Abstract
Background
Recent studies have suggested that a significant proportion of patients with axillary nodal metastases diagnosed by pre-operative axillary ultrasound (AUS)-guided needle biopsy were over-treated with axillary lymph node dissection (ALND). The role of routine AUS and needle biopsy in early breast cancer was questioned. This review aims to determine if pre-operative AUS could predict the extent of axillary tumor burden and need of ALND.
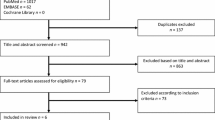
Methods
PubMed and Embase literature databases were searched systematically for abnormal AUS characteristics and axillary nodal burden. Studies were eligible if they correlated the sonographic abnormalities in AUS with the resultant axillary nodal burden in ALND according to the ACOSOG Z0011 criteria.
Results
Eleven retrospective studies and one prospective study with 1658 patients were included. Sixty-five percent of patients with one abnormal lymph node in AUS and 56% of those with two had low axillary nodal burden. Using one abnormal lymph node as the cut-off, the pooled sensitivity and specificity in prediction of axillary nodal burden were 66% (95%CI 63–69%) and 73% (95% CI 70–76%), respectively. Across the six studies that evaluated suspicious nodal characteristics, increased nodal cortical thickness may be associated with high axillary nodal burden.
Conclusion
More than half of the patients with pre-operative positive AUS and biopsy proven axillary nodal metastases were over-treated by ALND. Quantification of suspicious nodes and extent of cortical morphological changes in AUS may help identify suitable patients for sentinel lymph node biopsy.



Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
References
Galimberti V, Cole BF, Viale G, Veronesi P, Vicini E, Intra M, Mazzarol G, Massarut S, Zgajnar J, Taffurelli M, Littlejohn D, Knauer M, Tondini C, Di Leo A, Colleoni M, Regan MM, Coates AS, Gelber RD, Goldhirsch A (2018) International breast cancer study group trial 23–01. Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23–01): 10-year follow-up of a randomised, controlled phase 3 trial. Lancet Oncol Oct 19(10):1385–1393
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, McCall LM, Morrow M (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305(6):569–575
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, Ollila DW, Hansen NM, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Morrow M (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (alliance) randomized clinical trial. JAMA 318(10):918–926
Fillion MM, Glass KE, Hayek J, Wehr A, Phillips G, Terando A, Agnese DM (2017) Healthcare costs reduced after incorporating the results of the American college of surgeons oncology group Z0011 trial into clinical practice. Breast J 23(3):275–281
Ngui NK, Hitos K, Hughes TMD (2019) Effect of the American college of surgeons oncology group Z0011 trial on axillary management in breast cancer patients in the Australian setting. Breast J 25(5):853–858
Caudle AS, Kuerer HM, Le-Petross HT, Yang W, Yi M, Bedrosian I, Krishnamurthy S, Fornage BD, Hunt KK, Mittendorf EA (2014) Predicting the extent of nodal disease in early-stage breast cancer. Ann Surg Oncol 21(11):3440–3447
Verheuvel NC, Ooms HW, Tjan-Heijnen VC, Roumen RM, Voogd AC (2016) Predictors for extensive nodal involvement in breast cancer patients with axillary lymph node metastases. Breast 27:175–181
Boland MR, Ni Cearbhaill R, Fitzpatrick K, Walsh SM, Evoy D, Geraghty J, Rothwell J, McNally S, O’Doherty A, Quinn CM, McDermott EW, Prichard RS (2016) A positive node on ultrasound-guided fine needle aspiration predicts higher nodal burden than a positive sentinel lymph node biopsy in breast carcinoma. World J Surg 40(9):2157–2162
Verheuvel NC, Voogd AC, Tjan-Heijnen VCG, Siesling S, Roumen RMH (2017) Different outcome in node-positive breast cancer patients found by axillary ultrasound or sentinel node procedure. Breast Cancer Res Treat 165(3):555–563
Ahmed M, Jozsa F, Baker R, Rubio IT, Benson J, Douek M (2017) Meta-analysis of tumour burden in pre-operative axillary ultrasound positive and negative breast cancer patients. Breast Cancer Res Treat 166(2):329–336
Liu M, Yang Y, Xie F, Guo J, Wang S, Yang H, Wang S (2019) Could axillary clearance be avoided in clinically node-negative breast cancer patients with positive nodes diagnosed by ultrasound guided biopsy in the post-ACOSOG Z0011 era? PLoS ONE 14(1):e0210437
Syed A, Eleti S, Eletiet A (2018) Role of axillary ultrasound in the evaluation of early breast cancer in the era of Z0011: time to redefine? Med Res J 3(2):82–88
Pilewskie M, Mautner SK, Stempel M, Eaton A, Morrow M (2016) Does a positive axillary lymph node needle biopsy result predict the need for an axillary lymph node dissection in clinically node-negative breast cancer patients in the ACOSOG Z0011 era? Ann Surg Oncol 23:1123–1128
Boland MR, Prichard RS, Daskalova I, Lowery AJ, Evoy D, Geraghty J et al (2015) Axillary nodal burden in primary breast cancer patients with positive pre-operative ultrasound guided fine needle aspiration cytology: management in the era of ACOSOG Z011. Eur J Surg Oncol 41:559–565
Whiting PF, Rutjes AW, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536
Zamora J, Abraira V, Muriel A et al (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol. https://doi.org/10.1186/1471-2288-6-31
Farrell TP, Adams NC, Stenson M, Carroll PA, Griffin M, Connolly EM, O’Keeffe SA (2015) The Z0011 trial: is this the end of axillary ultrasound in the pre-operative assessment of breast cancer patients? Eur Radiol 25(9):2682–2687
Gálvez MM, Jiménez JA, Gil Izquierdo JI, Alcaraz AC, Benito AC, González LC, Ortiz GP, Funes DF, Aguayo Albasini JL, Ayala de la Peña F (2020) Ultrasound staging in breast cancer: a decision-making oriented approach to axillary metastatic burden prediction. Surg Oncol 35:114–119
Yi CB, Ding ZY, Deng J, Ye XH, Chen L, Zong M, Li CY (2020) Combining the ultrasound features of primary tumor and axillary lymph nodes can reduce false-negative rate during the prediction of high axillary node burden in BI-RADS category 4 or 5 breast cancer lesions. Ultrasound Med Biol 46(8):1941–1948
Hieken TJ, Trull BC, Boughey JC, Jones KN, Reynolds CA, Shah SS, Glazebrook KN (2013) Preoperative axillary imaging with percutaneous lymph node biopsy is valuable in the contemporary management of patients with breast cancer. Surgery 154(4):831–838
Nicolau P, Gamero R, Rodríguez-Arana A, Plancarte F, Alcántara R, Carreras R, Sabadell D, Vernet-Tomas M (2018) Imaging and pathology features to predict axillary tumor load in breast cancer. J Obstet Gynaecol Res 44(2):331–336
Zhu Y, Zhou W, Jia XH, Huang O, Zhan WW (2018) Preoperative axillary ultrasound in the selection of patients with a heavy axillary tumor burden in early-stage breast cancer: what leads to false-positive results? J Ultrasound Med 37(6):1357–1365
Harris CK, Tran HT, Lee K, Mylander C, Pack D, Rosman M, Tafra L, Umbricht CB, Andrade R, Liang W, Jackson RS (2017) Positive ultrasound-guided lymph node needle biopsy in breast cancer may not mandate axillary lymph node dissection. Ann Surg Oncol 24(10):3004–3010
Lim GH, Upadhyaya VS, Acosta HA, Lim JMA, Allen JC Jr, Leong LCH (2018) Preoperative predictors of high and low axillary nodal burden in Z0011 eligible breast cancer patients with a positive lymph node needle biopsy result. Eur J Surg Oncol 44(7):945–950
Del Riego J, Diaz-Ruiz MJ, Teixidó M, Ribé J, Vilagran M, Canales L, Sentís M, Grup de Mama Vallès-Osona-Bages (GMVOB) (2018) The impact of axillary ultrasound with biopsy in overtreatment of early breast cancer. Eur J Radiol 98:158–164
Kim WH, Kim HJ, Lee SM, Cho SH, Shin KM, Lee SY, Lim JK (2019) Prediction of high nodal burden with ultrasound and magnetic resonance imaging in clinically node-negative breast cancer patients. Cancer Imaging 19(1):4
Wang X, Chen L, Sun Y, Zhang B (2020) Evaluation of axillary lymph node metastasis burden by preoperative ultrasound in early-stage breast cancer with needle biopsy-proven metastasis. Clin Transl Oncol 22(4):468–473
Yoo TK, Kang BJ, Kim SH, Song BJ, Ahn J, Park WC, Chae BJ (2020) Axillary lymph node dissection is not obligatory in breast cancer patients with biopsy-proven axillary lymph node metastasis. Breast Cancer Res Treat 181(2):403–409
Puri S, Sharma N, Newcombe RG, Kaushik M, Al-Attar M, Pascaline S, Hajaj M, Wallis MG, Elsberger B, Goyal A (2018) Axillary tumour burden in women with one abnormal node on ultrasound compared to women with multiple abnormal nodes. Clin Radiol 73(4):391–395
Verheuvel NC, van den Hoven I, Ooms HW, Voogd AC, Roumen RM (2015) The role of ultrasound-guided lymph node biopsy in axillary staging of invasive breast cancer in the post-ACOSOG Z0011 trial era. Ann Surg Oncol 22(2):409–415
Boone BA, Huynh C, Spangler ML, Sumkin J, Johnson R, McGuire KP, Soran A, Ahrendt GM (2015) Axillary lymph node burden in invasive breast cancer: a comparison of the predictive value of ultrasound-guided needle biopsy and sentinel lymph node biopsy. Clin Breast Cancer 15(5):e243–e248
Farshid G, Kollias J, Grantley GP (2015) The clinical utility of assessment of the axilla in women with suspicious screen detected breast lesions in the post Z0011 era. Breast Cancer Res Treat 151(2):347–355
Alvarez S, Añorbe E, Alcorta P, López F, Alonso I, Cortés J (2006) Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol 186(5):1342–1348
Houssami N, Ciatto S, Turner RM, Cody HS 3rd, Macaskill P (2011) Preoperative ultrasound-guided needle biopsy of axillary nodes in invasive breast cancer: meta-analysis of its accuracy and utility in staging the axilla. Ann Surg 254(2):243–251
Kramer GM, Leenders MW, Schijf LJ, Go HL, van der Ploeg T, van den Tol MP, Schreurs WH (2016) Is ultrasound-guided fine-needle aspiration cytology of adequate value in detecting breast cancer patients with three or more positive axillary lymph nodes? Breast Cancer Res Treat 156(2):271–278
National collaborating centre for cancer (UK). Early and locally advanced breast cancer: diagnosis and treatment [internet]. Cardiff (UK): national collaborating centre for cancer (UK); 2009 Feb. (NICE clinical guidelines, No. 80.) available from: https://www.ncbi.nlm.nih.gov/books/NBK11643/
Luo H, Mo Y, Zhong J, Zhang Y, Zhu L, Shi X, Chen Y (2020) Preoperative axillary ultrasound helps in the identification of a limited nodal burden in breast cancer patients. Ultrasound Q 36(2):173–178
Cools-Lartigue J, Meterissian S (2012) Accuracy of axillary ultrasound in the diagnosis of nodal metastasis in invasive breast cancer: a review. World J Surg 36(1):46–54
Cooper KL, Harnan S, Meng Y, Ward SE, Fitzgerald P, Papaioannou D, Wyld L, Ingram C, Wilkinson ID, Lorenz E (2011) Positron emission tomography (PET) for assessment of axillary lymph node status in early breast cancer: a systematic review and meta-analysis. Eur J Surg Oncol 37(3):187–198
Liberale V, Rosso R, Arisio R, D’Alonzo M, Villasco A, Fuso L, De Sanctis C, Modaffari P, Biglia N (2020) Axillary dissection in patients with preoperative positive nodal cytology: genuine need or overtreatment? Breast J 26(2):168–175
Amonkar SJ, Oates E, McLean L, Nicholson S (2013) Pre-operative staging of the axilla in primary breast cancer. By redefining the abnormal appearing node can we reduce investigations without affecting overall treatment? Breast 22(6):1114–1118
Gao Y, Luo Y, Zhao C, Xiao M, Ma L, Li W, Qin J, Zhu Q, Jiang Y (2021) Nomogram based on radiomics analysis of primary breast cancer ultrasound images: prediction of axillary lymph node tumor burden in patients. Eur Radiol 31(2):928–937
Funding
The authors received no funding for this study and there is no conflict of interest for disclosure.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have completed the ICMJE uniform disclosure form. The authors received no funding for this study and there is no conflict of interest for disclosure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Man, V., Luk, WP., Fung, LH. et al. The role of pre-operative axillary ultrasound in assessment of axillary tumor burden in breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat 196, 245–254 (2022). https://doi.org/10.1007/s10549-022-06699-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06699-w