Abstract
We quantified associations between IgE and cancer in a meta-analysis and cohort study. Pubmed and Embase were searched to extract information using predefined inclusion criteria. In the Apolipoprotein MOrtality RISk (AMORIS) database, 24,820 persons had IgE measurements. Multivariate Cox proportional hazard models were used to analyze associations between IgE and cancer. Twenty-seven studies were reviewed from which seven case–control studies were included for analysis. The pooled relative risk (random effects model) was 0.97 (95% CI 0.86–1.09). Cell types of tumor origin (mesenchymal tissue or cells of the nervous system, lymphatic or hematopoietic tissue, and epithelium) modified the effect. In the AMORIS cohort, 862 persons developed cancer. Hazard ratios comparing quartiles of IgE were similar to the findings in the meta-analysis (HR 0.87 (95% CI 0.72–1.06); 0.94 (0.78–1.14); 0.90 (0.74–1.10) for the 2nd, 3rd, and 4th quartile compared to the 1st quartile), but there was no pattern by tumor origin. Both studies showed a weak inverse association between IgE and cancer, but a pattern by cancer type was only seen in the meta-analysis. Our findings suggest the need for prospective studies studying IgE and cancer. Measurements of IgE should be combined with other information, e.g., bio-banked samples containing other key immunological discriminators.
Similar content being viewed by others
Introduction
Numerous studies looked into the association between atopy and cancer [1–3]. About 40% of people in Western populations have symptoms of atopy, defined by exaggerated immunoglobulin E (IgE) responses to myriad common environmental allergens [4].
Three distinct perspectives underpin the possible association of atopy with cancer. According to the “antigenic stimulation” hypothesis, atopic inflammation contributes to cancer by causing oxidative damage that activates mutations in tumor suppressor genes or post-translational modifications in proteins involved in DNA repair or apoptotic control [5–7]. Conversely, the “immune surveillance” theory proposes that atopy is a consequence of a generalized enhanced immune responsiveness that has the capability to detect and eradicate dysregulated cells. An inverse association between cancer and allergy is also predicted by the “prophylaxis” hypothesis, by which allergic reactions frequently expel mutagenic toxins, microorganisms and environmental contaminants, promote tissue repair, and encourage behavioral avoidance of irritants and toxins antigens [7]. Nonetheless, reports that allergies associate with either reduced or increased risk of cancer are collectively inconsistent [7–9].
One reason for inconsistency may be the nature of atopy assessment. Self-completed questionnaires and interviews are most commonly used, with some use of skin prick testing and IgE measurement [2, 3]. Vojtechova et al. found in their meta-analysis no evidence for an association between asthma, hay fever, or ‘any allergy’ and cancers of the breast, prostate, or colorectum. They did, however, find a positive association of atopy (assessed by allergen-specific IgE or skin prick testing) with prostate cancer, but only one of the studies included in the meta-analysis used IgE to assess atopy [3]. The use of self-completed questionnaires or interviews to evaluate atopy can be problematic as it may lead to misclassification of exposure and to recall bias. Toren et al. [10] showed that patients with mild asthma are less prone to report it in a questionnaire.
Inconsistent findings might also relate to the fact that atopy influences different tissues in different ways. Since allergies occur primarily at body surfaces, it is logical that inverse relations between allergy and cancer may be more overt for cancers of the corresponding tissues and organ systems (e.g., mouth and throat, lungs, skin) versus sites that do not directly interface with the environment (e.g., prostate, breast, hematopoietic tissue) [7]. Indeed, different types of tissue are more generally associated with different immunological reactions [11–13], which gives a rationale to study cancers by tissue of origin when investigating the association of cancer and atopy.
Thus, we examined the association between IgE measurements and overall cancer as well as subtypes of cancer in a meta-analysis, and in the Swedish Apolipoprotein MOrtality RISk (AMORIS) database, which provided measurements for IgE in a cohort including 862 persons with cancer.
Methods
Meta-analysis
Literature search strategy
We used computerized literature search databases (Pubmed search followed by an Embase search) to identify full text and abstracts published to date. “Immunoglobulin E”, “neoplasms”, and “cancer” were used as search terms. Except for English language and human subjects, no further restrictions were added to the search. Thus, we included “grey literature”, such as letters and abstracts presented in relevant conference meetings. All references of the selected articles were checked so as to validate the completeness of the electronic searches.
Inclusion criteria
The following set of inclusion criteria was used to select the final set of studies: the publication pertained to an epidemiologic study, which measured IgE levels in association with cancer risk; the type of cancer was defined as well as the measurement and cut-off value for IgE; the analytical methods were well described. To include studies of large enough power, only those with at least 20 cancer cases were included. Initially, titles of articles were reviewed in order to ascertain whether they might potentially fit the inclusion criteria. If, after assessing the abstract, there was any doubt over whether it met the relevant criteria, it was subjected to more thorough, subsequent assessment. The list of potential articles was further shortened by performing detailed evaluations of the methods and results of each remaining paper. Figure 1 provides detailed information regarding the progressive ‘flow’ of the study exclusion process.
Data extraction
The following details were recorded for each study: author, year of publication, country where the study was undertaken, IgE levels and measurement methods, study type (case–control or cohort), cancer type, and number of cases and total subjects for each level of IgE.
Meta-analysis statistical techniques
The effect of IgE on cancer risk was evaluated by calculating the random effects summary relative risk to allow for possible heterogeneity between study results. The analyses were conducted for dichotomized values of total IgE, specific IgE, and a combination of both. Since all IgE measurements were dichotomized, a first meta-analysis combined all studies. If a study reported both total and specific IgE, total IgE was used. To verify whether the results differed by type of IgE, sensitivity analyses were conducted in which either total or specific IgE was excluded. The analysis was also stratified by type of cancer based on the tissue in which the cancer originated. The following strata were created based on ICD-7 codes: epithelial tissue (140–180, 190–191, 194–195, 199), lymphatic and hematopoietic tissue (200–209, 198), and mesenchymal tissue and cells from the nervous system (192–193, 196–197). For cancer with origin in mesenchymal tissue and cells from the nervous system, the analysis was based on all studies measuring total IgE, whereas for the other two types of cancer origin, we included studies that measured specific IgE. In order to account for the previously shown association between atopy and lung diseases, a sensitivity analysis was conducted for epithelial cancer excluding lung cancer. Potential heterogeneity of the study results was assessed with a forest plot, which displays the relative risk estimates of cancer risk comparing both levels of IgE, for each study. Potential heterogeneity of the study results was also statistically evaluated using the Q-statistic as well as the I 2 statistic [14]. Effect modification by country and year was assessed by conducting a meta-regression. Potential publication bias was assessed using Begg’s Test and Egger’s funnel plot. All analyses were performed using STATA (version 10).
AMORIS study
Study population and data collection
The AMORIS study (1985–1996), a prospective observational study, contains 351,487 men and 338,101 women, mainly from the greater Stockholm area (Sweden) with age ranging from <20 years to >80 years. The participants were either healthy individuals referred for clinical laboratory testing as part of health checkups or outpatients referred for laboratory testing. All laboratory analyses were done at the CALAB laboratory, Stockholm [15]. No individuals were inpatients at the time their blood samples were taken, and none were excluded from the database for disease symptoms or because of treatment. More than 60% were known to be fasting at the time of blood sampling. A more detailed description of the AMORIS study is given elsewhere [16–19]. The AMORIS database was linked to the Swedish National Cancer Register as well as the Cause of Death Register and the consecutive Swedish Censuses during 1970–1990 by using the Swedish 10-digit personal identity number [20]. Socioeconomic characteristics were obtained from the censuses including socioeconomic status (SES). SES is based on occupational groups and classifies gainfully employed subjects into manual workers and non-manual employees below denoted blue-collar and white-collar workers [21]. The National Cause of Death Register records all deaths in Sweden with date and underlying and contributing causes of death since 1961 and was used to determine vital status [20]. Incident cases of cancer were identified using the Swedish National Cancer Register, which was founded in 1958 and covers the entire Swedish population. According to the law, every case of diagnosed cancer must be notified to the cancer registry by the responsible clinician and also by the pathologist/cytologist [22, 23]. Follow-up was terminated at emigration out of Sweden as recorded in a national register of emigrations.
We used a sub-cohort of all 26,300 persons aged 20 or older, whose levels of IgE were measured at baseline and took the following information from the AMORIS study: IgE (kU/L), age at diagnosis, and gender. The quantitative determination of IgE was done with an ELISA/2-step sandwich assay using a fully automatic immunoassay system ES 700 (Boehringer—Mannheim, Germany) with a coefficient of variation <5%. From the other registries, we collected information regarding SES, cancer diagnosis, and death. Persons diagnosed with benign neoplasms or with a cancer diagnosis prior to their IgE measurements were removed from the sub-cohort (n = 1,480).
Data analysis
Multivariate Cox proportional hazards regression was used to investigate quartiles of IgE (<19.10, 19.10–47.30, 47.30–122.70, >122.70 kU/L) as well as clinical cut-offs of IgE (<25, 25–100, >100 kU/L [24]) in relation to cancer risk. The analysis was conducted for overall cancer and cancer originating in epithelial, lymphatic and hematopoietic, and mesenchymal tissue and in cells from the nervous system. All models took into account age, SES, gender, and seasonality (December–February, March–May, June–August, and September–November). The latter one is defined as the month in which the IgE measurement was taken. The analysis was repeated for quartiles of IgE among persons who had an IgE measurement within the 90th percentile in order to account for the ‘open ending’ of the fourth quartile of IgE in the original analysis. Another sensitivity analysis was conducted in which those who had their IgE measurement taken within 1.5 years prior to cancer diagnosis were deleted. This analysis was undertaken to exclude study subjects where symptoms related to an undiagnosed cancer might have led a person to have her/his blood samples taken and where IgE levels might therefore have been influenced by ongoing disease. Finally, the multivariate Cox proportional hazards regression was also conducted for a dichotomized value of IgE (cut-off 35 kU/L) to compare the results from our cohort study with those from our meta-analysis. All analyses were conducted with Statistical Analysis Systems (SAS) release 9.1.3 (SAS Institute, Cary, NC). This study complied with the Declaration of Helsinki, and the ethics review board of the Karolinska Institute approved the study.
Results
Meta-analysis
The initial search for papers on IgE and cancer risk resulted in 27 articles. After extracting information from the abstracts, seven case–control studies were selected for primary data analysis. Two studies were conducted in Northern America and five in Europe. The major reasons for excluding articles were missing information on methods and statistical analyses (n = 12), and cancer not as an outcome variable in the analysis (n = 6). Six different cancer types (glioma, breast, lung, lymphoma, prostate, and colorectal) were studied in association with IgE, and all cancer diagnoses were histologically confirmed. Three studies reported measurements for total IgE while six reported measurements for specific IgE (Fig. 2; Table 1).
Two important methodological characteristics of the selected case–control studies are the control selection and the IgE collection. Five of seven studies used random controls selected via, for instance, random digit dialing (n = 2) or from general health surveys [24–28]. Two studies used hospital-based controls seen in the hospital for a diagnosis distinct from the cancer outcome of interest [29, 30]. The methods used to measure IgE are described in Table 1. It is also important to know the time at which measurements were conducted in relation to cancer diagnosis: unfortunately, such information is not clearly described for each study. Melbye et al. conducted, in addition to a case–control study, a small prospective cohort study (198 cancers) in which the association between specific IgE seropositivity and risk of non-Hodgkin lymphoma was analyzed by time between IgE measurement and cancer diagnosis. The shorter the time interval, the more protective was the association, although none of the findings was statistically significant [26].
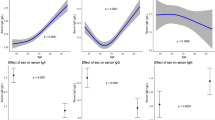
The random effects analysis, comparing overall cancer risk and IgE exposure status (total and specific combined), showed a pooled effects relative risk of 0.97 (95% CI 0.86–1.09). The Q-statistic and I 2 statistic suggested heterogeneity (Q = 31.26; df = 9; p < 0.001; I 2 = 71.2%), which can also be observed in the corresponding forest plot (Fig. 2a). A sensitivity analysis in which we only studied the association between specific IgE exposure status and overall cancer resulted in a pooled relative risk of 1.02 (95% CI 0.87–1.19). The pooled relative risk was 0.86 (95% CI 0.71–1.05) when only studying the association between total IgE and cancer. Meta-regression analysis did not show any effect modification by year or country. Egger’s funnel plot showed a symmetric spread of the studies indicating that there was no publication bias (Fig. 3).
When grouping cancer sites, we observed a protective effect of total IgE for cancers with origin in mesenchymal tissue or cells of the nervous system (pooled RR 0.80; 95% CI 0.70–0.91) and a protective effect of specific IgE for cancer with origin in lymphatic and hematopoietic tissue (pooled RR 0.82; 95% CI 0.70–0.95) (Fig. 2b, c). An increased risk was seen for those cancers with origin in epithelial tissue when combining the studies on specific IgE (pooled RR 1.14; 95% CI 1.02–1.27) (Fig. 2d).
AMORIS study
A total of 862 persons developed cancer during follow-up time, from which 767 developed a cancer of epithelial origin, 62 a cancer with lymphatic or haematological origin, and 33 a cancer originating in mesenchymal tissue and cells of the nervous system. Most cancers developed in women (62.2%), which is likely attributable to the age structure of the cohort and the ensuing distribution of cancer types: about 34% of female cancers were malignant neoplasia of breast and genital organs. The age distribution of this study cohort is young (mean age of 41) compared to the total Swedish population since most measurements were taken as part of health examinations done at company health checkups (Table 2).
Multivariate Cox regression (adjusted for SES, age, and gender) for the association between quartiles of IgE and overall cancer diagnosis showed associations that deviated modestly from unity. However, for overall cancer, the estimates were consistently below one, albeit not significant (Table 3). Similar results were found when using clinical cut-offs of IgE (Table 4). When grouping cancer sites, we observed a weak protective effect for cancers originating in epithelial tissue, but did not find any consistent pattern for cancers with origin in lymphatic or hematopoietic tissue or mesenchymal tissue and cells of the nervous system. An analog analysis for those with an IgE measurement within the 90th percentile did not show other findings (results not shown); nor did the sensitivity analysis in which we excluded those who had their IgE measurements within 1.5 years prior to their cancer diagnosis (Tables 3, 4). An extension of the exclusion period to 5 years did not alter the findings (results not shown).
To compare our findings with the meta-analyses, we repeated the analyses using a dichotomized variable for IgE. The HR for overall cancer was 0.97 (95% CI 0.85–1.11), and the HRs for the different cancer types were 0.98 (95% CI 0.85–1.13), 0.94 (95% CI 0.57–1.56), and 0.89 (95% CI 0.45–1.78) for cancer with origin in epithelial tissue, lymphatic and hematopoietic tissue, and mesenchymal tissue and cells from the nervous system, respectively.
Discussion
There are few comprehensive studies of association between IgE and cancer risk. This report presents both the first meta-analysis and the first large prospective cohort study investigating this association. Both the meta-analysis and the cohort study show a weak negative association between IgE and overall cancer risk, albeit not statistically significant. For cancers with origin in epithelium, the meta-analysis showed a positive association, whereas the prospective cohort study showed a negative effect.
Most studies on allergies and atopy and cancer have used physicians’ physical examinations or self-reports to health care professionals [7, 8, 31]. Most were case–control studies and assessed allergy histories retrospectively, which may lead to misclassification of exposure dependent on case status, i.e., recall bias. Moreover, high levels of IgE and atopy do not always correlate with clinically recognized allergies, placing qualifications of any equivalence of IgE and recounted history of allergy. To better define the association between atopy and cancer, some recent studies have analyzed the association between IgE levels and cancer diagnosis [24–30], although all such studies were also case–control studies in which the validity is much dependent on the method of selection controls [8, 27]. As a consequence of the case–control design, all IgE measurements were taken after tumor diagnosis and only two studies reported IgE measurements taken before treatment initiation [26, 30]. This is of importance as several cancer treatments have been suggested to increase IgE concentrations. Wiemels et al. showed that temozolomide, a common treatment for glioma, may influence IgE levels in relation to glioma risk [24, 28]. Supporting evidence was also observed in natural killer cell-depleted mice: whole-body radiation was correlated with elevated IgE production [32]. Hence, our prospective cohort study, with IgE measurements prior to tumor development, adds value to the existing literature on IgE and cancer.
Paradoxically, the growing interest in IgE and cancer is based on diametrically opposed perspectives about atopy and the action of IgE. For example, atopy may be interpreted to reflect a generalized immune hyperresponsiveness immune response that enhances natural immunosurveillance. Indeed, IgE is a product of Th2 responses that are promoted in tissues by the cytokine, “Thymic Stromal Lymphopoietin” (TSLP), released by “stressed” epithelial cells. Hence, high IgE may reflect a natural activation of immune-surveillance mechanisms, possibly promoted by cancers undiagnosed at the time of sampling. IgE has the capacity to recognize overexpressed tumor antigens and to then mobilize the cytotoxic effector functions of mast cells, eosinophils, and basophiles following binding to the Fcε-receptor [1]. This was demonstrated by Karagiannis et al. [33] in the context of human ovarian carcinoma xenografts. Likewise, a positive association between natural killer (NK) cell activity and serum IgE was reported in 66 healthy non-allergic males [34]. Overall, this perspective seems consistent with the findings in the meta-analysis of a protective effect of high IgE levels for lymphatic and hematopoietic cancers as well as mesenchymal and neural cancers. It is also consistent with proposals to employ tumor-specific IgE in experimental immunotherapy. However, challenging this standpoint are claims that when armed with a tumor-specific IgE antibody, effector cells from atopic individuals are less tumoricidal than effectors from non-atopic individuals, perhaps because their Fcε receptors are pre-bound by high levels of allergen-specific IgE [35].
An alternative perspective is that high IgE does not reflect generalized hyperimmune responsiveness, but rather an inappropriate skewing toward Th2 responses. Since signatory Th2 cytokines, such as IL-4 and IL-13, suppress interferon-γ (IFNγ)-associated inflammatory Th1 and cytolytic responses, atopy would be predicted to segregate positively with cancer, particularly in epithelial tissues where atopy is locally active. Some evidence for this was apparent in the weak positive effect observed for epithelial cancers. Challenging this standpoint, however, is the concept that inflammation promotes tissue disruption, re-organization, and re-vascularization that may collectively promote tumor cell growth and dissemination [11, 12]. By this perspective, the suppression of an inflammatory Th1 response might be beneficial. In short, there are many reasons to investigate IgE and cancer, but the current knowledge of human immunology is simply insufficient to predict whether high IgE should positively or negatively correlate with cancers in different tissues.
Clearly, positive and negative associations of IgE with specific cancer types might be attributed to any of the aforementioned immunological considerations, and one might even propose that the capacity for Th2 responses to simultaneously promote and suppress natural surveillance will inevitably lead to inconsistent association data. Moreover, yet other factors may be germane, for example to the negative association between IgE and cancers of mesenchymal or neural origin. As suggested by Wiemels et al, high IgE levels may reflect another factor that reduces these types of cancer, but does not affect (or even increases) cancer risk within epithelia [24].
Despite this statistically significant pattern by cancer origin in the meta-analysis, the results need to be interpreted carefully as there are several study limitations. Few studies were included and when stratifying by tissue of origin, the analysis was sometimes limited to findings from a small group of researchers. The assessment of IgE is subject to measurement error and misclassification. Dichotomization of IgE exposure (high vs. low), for example, could lead to substantial variations in exposure levels for “high”. Unfortunately, it was not possible in this meta-analysis to use dose-response data as the number of relevant studies available to date was small and the qualitative classifications of IgE varied. In addition, assessment of IgE levels can vary substantially between studies. Between-laboratory variation is apparent because different assays and methods of internal control were used. There was also only one measurement of IgE used per person, which could result in within-person variation. Repeated measurement could have provided a more stable estimate in order to prevent influence from seasonality. Moreover, IgE levels could be influenced by ongoing cancer treatments. It is unlikely that there is a lot of misclassification for the cancer outcomes as all cancers have been histologically confirmed. There might have been residual confounding from possible unmeasured or measured lifestyle factors that differ between atopic and non-atopic persons. For example, those with respiratory or gut allergies may have distinctly different consumption and/or adsorption levels of toxins [27]. Some of the case–control studies used random digit dialing to select controls and some used hospital-based control series; both methods imply that the control series are not necessarily fully representative of the study base that gives rise to the cases, and these designs are therefore sensitive to selection bias.
Given the limitations of the case–control studies included in the meta-analysis, it was of interest to study the association between IgE and cancer in a prospective cohort study. Our findings in the AMORIS sub-cohort also showed a weak trend by quartiles of IgE for overall cancer, but did not show a pattern by cancer type. This lack of a pattern by type of origin could be explained by the small number of cancers in each subgroup. However, our prospective data could also have less inherent bias than the case–control data in the meta-analysis and reflect a true lack of an association by tumor type. Furthermore, the time between IgE measurement and cancer diagnosis might have played a role in the case–control studies as undiagnosed cancers could have already affected IgE levels, as outlined earlier. In this study, the mean time between IgE measurement and cancer diagnosis was 4.5 years (SD 2.7). It is unclear what the mean time between cancer diagnosis and IgE measurement was in the studies included in the meta-analysis.
For the meta-analysis, we made all possible efforts to include all relevant publications available to date through various sources, including grey literature, and the two main online databases (PubMed and Embase). In addition, clearly defined objective criteria for exposure, outcome, and other study characteristics were specified a priori. Publication bias is unlikely to be an issue as about half of the studies included reported non-significant results [25, 27, 28].
The major strength of this analysis is the large number of persons with prospective measurements of IgE in AMORIS, all measured at the same clinical laboratory. Use of national health registers provided complete follow-up for each person as well as detailed information on cancer diagnosis, time of death, and emigration. Furthermore, assessment of both exposure (IgE measurement) and outcome (cancer) was conducted in an accurate manner. The AMORIS population was selected by analyzing blood samples from health checkups in non-hospitalized individuals. During the study period, the all-cause mortality was about 14% lower in the AMORIS population than in the general population of Stockholm County when taking age, gender, and calendar year into account [36]. Nevertheless, this healthy cohort effect would not affect the internal validity of our study, and it is also likely to be minor since it has been shown that the AMORIS cohort is similar to the general working population of Stockholm County in terms of SES and ethnicity. There were no repeated measurements for IgE available nor was there information on possible other confounders such as smoking habits.
Conclusions
Both our meta-analysis and cohort study showed a weak negative association between IgE and cancer, but in contrast to the meta-analysis, the findings in the cohort study did not show a pattern by cancer type. This contradiction might be explained by a less inherent bias in prospective data than in case–control data in the meta-analysis, reflecting a true lack of an association by tumor type. Given the current knowledge about IgE and cancer, there are compelling reasons to continue to investigate this association. Our findings suggest that prospective studies might be more appropriate, but only if any future assessments of IgE are undertaken in the context of other immunological markers such as cytokines and effector cell capabilities. In this way, the IgE status can be related either to generalized hyperimmune responsiveness or to specific Th2-skewing. By careful assessment of atopy and allergy, it may also be possible to determine whether high IgE levels are in part attributable to epithelial release of TSLP prompted by genotoxic stress during tumor formation.
References
Jensen-Jarolim E, Achatz G, Turner MC et al (2008) AllergoOncology: the role of IgE-mediated allergy in cancer. Allergy 63:1255–1266
Linos E, Raine T, Alonso A, Michaud D (2007) Atopy and risk of brain tumors: a meta-analysis. J Natl Cancer Inst 99:1544–1550
Vojtechova P, Martin RM (2009) The association of atopic diseases with breast, prostate, and colorectal cancers: a meta-analysis. Cancer Causes Control
Janeway C, Travers P, Walport M, Shlomchik M (2001) Allergy and hypersensitivity. Immunobiology 5: the immune system in health and disease, 5th edn. Garland Publishing, New York
Heikkila K, Harris R, Lowe G et al (2008) Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes Control
Siemes C, Visser LE, Coebergh JW et al (2006) C-reactive protein levels, variation in the C-reactive protein gene, and cancer risk: the Rotterdam Study. J Clin Oncol 24:5216–5222
Sherman PW, Holland E, Sherman JS (2008) Allergies: their role in cancer prevention. Q Rev Biol 83:339–362
Turner MC, Chen Y, Krewski D, Ghadirian P (2006) An overview of the association between allergy and cancer. Int J Cancer 118:3124–3132
Morgan GJ, Linet MS, Rabkin CS (2006) Immunologic factors. In: Schottenfeld DF, Fraumeni J (eds) Cancer epidemiology and prevention, 3rd edn. Oxford University Press, Oxford
Toren K, Palmqvist M, Lowhagen O, Balder B, Tunsater A (2006) Self-reported asthma was biased in relation to disease severity while reported year of asthma onset was accurate. J Clin Epidemiol 59:90–93
DeNardo DG, Coussens LM (2007) Inflammation and breast cancer. Balancing immune response: crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res 9:212
Martinez FO, Sica A, Mantovani A, Locati M (2008) Macrophage activation and polarization. Front Biosci 13:453–461
Hayday AC (2009) Gammadelta T cells and the lymphoid stress-surveillance response. Immunity 31:184–196
Deeks J, Altman D, Bradburn M (2001) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith G, Altman D (eds) Systematic reviews in health care: meta-analysis in context. TJ International Ltd, Padstow
Jungner I, Marcovina SM, Walldius G, Holme I, Kolar W, Steiner E (1998) Apolipoprotein B and A-I values in 147576 Swedish males and females, standardized according to the World Health Organization-International Federation of Clinical Chemistry First International Reference Materials. Clin Chem 44:1641–1649
Walldius G, Jungner I, Holme I, Aastveit AH, Kolar W, Steiner E (2001) High apolipoprotein B, low apolipoprotein A-I and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. Lancet 358:2026–2033
Holme I, Aastveit AH, Jungner I, Walldius G (2008) Relationships between lipoprotein components and risk of myocardial infarction: age, gender and short versus longer follow-up periods in the Apolipoprotein MOrtality RISk study (AMORIS). J Intern Med 264:30–38
Holme I, Aastveit AH, Hammar N, Jungner I, Walldius G (2009) Relationships between lipoprotein components and risk of ischaemic and haemorrhagic stroke in the Apolipoprotein MOrtality RISk study (AMORIS). J Intern Med 265:275–287
Walldius G, Jungner I, Kolar W, Holme I, Steiner E (1992) High cholesterol and triglyceride values in Swedish males and females: increased risk of fatal myocardial infarction. First report from the AMORIS (Apolipoprotein related MOrtality RISk) study. Blood Press Suppl 4:35–42
The National Board of Health and Welfare (2007) Statistics in the areas of health and medical care
Central Bureau for Statistics (2008) Statistics Sweden [cited; Available from: http://www.scb.se/]
Mattsson B, Wallgren A (1984) Completeness of the Swedish Cancer Register. Non-notified cancer cases recorded on death certificates in 1978. Acta Radiol Oncol 23:305–313
The National Board of Health and Welfare (2008) The Swedish cancer registry
Wiemels JL, Wiencke JK, Patoka J et al (2004) Reduced immunoglobulin E and allergy among adults with glioma compared with controls. Cancer Res 64:8468–8473
Hallgren R, Arrendal H, Hiesche K, Lundquist G, Nou E, Zetterstrom O (1981) Elevated serum immunoglobulin E in bronchial carcinoma: its relation to the histology and prognosis of the cancer. J Allergy Clin Immunol 67:398–406
Melbye M, Smedby KE, Lehtinen T et al (2007) Atopy and risk of non-Hodgkin lymphoma. J Natl Cancer Inst 99:158–166
Wang H, Rothenbacher D, Low M, Stegmaier C, Brenner H, Diepgen TL (2006) Atopic diseases, immunoglobulin E and risk of cancer of the prostate, breast, lung and colorectum. Int J Cancer 119:695–701
Wiemels JL, Wilson D, Patil C et al (2009) IgE, allergy, and risk of glioma: update from the San Francisco Bay Area Adult Glioma Study in the temozolomide era. Int J Cancer 125:680–687
Ellison-Loschmann L, Benavente Y, Douwes J et al (2007) Immunoglobulin E levels and risk of lymphoma in a case–control study in Spain. Cancer Epidemiol Biomarkers Prev 16:1492–1498
Petridou ET, Chavelas C, Dikalioti SK et al (2007) Breast cancer risk in relation to most prevalent IgE specific antibodies: a case control study in Greece. Anticancer Res 27:1709–1713
Wang H, Diepgen TL (2005) Is atopy a protective or a risk factor for cancer? A review of epidemiological studies. Allergy 60:1098–1111
Park HR, Jung U, Jo SK (2007) Impairment of natural killer (NK) cells is an important factor in a weak Th1-like response in irradiated mice. Radiat Res 168:446–452
Karagiannis SN, Bracher MG, Hunt J et al (2007) IgE-antibody-dependent immunotherapy of solid tumors: cytotoxic and phagocytic mechanisms of eradication of ovarian cancer cells. J Immunol 179:2832–2843
Kusaka Y, Sato K, Zhang Q, Morita A, Kasahara T, Yanagihara Y (1997) Association of natural killer cell activity with serum IgE. Int Arch Allergy Immunol 112:331–335
Karagiannis SN, Wang Q, East N et al (2003) Activity of human monocytes in IgE antibody-dependent surveillance and killing of ovarian tumor cells. Eur J Immunol 33:1030–1040
Holzmann M, Jungner I, Walldius G, Ivert I, Nordqvist T, östergren J (2008) Apolipoproteins B and A-I, standard lipid measures and incidence of myocardial infarction in men and women, with or without chronic kidney disease. Study IV in Thesis for doctorial degree (PhD). In: Holzmann M (ed) Renal insufficiency, mortality and myocardial infarction. Karolinska Institutet, Stockholm
Acknowledgments
The authors would like to thank Dr. Sarah Rudman for her inspiring talk on IgE and cancer risk. The study was supported by grants from the Gunnar and Ingmar Jungner Foundation for Laboratory Medicine (Stockholm), Cancer Research-UK, and the University of London Central Research Fund. The authors also acknowledge financial support from the Department of Health via the National Institute for Health Research (NIHR) comprehensive Biomedical Research Centre award to Guy’s, and St Thomas’ NHS Foundation Trust in partnership with King’s College London and King’s College Hospital NHS Foundation Trust.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Hemelrijck, M., Garmo, H., Binda, E. et al. Immunoglobulin E and cancer: a meta-analysis and a large Swedish cohort study. Cancer Causes Control 21, 1657–1667 (2010). https://doi.org/10.1007/s10552-010-9594-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-010-9594-6