol Genet 20(19):3867–3875
Iceland S (2011) (cited 2014). http://www.statice.is/
Psaty BM et al (2009) Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Consortium Design of Prospective Meta-Analyses of Genome-Wide Association Studies From 5 Cohorts. Circ Cardiovasc Genet 2(1):73–80
Murphy RA et al (2013) Candidate gene association study of BMI-related loci, weight, and adiposity in old age. J Gerontol A Biol Sci Med Sci 68(6):661–666
Nalls MA et al (2011) Multiple loci are associated with white blood cell phenotypes. PLoS Genet 7(6):e1002113. doi:10.1371/journal.pgen.1002113
Li Y et al (2009) Genotype imputation. Annu Rev Genomics Hum Genet 10:387–406
Cochran WG (1954) The combination of estimates from different experiments Biometrics 10:101–129
Evangelou E, Ioannidis JPA (2013) Meta-analysis methods for genome-wide association studies and beyond. Nat Rev Genet 14:379–389
Wu MC et al (2010) Powerful SNP-set analysis for case–control genome-wide association studies. Am J Hum Genet 86(6):929–942
Lin X et al (2011) Kernel machine SNP-set analysis for censored survival outcomes in genome-wide association studies. Genet Epidemiol 35(7):620–631
Kelly MA et al (2012) Circadian gene variants and susceptibility to type 2 diabetes: a pilot study. PLoS One 7(4):e32670. doi:10.1371/journal.pone.0032670
Cao Q et al (2009) A role for the clock gene Per1 in prostate cancer. Cancer Res 69(19):7619–7625
Hoffman AE et al (2008) The circadian gene NPAS2, a putative tumor suppressor, is involved in DNA damage response. Mol Cancer Res 6:1461–1468
Zhu Y et al (2006) Does “clock” matter in prostate cancer? Cancer Epidemiol Biomarkers Prev 15(1):3–5
Carpen JD et al (2005) A single-nucleotide polymorphism in the 5′-untranslated region of the hPER2 gene is associated with diurnal preference. J Sleep Res 14(3):293–297
Evans DS et al (2013) Common genetic variants in ARNTL and NPAS2 and at chromosome 12p13 are associated with objectively measured sleep traits in the elderly. Sleep 36(3):431–446
Duffy JF, Wright KP (2005) Entrainment of the human circadian system by light. J Biol Rhythms 20:326–338
Acknowledgments
We thank the study participants and the Icelandic Heart Association clinic staff for their invaluable contribution. We are grateful to the ongoing participation of men in the Health Professionals Follow-up Study (UM1 CA167552) and would like to acknowledge our colleagues (Lauren McLaughlin and Siobhan Saint-Surin) working on these studies for their valuable help. In addition, we would like to thank the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, and WY. The AGES-Reykjavik is supported by Contract N01-AG-12100 from the National Institutes on Aging Intramural Research Program; Hjartavernd (the Icelandic Heart Association); and the Althingi (the Icelandic Parliament). In addition, this study was supported by funding from the Harvard Catalyst Award, the Icelandic Cancer Society, the National Cancer Institute at the National Institutes of Health (P01 CA055075, CA133891, CA42182, CA34944, CA40360, CA141298, CA98233 and CA097193); the National Heart, Lung, and Blood Institute at the National Institutes of Health (HL26490, HL34595). National Cancer Institute at the National Institutes of Health Training Grant (R25 CA098566 and T32 CA09001-35 to SCM); and the Prostate Cancer Foundation (to LAM and JRR); US Army Department of Defense Prostate Cancer Research Program Fellowship (to IMS). CAC was supported in part by NIH NIA Grant P01-AG-009975.
Conflict of interest
Dr. Czeisler has received consulting fees from or served as a paid member of scientific advisory boards for: Bombardier Inc., Boston Red Sox, Boston Celtics, Cephalon, Inc. (acquired by Teva Pharmaceutical Industries Ltd. October 2011), Michael Jackson’s mother and children, Koninklijke Philips Electronics, N.V., Novartis, United Parcel Service (UPS), Vanda Pharmaceuticals, Inc., and Zeo, Inc; owns an equity interest in Lifetrac, Inc., Somnus Therapeutics, Inc. and Vanda Pharmaceuticals, Inc.; received royalties from McGraw Hill, Penguin Press/Houghton Mifflin Harcourt, and Philips Respironics, Inc.; and has received research support from Cephalon, National Football League Charities, ResMed, and Philips Respironics. Dr. Czeisler is the incumbent of an endowed professorship provided to Harvard University by Cephalon, Inc., holds a number of process patents in the field of sleep/circadian rhythms (e.g., photic resetting of the human circadian pacemaker), and since 1985, has also served as an expert witness on various legal matters related to sleep and/or circadian rhythms.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Markt, S.C., Valdimarsdottir, U.A., Shui, I.M. et al. Circadian clock genes and risk of fatal prostate cancer. Cancer Causes Control 26, 25–33 (2015). https://doi.org/10.1007/s10552-014-0478-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-014-0478-z